Claire Magone, Michaël Neuman & Fabrice Weissman
Head of Communications, Médecins Sans Frontières - Operational Centre Paris (OCP)
After studying communication (CELSA) and political sciences (La Sorbonne), Claire Magone worked for various NGOs, particularly in Africa (Liberia, Sierra Leone, Sudan, Nigeria). In 2010, she joined MSF-Crash as a Director of Studies. Since 2014, she has been working as a Head of Communications.

Director of studies at Crash / Médecins sans Frontières, Michaël Neuman graduated in Contemporary History and International Relations (University Paris-I). He joined Médecins sans Frontières in 1999 and has worked both on the ground (Balkans, Sudan, Caucasus, West Africa) and in headquarters (New York, Paris as deputy director responsible for programmes). He has also carried out research on issues of immigration and geopolitics. He is co-editor of "Humanitarian negotiations Revealed, the MSF experience" (London: Hurst and Co, 2011). He is also the co-editor of "Saving lives and staying alive. Humanitarian Security in the Age of Risk Management" (London: Hurst and Co, 2016).

A political scientist by training, Fabrice Weissman joined Médecins sans Frontières in 1995. First as a logistician, then as project coordinator and head of mission, he has worked in many countries in conflict (Sudan, Ethiopia, Eritrea, Kosovo, Sri Lanka, etc.) and more recently in Malawi in response to natural disasters. He is the author of several articles and collective works on humanitarian action, including "In the Shadow of Just Wars. Violence, Politics and Humanitarian Action" (ed., London, Hurst & Co., 2004), "Humanitarian Negotiations Revealed. The MSF Experience" (ed., Oxford University Press, 2011) and "Saving Lives and Staying Alive. Humanitarian Security in the Age of Risk Management" (ed., London, Hurst & Co, 2016). He is also one of the main hosts of the podcast La zone critique.
I. Stories
Sri Lanka. Amid All-out War
Fabrice Weissman
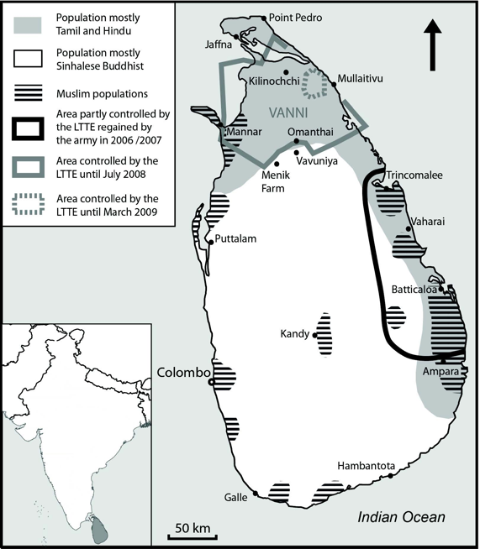
On 18 May 2009, the Sri Lankan government’s crushing victory over the Liberation Tigers of Tamil Eelam (LTTE) put an end to twenty-six years of civil war. Described by the government as the world’s largest humanitarian operation, the victorious Colombo offensive was praised as a model by many foreign military commentatorsCf. for example, V.K. Shashikumar, “Lessons from the War in Sri Lanka”, Indian Defence Review, 24, no. 3 (July–Sept. 2009); Lawrence Hart, “The option no one wants to think about”, The Jerusalem Post, 9 Dec. 2009. keen to demonstrate that a determined democratic army could vanquish a “terrorist” movement. In reality, victory came at the price of thousands of civilian deaths, and the enlisting of humanitarian organisations into a counterinsurgency strategy based on forced displacements and internment. MSF’s experience reveals the hard choices that all-out war imposes on aid organisations.
MSF withdrew from Sri Lanka in 2003, after working for seventeen years against a background of civil war between the government and the LTTE that began in the mid-1980s. A ceasefire agreement (CFA) was signed a year before MSF’s departure, leading to a return to relative normality and the hope of peace. Negotiations began under the copresidency of the European Union, the USA and other western countries, including Norway, which also headed a ceasefire observation mission, the Sri Lanka Monitoring Mission (SLMM).
As early as 2003, the discussions stalled on the key question raised by the conflict: how to ensure peaceful coexistence between the Sinhalese, Tamil and Muslim communities, representing 75%, 17% and 8% respectively of the island’s population. Although the parties did undertake to explore a federal solution to the conflict, talks became acrimonious once they got down to specifics or tried to agree on a transitional administration for the rebel areas (a third of Sri Lankan territory).Eric Meyer and Eleanor Pavey, “Bons offices, surveillance, médiation: les ratés du processus de paix à Sri Lanka” [Good offices, surveillance and mediation: failures in the Sri Lankan peace process], in Critique Internationale, no. 22 Jan. 2004, 35–46, p. 37.
A return to warfare seemed imminent when the Sri Lankan coasts were hit by the tsunami on 26 December 2004. Once the emergency response phase ended, management of reconstruction aid rekindled the conflicts over sovereignty between central government and the separatists. In late 2005, attacks, assassinations and abductions escalated in the north east of the country, fuelling a climate of terror. As ceasefire violations increased the eastern provinces slipped into open warfare during April 2006.
From 2006 to 2007, the army regained control of Batticaloa and Trincomalee in the east, driving the LTTE northwards back towards its sanctuary in the Vanni. The following year, the government officially renounced the ceasefire agreement and tightened its grip around the Vanni, taking control of Mannar district in April 2008 before entering Kilinochchi district in July. In January 2009, the army launched its final offensive. The Tigers were boxed into an area of land along the coast that shrank from 300 km2 in January to 26 km2 in March, 12 km2 on 23 April then to 4 km2 on 8 May. They were wiped out ten days later and their leader was killed along with most of the political and military commanders.
The LTTE cause most of the ceasefire violations in 2005 to 2006, and was largely responsible for triggering the resumption of hostilities. During the presidential elections in November 2005, it urged the Tamil population to abstain, thus contributing to the victory of Mahinda Rajapaksa, a candidate hostile to the peace process and who narrowly defeated CFA negotiator and former prime minister, Ranil Wickremesinghe. According to Sri Lankan political pundit Jayadeva Uyangoda,Jayadeva Uyangoda, “The Way We Are. Politics of Sri Lanka 2007– 2008”, Colombo: Social Scientists’ Association, 2008, p. 7. the LTTE was then counting on a new confrontation to boost its leverage in future negotiations: a war of attrition would weaken the economy, divide the regime’s support base and isolate it internationally due to the war crimes and human rights violations it would certainly commit. Media coverage of the army’s violence was in fact the LTTE’s main political asset on the international scene.
Even before its official withdrawal from the CFA in January 2008, the Rajapaksa administration made it clear that it was not prepared to negotiate any longer. It used the rhetoric of the global “war on terror” following the events of September 11 2001 to put a security and antiterrorist spin on the conflict. Denying the existence of the “ethnic problem” at the heart of negotiations and political debate since 1987, the Rajapaksa administration declared the LTTE as the only obstacle to peace, and sought its military and political destruction.
In the face of rapidly advancing government troops, the LTTE dragged tens of thousands of civilians down with them. As the rebel territory shrank, the Tigers used increasingly violent means to dissuade civilians from fleeing to government-controlled areas, executing those that tried to flee and/or making reprisals against their families, and then, in January 2009, strafing, bombarding and launching suicide attacks on columns of civilians trying to reach government lines.Report of the Secretary-General’s Panel of Experts on Accountability in Sri Lanka, United Nations, 31 Mar. 2011.
Controlling the population was strategically essential to the LTTE for at least two reasons. First, it needed to enlist increasingly younger children to make up for its heavy losses, and second, by mixing fighters with civilians, it forced the government army to choose between two ills: slow down or even halt the offensive, or commit war crimes.
Denouncing the use of the population as a “human shield”, in November 2006 the government asked the ICRC and the SLMM to mediate so it could evacuate civilians living in combat zones to camps behind its lines. The Tigers opposed the operation. Colombo then described its offensive as a “humanitarian mission” seeking to “free innocent civilians held hostage by the LTTE”.Cf., for example, “Offensive to provide water, not to gain territory”, The Sunday Leader, Volume 13, Issue 4 Colombo, 6 Aug. 2006.
In reality, although the army claimed to “adhere to the zero civilian casualty (ZCC) policy”,Ministry of Defence—Sri Lanka, “Ultimatum to LTTE expires: terrorists ignore safe passage for stranded civilians”, 1 Feb. 2009, http://www.defence.lk/new.asp?fname=20090201_01. it did not let itself be troubled by the presence of aid workers and civilians during its push forwards. Camps for internally displaced persons (IDPs), hospitals, humanitarian convoys and food distribution sites were hit by government artillery and air strikes on several occasions.Report of the Secretary General’s Panel of Experts on Accountability in Sri Lanka, UN.
Several hundred civilians fell victim to shells and bullets between 2006 and 2008, several thousand between January and March 2009, and tens of thousands between April and May 2009. According to unofficial UN figures, 7,000 civilians were killed between January and early May 2009, and 13,000 more in the last two weeks of the confrontation. International Crisis Group (ICG) put the figure for civilian deaths at not less than 30,000 during the northern campaign. The government only acknowledged 5,000 civilian deaths and blamed them on the LTTE.ICG, “War Crimes in Sri Lanka’, Brussels: International Crisis Group”, 17 May 2010.
Throughout the conflict, the government carried out an intensive propaganda war designed to mask the terrible human cost of its offensive. It stated that it was leading a “humanitarian war”, thereby justifying its co-opting of NGOs and UN agencies into its pacification policies. From 2006 to 2008, MSF tried in vain to resist. Then, in 2009, it attempted to become a major cog in the military-humanitarian machine in the hope of lessening its brutality.
2006 to 2008: The Government Makes the Rules
From 2006 to 2007, the recapture of the east left at least 250 civilians dead and several hundred wounded, according to local human rights organisations.UTHR(J), Can the East be Won Through Human Culling?, Special Report no. 26, University Teachers for Human Rights (Jaffna), Aug. 2007, http://www.uthr.org/SpecialReports/spreport26.htm.
The fighting displaced 160,000 people. They received various forms of aid from the government, NGOs and UN agencies invited by Colombo to set up in the army’s wake, but this only lasted a few months. In March 2007, by cutting off humanitarian aid and using threats, the government—with the support of the UNHCR— organised the forced return of displaced people to their towns and villages, now destroyed and placed under military rule.
The first government victories went hand-in-hand with escalating political violence (abductions, assassinations and threats) targeting Sri Lankan figures who openly criticised the new administration’s militarism and xenophobic nationalism. Foreign journalists and international NGOs were also the targets of intimidation. Exploiting Sri Lankan society’s distrust of NGOs since their arrival en masse in December 2004, a phenomenon Sri Lankans described as a “second tsunami”, the nationalist media regularly accused humanitarian aid organisations of being “war profiteers” and “stooges of the terrorists”.Cf., on this topic, Simon Harris, “Humanitarianism in Sri Lanka: Lessons Learned”, Feinstein International Center, Tufts University, Briefing Paper, June 2010, https://wikis.uit.tufts.edu/confluence/pages/viewpage.action?pageId=3667....
A grenade attack hit three international NGOs in the eastern provinces in May 2006, wounding three people. On 4 August 2006, seventeen Sri Lankan employees from Action Contre la Faim (ACF) were executed in their office in Muttur on the east coast, a few hours after pro-government forces recaptured the town. The assassination, an unprecedented event in the history of humanitarian action in Sri Lanka and for which the SLMM held the government responsible, was officially condemned by senior western diplomats and the UN. The government responded by creating an investigation commission, whose investigations led nowhere. From 2007 to 2009, more than ten humanitarian workers were assassinated, including several ICRC employees.
MSF’s Goals
Anticipating a renewal of hostilities, MSF’s French section sent several exploratory missions to Sri Lanka in the first half of 2006, which were soon joined by teams from the Dutch and Spanish sections. In July and August 2006, the three sections proposed opening surgical programmes in three hospitals in the government-controlled zone near the front lines in Point Pedro (northern front), Vavuniya (southern front) and Mannar (western front). Their shared objective was to operate eventually in Tiger-controlled zones, with the French section already proposing to open a mission between Batticaloa and Trincomalee on the eastern front, where the first population displacements had been reported.
However, none of the evaluation teams observed any urgent needs. Sri Lanka had qualified personnel and an effective healthcare system, thanks to the ambitious social policies adopted after independence. Furthermore, wishing to assert its symbolic sovereignty over all the national territory, the government had continued to run public services in rebel areas, paying health workers’ salaries and ensuring supplies for medical facilities. In addition, a great many humanitarian aid organisations that had arrived in the wake of the tsunami were still in the country in 2006.
In such circumstances, the operations proposed for Point Pedro, Mannar, Vavuniya and in Tiger-controlled territories were primarily about being prepared. MSF sought to expand its healthcare services and emergency response capacity in areas where the organisation expected the conflict to resume with the predictable consequences: a breakdown in medical supply lines, departure of local medical personnel and an influx of wounded and IDPs. MSF’s goal, even if not always clearly expressed (except by the Dutch section), was also to ensure an international presence in conflict areas in order to “bear witness to the plight of the population”, in the hope of encouraging the belligerents to exercise restraint in the use of violence.MSF-Holland, Sri Lanka Annual Plans 2008 and 2009.
Discord
As the first shells fired by the government’s “humanitarian mission” started to rain down on the eastern front in July 2006, the MSF-France teams thought they could obtain the necessary authorisations to launch their activities within a reasonable timescale. They felt that the organisation had acquired legitimacy in Sri Lanka through its presence on both sides of the front line from 1986 to 2003, and its response to the tsunami. By calling a halt to donations three days after the catastrophe, explaining that reconstruction was the responsibility of the state and that most emergency needs were already covered by the authorities and civil society, MSF had flattered national Sri Lankan pride.
The MSF teams soon lost their illusions. Despite support from the local authorities and the Ministry of Health, requests for import licences, visas and authorisations to travel within the country got lost in a bureaucratic maze. As failure followed failure, it became clear that no decision could be taken without the approval of the Ministry of Defence and the president’s entourage, whose grip on the state apparatus was tightening.
Starting in July 2006, the Ministry of Defence had indeed restricted access to the rebel zones affected by fighting (designated “uncleared areas”) to the ICRC and selected UN agency teams that were only allowed short visits. Other aid organisations had been asked to work in government-controlled zones behind the lines. Failing to negotiate special status, comparable to that enjoyed by the ICRC and UN agencies, the French section decided to exert media and diplomatic pressure. On 9 August 2006, it published a press release denouncing the murder of the ACF workers and the “lack of medical help [for] tens of thousands of people living at the heart of the military offensive”. A week later, it organised a series of bilateral meetings with western ambassadors and the peace process co-presidents, feeling that the latter “had the ear of the government”. In late August, MSF-France managed to meet with Basil Rajapaksa, special adviser to the president, and Gotabaya Rajapaksa, secretary of defence. Although the president’s two brothers assured MSF that it was welcome to work in hospitals designated by the Ministry of Health, they lost their tempers when the head of mission demanded access to rebel zones. MSF was accused of partiality towards the LTTE and of “wanting to tell the government what to do”.Interview with the former MSF-France head of mission on 24 Feb. 2011.
MSF found itself in a delicate negotiating position. In August 2006, it had no information indicating that the aid provided by the government, ICRC and UN agencies in the “uncleared areas” was inadequate. MSF estimated that the existing set-up would not be able to cope with the expected influx of wounded and IDPs, an assessment rejected by the government who claimed that the consequences of the conflict would be minimal and handled appropriately by the authorised agencies. In reality, these disagreements masked underlying discord: MSF was keen to use its freedom of speech to denounce the excessive use of force its teams might witness while the government was keen to limit the number of observers likely to reveal the war crimes it was to commit.
Crisis
On 30 September 2006, while head office was encouraging the MSF field teams to stand firm, the French section learned from the national daily press that it was subject to an expulsion order, along with MSF-Spain and five other international NGOs. This was confirmed the same day in a letter from the Department of Immigration ordering MSF teams to leave the country within one week due to “activities […] in contravention of the visa conditions”. The press blamed the expulsion on MSF’s pro-LTTE commitment: quoting Ministry of Defence sources, it claimed that the organisation had carried out “clandestine activities” for the Tigers under cover of post-tsunami reconstruction aid.Cf., for example “Four INGOs to be booted out over link with Tigers”, The Island, 30 Sept. 2006; “Ignominious departure for INGOs, under fire for alleged assistance to LTTE and non-implementation of post-tsunami rebuilding pledges”, The Sunday Times, 8 Oct. 2006.
MSF immediately asked for support from the embassies of the expatriates targeted by the expulsion measures. On 5 October 2006, the minister of human rights told MSF that the expulsion order was on hold pending the results of an investigation into its activities. The head of state had just met with the CFA co-presidents and officially declared that he “would continue to facilitate humanitarian access to the conflict-affected areas while keeping in mind security considerations”.
Nevertheless, MSF staff still had no work permits and remained publicly accused of pro-LTTE clandestine activities. In mid-October 2006, the heads of mission wondered what they could do to rebuild MSF’s reputation when there was little chance of a government retraction. MSF’s international president, who had come to support them in the wake of the expulsion, had tried to publish a denial in the local media, calling a press conference in the hope of “clearing MSF’s name”. Only two (English-language) newspapers reported it.
What safety guarantees should MSF demand from the authorities, the heads of mission asked themselves, when the ICRC had just come under grenade attack a few days after having been accused of pro-LTTE partiality by the press, and the Ministry of Defence had refused to meet with MSF, relegating the crisis to a visa problem that had already been solved. Should they be happy with the suspension of the expulsion order and recent press restraint (MSF-Holland) or demand a public statement of support announcing that proceedings were being dropped and guaranteeing MSF teams’ safety (MSF-France) in line with the international president’s publicly-expressed position? How long could MSF wait for work permits?
Although all the sections were wondering if they should pull out, only MSF-France seemed determined to put words into action; on 13 October 2006, the head of operations warned: “If we don’t see some concrete results soon, we will have to take the decision to leave the country because of the lack of humanitarian space”. Not everyone agreed with this option: could they turn their back on the country when all evidence pointed to the conflict being on the brink of escalating? What purpose would be served by one or more sections leaving? Should they simply redeploy their intervention resources to those areas where the organisation was accepted? Or stage a media event to put the government in an awkward diplomatic position and strengthen the negotiating position of the organisations that were staying put?
Compromise
The three sections finally chose to continue to negotiate. They stopped seeking an official denial, the abandonment of the investigation and a public statement of support, and ended up signing a Memorandum of Understanding (MoU) allowing them to launch operations in three hospitals selected by the Ministry of Health. The question of access to “uncleared areas” was not raised. The projects opened in December 2006 and January 2007.
During the two years that followed, the medical-surgical missions in Point Pedro (MSF-France), Mannar (MSF-Spain) and Vavuniya (MSF-Holland) were not over-stretched. In 2007, most of the wounded and people displaced by war were concentrated on the eastern front, while in 2008 the operation to surround the Vanni had not yet caused many civilian casualties. MSF’s operations did nonetheless ensure continuity of healthcare (emergencies and surgery) in hospitals with insufficient specialists, dealing with supply breakdowns and the rigours of military occupation. In Vavuniya, MSF-Holland had to suspend surgical activities in March 2008 as the increased Ministry of Health teams made its presence redundant. MSF-Spain decided to close the Mannar programme after the army recaptured the district in late 2008, and left the country the following year.
The French section tried nevertheless to gain access to the eastern provinces where the army was making fast progress. In order to be allowed into the “uncleared areas”, it turned to the UN. In late October 2006, the resident UN coordinator endeavoured to negotiate a procedure with the government for designating organisations approved to work in rebel zones and, in November 2006, it obtained authorisation for access from the Ministry of Defence for twenty-one NGOs, one of which was MSF.
Having obtained their passes, the coordination team carried out an evaluation mission in Tiger-controlled areas close to Vaharai in February 2007. However, it did not manage to obtain the necessary authorisations to start up the project before the government forces recaptured the zone a month later, making the planned intervention irrelevant. In April 2007, it proposed providing support to the Batticaloa hospital as the surgical unit was overflowing after the army’s recapture of the coastal strip to the south of the town. Once again, Colombo’s administrative obstruction and the lack of human resources in Paris delayed the intervention. The surgical teams arrived in August 2007, at a time when the hospital’s activities had returned to normal and the eastern provinces were almost entirely pacified.
The French section settled for helping IDPs, providing modest support (mobile clinics, sanitation and distribution of essential goods) to around 30,000 of the 160,000 people caught in the midst of the government’s forced displacement/resettlement operation. It closed its programme in January 2008, without ever really looking at the issues raised by its participation in forced population transfers organised with HCR support.
In the end, only the Dutch section managed to set up in Tiger-controlled territories, although it was far from the combat zone. In May 2007, it opened a programme in the LTTE “capital” Kilinochchi which was not yet affected by the fighting. It chose to support the gynaecological, obstetrical and paediatrics units with a view to getting prepared.
But as the front came closer in the summer of 2008, bringing displaced civilians to Kilinochchi, difficult relations with the hospital’s medical staff forced MSF to limit its intervention to logistics aid for the waste treatment area and building latrines for the IDPs. On 8 September 2008, the government ordered all the humanitarian aid organisations other than the ICRC and selected UN teams to evacuate the Vanni.
MSF was one of the first organisations to leave the LTTE zones. Its immediate efforts to return encountered a categorical refusal from the secretary of defence, whom they met on 28 November 2008. Asked to pressure the authorities, the Indian and western embassies said they were powerless. Since 2007, Sri Lanka had been drawing closer to China, Pakistan and Iran, with which it had signed a series of economic and military agreements.
After three years of negotiation, as the conflict seemed on the verge of a decisive confrontation that would not spare the civilian populations, MSF had just one surgical programme in Point Pedro, a small-scale project supporting the Vavuniya health district, and very little hope of gaining access to conflict zones. Moreover, MSF was not comfortable with making its voice heard: since the 2006 crisis, it felt that public criticism of the government was likely to lead to expulsion or even physical reprisals against its staff. The MSF teams seemed completely at a loss as to what to do.
2009: All-out War and the Humanitarian Solution to the Tamil Question
Between January and May 2009, the fighting was concentrated on a constantly shrinking and densely populated area and the number of civilian victims increased sharply. In LTTE zones, the wounded had access only to rudimentary care provided by eight Sri Lankan doctors from the Ministry of Health who had refused to abandon their post. The ICRC, which continued to provide them with medical supplies overland then by sea until 9 May 2009, managed to transfer 6,600 wounded and seriously ill people as well as those accompanying them, a total of 13,000 people, to government-controlled areas.
The army evacuated almost 300,000 people from territories gradually recaptured from the Tigers. Soldiers escorted the survivors to transit zones where they were screened: people suspected of belonging to the LTTE were transferred to demobilisation camps, called “rehabilitation centres”, and the others to closed internment camps managed by the army and called “welfare centres”. Ringed by several rows of barbed wire, the camps were guarded by the army and police.
The largest “welfare centre” was at Menik Farm to the south of Vavuniya, in a marshy and isolated area. Its construction began in September 2008 and was coordinated by the army, which completed the first two zones of the complex. In early February 2009, Colombo asked for help from humanitarian agencies and donor countries in building five additional zones. The medical project included the opening of 1,400 beds in hospitals around the centre and installing five small hospitals and twenty health units within the centres. These “welfare villages” were intended to house 200,000 people for three to five years. Donors were very reluctant to finance construction of permanent internment camps, but ended up agreeing to support the emergency programme for a few months, in exchange for a commitment from the government to resettle 80% of displaced people by the end of 2009.
In February 2009, the announcement of the setting up of Menik Farm stirred up controversy both nationally and internationally, a controversy that grew fiercer in July. Sri Lankan, Indian and British members of parliament compared the “welfare centres” to “concentration camps”, reminiscent of those in Nazi Germany.Jeremy Page, “Barbed wire villages raise fears of refugee concentration camps”, The Times, 13 Feb. 2009. International journalists, who had been banned from going to Menik Farm other than during a handful of guided visits organised by the army, gave wide coverage to alarmist claims about health conditions in the camps. In July, British daily newspaper The Times claimed it had been told by senior aid sources that 1,400 people were dying in the camp each week,Rhys Blakely, “Thousands die in Tamil ‘welfare village’”, The Times, 10 July 2009. and added that the death toll lent credence to allegations of “ethnic cleansing” by the government. The press began to question the role of the UN and aid organisations. The UN was accused of “having hidden the scale of the massacres”,Philippe Bolopion, “L’ONU a caché l’ampleur des massacres au Sri Lanka” [The UN hid the scope of massacres in Sri Lanka], Le Monde, 29 May 2009. British aid to war victims was suspected of being used “to fund concentration camps”,Jeremy Page, “British aid for war refugees may be used to fund ‘concentration camps’”, The Times, 28 Apr. 2009. and the UN and NGOs of being “complicit in a large-scale detention operation”.“Sri Lanka, stop!”, Le Monde, editorial, 10 Sept. 2009.
Waiting in the Wings
Between January and 20 April 2009, MSF watched the crushing of the Vanni from afar. In late January 2009, the first civilians began to arrive in the government-controlled zone, making the Dutch section operational once more. The sick and wounded evacuated from the combat zones began to crowd into Vavuniya’s general hospital, where the number of hospitalised patients jumped from 365 to 1,004 between 1 February and 1 April. First one, then another MSF-Holland surgeon came to join the Sri Lankan team. MSF hired nursing auxiliaries to improve post-operative care. But it could do no more: the authorities refused to allow an anaesthetist and two extra expatriate nurses to join the team. They also opposed increasing surgical teams in the other hospitals which were taking in the wounded evacuated by the ICRC.
In Vavuniya district, the dozen internment camps set up in public buildings were soon overwhelmed, leading soldiers to transfer the first interned civilians to zones zero and one at Menik Farm in February. The military and health authorities in Vavuniya asked for support from the UN and NGOs to assist recently evacuated populations. The local authorities were seeking organisations to distribute special food supplements to the under-fives and pregnant and breast-feeding women in the internment centres, and the Dutch section agreed to help. Distribution began in mid-February 2009, despite the lack of any formal agreement from the Ministry of Health in the capital, which had made clear its wish to be the sole provider of medical and nutritional assistance in the camps. “[Local administrators] really want us to bring staff, no matter what they say in Colombo. We also got full access to all camps, and the army general [in charge of supervising the camps] gave us his personal cell number in case anyone objects”, reported the MSF-Holland head of mission.
In direct contact with the displaced and wounded coming out of the Vanni, the Dutch section played a part in disclosing the brutality of the regime’s counter-insurgency campaign and its internment policies. Between January and March 2009, it issued a press release and posted several updates on MSF websites describing the living conditions of civilians caught up in artillery fire in the Vanni and the lack of freedom for the displaced people interned in Vavuniya. Several MSF representatives talked to the international media about these issues. While the ICRC was claiming that “plain common sense dictate[s] that the civilian population should be urgently evacuated [from combat zones]”, “Sri Lanka: ICRC reiterates concern for civilians cut off by the fighting”, 4 Mar. 2009, http://www.icrc.org/eng/. MSF “called on all parties to the conflict to allow independent humanitarian agencies to provide medical aid to the wounded in the Vanni”.
With activities functioning only in Point Pedro, the French section took a more discreet approach. It limited itself to relaying some of MSF-Holland’s information and giving a number of interviews in which it expressed alarm at the bombing of civilian zones and health facilities, a practice already strongly condemned by the ICRC, human rights organisations, the UN and western embassies, which in February demanded a “humanitarian ceasefire” to spare civilian lives.
An Emergency Situation
On 20 April 2009, the army broke through the LTTE’s defensive lines and cut its territory in two, triggering the evacuation of over 100,000 civilians in just a few days. The final battle caused an additional 77,000 to be displaced between 14 and 20 May. The evacuated included a great number of wounded. On 21 and 22 April, 400 patients were admitted to Vavuniya hospital, where MSF and Ministry of Health teams operated day and night. In mid-May, the hospital had over 1,900 hospitalised patients, and just 480 beds. As army bulldozers cleared zones 3 to 5, the Menik Farm population rose from under 30,000 inmates to over 220,000 in five weeks. Forty-five thousand people were also interned in small temporary camps in Vavuniya district and 21,000 in camps in Jaffna, Mannar, Batticaloa, Trincomalee and Ampara.
From 20 April the two MSF sections set themselves three priorities: provide emergency care to IDPs in the transit zone, boost operative and post-operative capacity (notably by deploying a field hospital) and develop healthcare provision inside the internment centres. The local authorities, seemingly caught off guard by the scale and speed of the population displacements, proved receptive to most MSF proposals, even asking the Dutch section to open mobile clinics inside the camps “as soon as possible”.Office of the Regional Director of Health Services, Vavuniya, “To MSF-Holland Project Coordinator. Request for Medical Team to Work at IDP Camps”, 21 Apr. 2009.
In Colombo, the Ministry of Health opposed the proposals. The master plan it had just updated with help from the WHO and UNICEF gave the monopoly in healthcare and public health activities within the camps to the government and carefully selected partners. But Colombo was particularly interested in MSF’s proposed interventions outside the internment camps as they fitted in with its plans. On 16 May, the French and Dutch sections each signed a new Memorandum of Understanding with the Ministry of Health authorising them to launch three projects: open a 100-bed surgical field hospital opposite the Menik Farm detention centre (MSF-France), provide additional assistance for treating the wounded at Vavuniya hospital (MSF-Holland), and open a post-operative care unit in Pompaimadhu (MSF-Holland). Faced with an emergency situation, MSF chose to go along with the government’s action plans and made two concessions: it renounced, for the time being, negotiating access to transit zones and internment camps, and signed a MoU committing it to “strictly maintain the confidentiality of the information on service provision” and make “no comments […] without the consent of the Ministry of Health Secretary”.
As the programmes approved by Colombo opened in under two weeks, the teams tried to go beyond the authorised activities. When the second wave of IDPs arrived, MSF-Holland succeeded in negotiating at the local level the dispatch of a four-person team to the Omanthai transit zone (where it had tried in vain to intervene in April). From 16 to 20 May, MSF doctors helped with the triage of 77,000 survivors of the final offensive and with boarding them onto army buses heading for the internment camps. The team treated 750 patients, mostly with old wounds that had received little or poor care. All they could do was provide emergency treatment (cleaning wounds, administering antibiotics and pain relief), refer the 200 most serious cases to the hospital at Vavuniya, which they knew was overflowing, and hope that the wounded transferred straight to the camps would receive the care they needed to prevent them from developing crippling and/or fatal infections.
Some of the wounded were transferred to Mannar hospital. The ICRC, which had set up a surgical team in the hospital, reported 800 patients and contacted MSF directly to reinforce its teams. From 23 to 24 May, joint ICRC, MSF and Ministry of Health teams operated on sixty patients with old and infected wounds. But on 25 May as it had not received prior approval from the Ministry of Health, the hospital’s management received an order from Colombo to break off cooperation with the ICRC and MSF.
Doubts Arise
Access to camps then became a key issue for MSF. Since the government’s “humanitarian mission to rescue civilians held hostage by the LTTE” had turned out to mean carpet-bombing, then would the “welfare villages” turn out to be places where the Tamil population would be left to die?
Access to internment camps was strictly regulated; however, access was possible for national and international staff from MSF, fifty-two NGOs and UN agencies, except during several forty-eight-hour periods when the security forces carried out screening operations seeking to identify suspected LTTE militants. Even so, MSF was unable to get a precise picture of the health situation. Claiming the monopoly on producing numbers, the government banned any independent epidemiological surveys. The MSF teams had only an approximate idea of health conditions in the camps, based on their visual impressions, brief interviews with internees and longer discussions with hospitalised patients at Vavuniya and Menik Farm. They completed their rough assessment by sharing information with Sri Lankan health workers, national and international employees of other aid agencies, and the security forces, including a number of government officials who openly criticised Colombo’s refusal to authorise greater access to the camps for international organisations.
The general impression was that the two huge waves of internees in April and May had created considerable chaos, but that it had gradually been brought under control by the government and aid organisations coordinated by major-general Chandrasiri, the overall head of the internment complexes. The major-general presided over inter-agency coordination meetings and managed aid with an iron fist. In late May, OCHA noted that the camp was short of 15,000 shelters (out of 40,000), that half the latrines had been built and that 75% of water requirements were being met. In private, its representatives acknowledged that the aid services had deployed at an incomparably faster rate than, for example, the slow and chaotic response from the UN and NGOs in Darfur in 2004.
The ministry’s master plan seemed to draw straight from public health guidelines drawn up by the WHO and MSF, but the government appeared to have trouble implementing them, despite claiming the enlisting of 300 doctors and 1,000 nurses. The teams learnt from different concurring sources (the police, the morgue and the ICRC in charge of distributing body bags) that the number of deaths at Menik Farm was between ten and fifteen a day in late May. When set against the overall population of the camp, it corresponded to a daily mortality rate of 0.45 per ten thousand and, although this rate was much lower than the emergency thresholds used in Africa, it was three times higher than the national average. The detainees were not dying en masse, but the initial disorganisation of the healthcare system
(denounced by some of the Sri Lankan doctors who went on strike in the summer) was in all likelihood the cause of a higher death rate among physiologically weakened inmates, such as the wounded, the elderly, children and those suffering from chronic diseases.
In June, the two MSF sections made several proposals for interventions inside the camps (primary healthcare, nutrition, surgical consultations, mental healthcare, epidemiological monitoring, etc.). They were all turned down, more or less explicitly. This refusal increased the teams’ doubts and unease. Why was the government insisting on prohibiting MSF from carrying out any health activities within the camps? Was it trying to mask a serious deterioration in the health situation, or ferocious political repression?
The MSF-France teams working at the Menik Farm hospital were particularly puzzled. No more than 70% of beds were occupied, whereas the other outlying hospitals were still overflowing. With no control over selecting the patients arriving from the camps, MSF wondered what was behind the underuse of its hospital. How could it be sure that the most serious cases were being given priority? Were the patients subject to a politically-skewed selection process? Was the MSF hospital merely a propaganda tool for a government seeking to create the appearance of normality? At the head offices and in the field, many MSF members asked themselves if all the sections should leave the camps and denounce the regime’s detention policies, to which aid organisations were public health auxiliaries.
Making a Choice
Following a visit by head office in June 2009, the French section chose to stay put, although they were fully aware of the role the government had assigned them: contribute to maintaining public health order in the internment camps, the main function of which was to monitor and control “dangerous” populations and stifle any fresh surge in Tamil nationalism.Fabrice Weissman, “Welcome to the farm. MSF and the policy for interning the displaced people of Vanni”, report of the visit to Menik Farm and Colombo camps (Sri Lanka), 4–14 June 2009. Paris, Fondation MSF/ CRASH, July 2009.
Having decreed the abolition of minorities and thereby dispensed with taking their political aspirations into account, In July 2009, the president stated his belief in “my theory…[that] there are no minorities in Sri Lanka, there are only those who love the country and those who don’t”, cf., The Hindu, 6 July 2009. the Rajapaksa administration sought to reduce the citizens from the Vanni to beneficiaries of the state’s humanitarian benevolence, well-cared for, well-fed, well-housed and, most importantly, well-guarded. The Menik “Farm” symbolised this policy, which extended beyond the barbed wire, as illustrated by the Ministry of Defence’s decision to recruit 50,000 extra soldiers after the war was over. This last initiative lent credence to critics of the regime who denounced a pacification of the Vanni in the form of long-term military occupation.
The only concessions that the international actors (states, the UN, NGOs, etc.) could count on concerned the relaxing of the detention policy: transparency of the screening process, release of certain categories of internees and improved detention conditions. Head office felt that MSF should contribute to these improvements. MSF-France therefore sought to become an essential cog in the internment camps’ health system: in July, it expanded its hospitalisation capacity, improved its technical services (radiology, ultrasound, laboratories, etc.) and replaced the hospital tents with semi-permanent buildings. It also started to try and get some internees released on medical grounds.
This position was poles apart from the stance taken by other humanitarian aid organisations and donors, particularly the USA and the EU. Funding the camps to the tune of 700,000 dollars a day, in June 2009 the UN and its donors opposed the major improvements in aid standards demanded by the government (construction of permanent shelters and latrines with septic tanks, extension of healthcare infrastructures and the running water network, etc.) so as to underline the temporary nature of the internment camps. During the same period, most NGOs refused to distribute cement to consolidate the floors of the tent and plastic shelters. Yet the housing conditions were precarious. The tents and tarpaulins used throughout the zones (apart from zones 0 and 1 which had permanent structures built by the army) deteriorated rapidly while the latrines overflowed and a foul-smelling tide of mud flooded the groundsheets. In a strange reversal of roles, the government accused aid organisations of causing a “humanitarian crisis” and holding the IDPs hostage to make the authorities give in to their demands. The accusations grew fiercer in August 2009 when the first monsoon rains transformed the camps into open sewers. But images of flooded camps also served as a tool for mobilising opinion and were seized upon by human rights organisations and some Sri Lankan politicians who demanded “a prompt and rapid resettlement of displaced persons to their places of origin”.
The decision by General Sarath Fonseka, commander-in-chief of the Sri Lankan army and leader of the victorious offensive, to join the opposition and run against the outgoing head of state in the presidential elections planned for January 2010, had indeed placed the issue of IDP internment centre stage. Rajapaksa and Fonseka shared the same support base and were trying to attract the minority vote. In August 2009, the former commander-in-chief denounced the fate meted out to internees by the Rajapaksa administration. Combined with international pressure, these electoral concerns persuaded the regime to open the camps and initiate a fast-paced resettlement policy starting in September 2009. By 31 December over half the IDPs had already been sent back to their towns and villages, destroyed, mined and tightly controlled by the army and plainclothes security forces. The French and Dutch sections closed down their emergency programmes. The Menik Farm hospital never became the main hospital for the internment camps. Four thousand admissions were recorded between 22 May and 6 December including 585 suffering from war wounds. According to the information gathered from local health authorities, this 4,000 represented 5% to 10% of all hospitalisations from the camps.
Having returned to Sri Lanka believing that it benefited from a special status in the aid world, MSF found itself in an extremely delicate negotiating position, on a par with the other NGOs. Its weak position sprang primarily from the Tigers’ “human shield” strategy of victimisation, which subverted the humanitarian narrative into a propaganda tool to sustain a movement using totalitarian practices. Using the LTTE’s treachery as justification, the government showed a remarkable capacity for organising and justifying the subjugation of humanitarian aid organisations to its political and military interests. MSF found itself assigned the role of assisting in a pacification policy that had settled the ethnic question in Sri Lanka by bombings and military surveillance, providing humanitarian aid to populations decreed to be dangerous.
Under permanent threat of administrative obstruction and violent reprisals, MSF did not know how to get the political support it needed to resist. Lacking allies in Sri Lankan society, it looked to western states and the UN, whose influence was waning. MSF ended up accepting the government’s diktats, imposing the places, targets and mechanisms for intervention, while counting on bureaucratic flaws in the system and its internal pockets of protest to retain some degree of autonomy. MSF decided not to make use of its freedom of speech to attack a regime that was eager to appear to the world and its own society as the guarantor of a rule of law and democratic values. At the end of the day, MSF adopted a policy of opting for the lesser evil, aimed at improving the condition of survivors of an all-out war that no political power seemed capable of checking.
Translated from French by Nina Friedman
***
Ethiopia. A Fool’s Game in Ogaden
Laurence Binet

The Ogaden region in the Somali regional state of Ethiopia has been the scene of conflict between the Ethiopian federal government and the Ogaden National Liberation Front (ONLF) separatist movement since 1994. In April 2007, the fighting intensified. After a series of rebel offensives, a wave of repression hit the region, which saw villages attacked and burned, violence and forced displacements, denial of access to wells and a blockade on all commercial traffic, vital to the nomads who inhabit the area. Jeffrey Gettleman, “In Ethiopian Desert, Fear and Cries of Army Brutality”, The New York Times, 18 June 2007.
In 2007, MSF’s objective was to provide care for the victims of the conflict. In a region with very few medical facilities and a dispersed population, this meant supporting health centres and organising mobile clinics to go where patients were in need of treatment.
Since the beginning of 2007, the Dutch section’s team had been trying to set up a programme in the Wardher hospital on the outskirts of the conflict, but the army regularly denied MSF access to the population living in the area. After a rebel attack near its base in July, MSF decided on a temporary evacuation that was followed by the authorities banning the organisation from returning. Before pulling out, during the few rounds of medical consultations it had managed to hold, MSF had been able to collect witness reports on the acts of violence committed by the warring factions.
During the same period, the Belgian section was prohibited from completing an exploratory assessment at the centre of the conflict zone in the area around Fiq where it was preparing to start up a programme and the ICRC, accused by the Ethiopian authorities of supporting the ONLF, was expelled from the Somali region.
No other humanitarian organisations were active in the conflict-ridden areas of Ogaden. The army’s distribution of WFP aid raised questions of impartiality as it was suspected of using the aid to reward people for keeping their distance from the ONLF.
In early September, after a series of diplomatic meetings with Ethiopia’s main donors and other stakeholders that brought few results, MSF held a press conference to condemn the government’s refusal to allow humanitarian organisations into the Ogaden region. MSF, “MSF Denied Access to Somali Region of Ethiopia despite Worsening Humanitarian Crisis”, press release, 4 Sept. 2007.
Accounts of human rights violations, documented by the Dutch section, were also cited at the press conference and reported by the international media. “Ethiopia Blocking Civilian Access to Medicine in Conflict Zone, Agency Says”, Associated Press, 4 Sept. 2007.
The government then accused MSF of violating its sovereignty and supporting the ONLF. “Ethiopia: Government Denies ‘Blocking’ NGO”, IRIN, Nairobi, 4 Sept. 2007.
The Belgian section was ordered to close down its long-standing programme for tuberculosis patients outside the conflict zone and the ban on the Dutch team returning to Wardher was maintained.
In the meantime, OCHA, responding to the alerts on the situation in Ogaden, issued in particular by MSF, sent a fact-finding mission which reported a worsening of the health and economic situation in certain areas:“Report on the Findings from the UN Humanitarian Assessment Mission to the Somali Region, 30 Aug.–5 Sept. 2007”. difficult access to water and food, shortage of drugs and therapeutic foods, and many cases of acute diarrhoea and measles. In November, OCHA obtained permission from the Ethiopian authorities for several international organisations to work in Ogaden. As the authorities were continuing to block the return of the Belgian and Dutch sections, the MSF movement encouraged applications from the Swiss and Spanish sections that went on to become some of the chosen few. OCHA also obtained the promise that WFP officials could be present when the army distributed food aid, a promise that was not to be kept.
In January 2008, the Swiss and Spanish sections started up medical and nutritional programmes in the areas of Fiq and Degeh Bur that were directly affected by the conflict and the Dutch section returned to Wardher, without authorisation but not officially banned either. But, in reality, by mid-January the operations of two sections were at a standstill. The team of the Dutch section was put under house arrest in Wardher after one of its lorries refused to stop at an army roadblock, and several national staff members were accused of spying for the ONLF. With no explanation, an MSF-Switzerland field team was also ordered to shut down its exploratory mission and forbidden to leave the hotel. Before the mission was suspended, the team had observed that the people it had encountered were victims of violence and suffering from shortages of water, food and medical care due to the restrictions on movement caused by the conflict. However, MSF headquarters was reluctant to draw overall conclusions from these events with regard to the situation in the region as a whole.
In March, the house arrest orders had only just been lifted when all the MSF teams were hindered, on the pretext that most of the expatriate staff members didn’t have work permits.“Letter from MSF International Office Secretary-General to Ethiopian Prime Minister and Minister of Foreign Affairs”, 31 Mar. 2008.
In May, a severe nutritional crisis necessitated the assistance of international organisations to conduct emergency relief operations in several Ethiopian states and the authorities took a more relaxed attitude to the question of work permits.
In the Fiq area, however, the MSF-Switzerland field teams were still paralysed and, in June, several national staff members were accused of spying and imprisoned. A month later, the Swiss section shut down its programme and issued a public condemnation of the administrative obstruction that was preventing it from providing relief to the population.MSF-Switzerland, “Ethiopia: Repeated Obstructions Lead MSF-Switzerland to Pull Out from Fiq, Somali Region of Ethiopia”, press release, 10 July 2008.
It also circulated a document to donors, international institutions and embassies denouncing the Ethiopian authorities’ exploitation of emergency food aid for political ends and the absence of a response from the United Nations.MSF, “Access and Response in the Somali Region: Mission Impossible? The Case of MSF-Switzerland in Fiq”, report, Dec. 2007–June 2008.
The other sections, hoping to be able to work within the limits allowed them and judging that they lacked solid evidence of the misappropriation of aid, did not join MSF-Switzerland in the condemnation.
In the following years, managing as best they could with the endless administrative hurdles, they instigated programmes to support health facilities in areas of ongoing, low-intensity conflict. They provided medical and nutritional aid to the inhabitants—who lacked such care even in times of peace—and medical care to Somali refugees in the transit camps on the border.
Conflicting Objectives
The issue of access to Ogaden in 2007 to 2008 was marked from the outset by a conflict between MSF’s goals and those of the Ethiopian government. The latter regarded international humanitarian organisations’ aid to the inhabitants of ONLF-controlled areas as potential support for the rebellion. Any contact with the insurgents—even though such contact was crucial to impartial distribution of aid and the safety of the humanitarian teams—was condemned as a sign of political partiality. This position was clearly expressed and defended during meetings with MSF representatives and in the official correspondence sent to them.Letter from Tekeda Alemu, Ethiopian minister of foreign affairs, to the heads of mission of the Belgian, Dutch, Swiss and Spanish sections of MSF, 18 Feb. 2008.
In 2009, the president of the Somali regional state even confided to a journalist that he believed “that MSF has a hidden agenda. MSF is consulting the ‘elders’ [clan chiefs] who have close relations with the ONLF, and hiring personnel who support the ONLF”. Peter Gill, Famine and Foreigners: Ethiopia since Live Aid, Oxford: Oxford University Press, 2010. MSF, convinced of the legitimacy of its cause of providing assistance to the Ogaden people, took a while to realise just how intransigent the government was. It tried to resist the pressure by playing on the fact that there were several MSF sections present and using the levers of diplomatic negotiation and public statement. But those public statements worked to its detriment. The September 2007 press conference referred to the accounts of violence logged by the Dutch section’s team, even though they had been regarded initially as insufficiently documented. This increased the Ethiopian authorities’ mistrust of MSF, who they accused of spreading propaganda on behalf of the ONLF under cover of providing humanitarian aid. A few weeks later, representatives of MSF were able to experience the government’s intolerance of criticism first-hand. During a meeting with the foreign affairs minister, they were shown a file of press cuttings containing all of MSF’s public criticisms of the government dating back to its denunciation of forced displacements during the famine of 1985.
In July 2008, the Swiss section’s public criticism of the government’s refusal to allow access to the area was weakened as the two other MSF sections were still in Ogaden and did not join in the accusation. A paradox that did not escape the notice of the authorities, who publicly accused MSF of “disseminating rumours whose content is clearly at odds with the reality on the ground”. “Ethiopia Slams Swiss Charity over Ogaden Pull-out”, Reuters, 12 July 2008.
When it came to negotiating with the authorities, even the heads of mission acknowledged that MSF’s network of official contacts in Ethiopia was insufficient and poorly organised. The operational teams, often with little experience in the country, struggled to identify the right contacts within a complex governmental system with blurred levels of responsibility; decisions on authorisations and restrictions were taken sometimes at regional level and sometimes at federal level, sometimes by the health authorities and sometimes by the army, without any clearly defined rules.
On the diplomatic front, the team responsible for coordinating the different MSF sections’ relations with countries, civil society and international institutions saw that appealing to the African Union would be futile, given Ethiopia’s prominent role in the organisation. The team therefore concentrated its efforts on United Nations agencies and western donors who, as providers of aid to Ethiopia, were liable to take seriously the difficulties experienced by the people of Ogaden in gaining access to their aid. But Ethiopia is the United States’ main African ally and its partner in the “war on terror”, particularly in Somalia where the Ethiopian government plays a leading role in the combat against Islamist insurgents. See infra, “Somalia: Everything is open for negotiation”, pp. 77–106.
Most of the diplomats and representatives of those UN agencies present in Ethiopia privately expressed their alarm at the government’s refusal to allow access to the area and its misappropriation of aid. While many of them encouraged MSF to voice what they were thinking, none of them seemed to have either the means or the ambition to change the balance of power with the Ethiopian government, a past master in the art of controlling aid.
Over the course of these events, the Ethiopian authorities manoeuvred MSF into waltzing twice round the floor. The first time of the first round began when the Ethiopian government launched a crackdown and denied access to the area from April to November 2007. The second was marked by MSF’s diplomatic and public protests, and the third by a spurious opening-up in November, briefly imposed on the Ethiopian government after pressure from the United Nations.
In 2008, events speeded up in the second round. Access was refused for longer, the period of opening-up was no more than brief. The authorities engaged in virtually uninterrupted harassment, paralysing all action by the MSF teams.
If MSF resisted the first waltz, it subsequently bent to the tempo that permitted it to stay at the dance. Since what was to be to date its last public statement on the situation in Ogaden, the organisation has kept a low profile, hoping to improve its relations with the authorities and thereby gain wider access to the region. This strategy is designed to enable MSF to assist the inhabitants should the conflict intensify, but there is no reason to believe that the Ethiopian government will be any more willing to open up the area than it was in 2007 and 2008.
Translated from French by Neil Beschers
***
Yemen. A Low Profile
Michel-Olivier Lacharité
In 2004, an insurrection led by former member of parliament Hussein Al Houthi broke out in the northern Yemeni governorate of Saada. His supporters objected to the Yemeni government’s political rapprochement with the United States, and demanded the return of Zaydism— the school of Shi’a Islam whose imams ruled Yemen until 1962. Lasting from June 2004 to February 2010, the Saada War was characterised by periods of intense conflict interspersed with relative calm.
The French section of Médecins Sans Frontières conducted an initial exploratory mission in northern Yemen in July 2007, after the signing of a ceasefire a month earlier under the auspices of the government of Qatar. After four episodes of fighting, the government had failed to suppress the Houthist movement, which had failed to gain control of any territory. MSF’s objective was to improve access to secondary healthcare in the Saada region, which had few hospitals and was at risk of renewed hostilities with the predictable consequences (war wounded, population displacements, etc.). The organisation started working in Haydan hospital in September 2007, in Razeh hospital in December 2007, and in Al Talh hospital in April 2008. While all three hospitals were in government-held areas when MSF first arrived, they progressively came under Houthi control during the course of the war—Haydan in 2008, and Razeh and Al Talh in 2009.

There was very little media coverage of the Yemen conflict between 2004 and 2007. The lack of war images and reports was due to the Yemeni government’s extremely tight control over information, exercised through physical persecution of journalists and legal prosecution of the regime’s opponents.Patrice Chevalier, “The Yemeni Law and How to Use it Against Journalists”, http://hal.archives-ouvertes.fr/docs/00/36/17/00/PDF/Chevalier_The_Yemen... — version 1, 16 Feb. 2009.
These prosecutions stepped up in 2001, helped by Yemeni involvement in the “global war on terror”, which signified its alignment with the United States.Chevalier, “The Yemeni Law”, http://hal.archives-ouvertes.fr/docs/00/36/17/00/PDF/Chevalier_The_Yemen... — version 1.
The government also controlled the communications of the supporters of Al Houthi’s movement. Journalists close to the government created a think tank and a website, http://www.nashwannews.com. See Samy Dorlian, “Yémen: observation sur le traitement médiatique de la guerre de Saada”, Olfa Lamloum (ed.), Médias et islamisme, Beirut: Presses de l’Ifpo, 2010, Coll. Études contemporaines. the analyses of which were aimed at limiting the rebels’ capacity for political mobilisation, leaving them with almost no way to get attention, aside from pamphlets distributed to the population and rare contacts with the few journalists who dared cover the conflict.
However, by the time MSF launched its project in September 2007, the situation had evolved over the previous months. Qatar’s diplomatic intervention had brought media attention to the conflict—notably by Qatari satellite channel Al Jazeera. The insurgents began distributing DVDs with footage of the war, their military victories and speeches by their leaders, and posted information via electronic mailing lists, allowing them to circumvent the pro-Houthi websites that had been taken down.
MSF was the only international aid organisation to reach the combat zones, aside from the ICRC, which was acting through the Yemeni Red Crescent. One of the few foreign witnesses to the conflict and its disastrous consequences for the population, the organisation faced a dilemma; should it help expose the violence of this little-known war, at the risk of jeopardising its work? Between 2007 and 2009, the shifting context of intervention prompted MSF to choose caution. Its room for manoeuvre depended largely on the goodwill of the government, which required that travel by international staff, drugs and MSF supplies all be approved on a case-by-case basis by the Ministry of Planning, the police, and the governor of Saada. In 2009, MSF deliberately limited its communications to only making its activities in Yemen known locally—in other words, to gaining acceptance from the parties to the conflict.
A Convenient Silence?
Between August 2009 and February 2010, the town of Al Talh came under Houthist control and the hospital where MSF was working found itself on a frontline that advanced and retreated between Al Talh and Saada city. It was hit by bullets and shell fragments on several occasions in August and September.
On 8 September 2009, the MSF hospital teams treated seven children and one woman wounded by the air strikes that hit the centre of the town. Only two of them survived their injuries. On 14 September government planes bombed Al Talh market: thirty-one wounded and nine dead were brought to the hospital. Within moments, Houthist supporters burst in, en masse, to take pictures of the wounded, until MSF teams convinced them to leave by pointing out that the presence of insurgents made the hospital a potential military target. The governmental authority in the region contacted the project coordinator several times that day, assuring her that it had not given the order to bomb, and anxious to know whether MSF was going to say anything publicly about the event. The next day, the central authorities issued a press release in which they denied any responsibilityYemen National Information Center, http://www.yemen-nic.info/news/detail.php?ID=23227. Cited in “All Quiet on the Northern Front?”, New York: Human Rights Watch, Mar. 2010, p. 29. for the air strikes. Two days later, a government plane dropped pamphlets giving the population two options: fight the rebels or leave town.
In the days that followed, the fighting around Saada intensified. MSF teams worried about the impact of the growing insecurity on their ability to continue their work at the hospital. The evacuation routes toward the capital and Saudi Arabia were becoming increasingly dangerous, and the possibility of evacuating the international staff seemed less likely with each passing day. Members of the national staff, who travelled the road between Saada and Al Talh several times a week, were being stopped and harassed by the army, and prevented from moving around. Contacted by MSF in the hopes of obtaining assurances of safety, a high-ranking Yemeni military official advised the organisation to leave. On 22 September, MSF suspended its surgical programmes and arranged to transfer patients to the Saada hospital, about fifteen kilometres away. A few days later the expatriate staff were evacuated from Al Talh, and the national staff left the hospital.
The organisation said nothing publicly about the air strikes it had witnessed, thus failing to honour the commitment that had been made by the MSF movement as a whole in 2006: “We have learned to be cautious in our actions […] without precluding MSF from denouncing grave and ignored crimes such as the bombing of civilians, attacks on hospitals and diversion of humanitarian aid. Taking a stand in reaction to such situations and confronting others with their responsibilities remains an essential role of MSF”.MSF, La Mancha Agreement, Athens, 2006.
How did MSF justify remaining silent about a serious crime that few direct witnesses relayed to the outside world?
Operational managers at MSF felt that condemning the air strikes would amount to placing blame squarely on the government, and would jeopardise MSF activities in Yemen with little clear benefit. Would speaking out about civilian deaths in the fighting prompt the combatants to show restraint in their use of violence?
More generally, in 2009, MSF was expelled from Darfur, its activities in Niger were suspended by the government and, at the time of the air strikes in Al Talh, a public statement by MSF on internment conditions for people displaced by the Sri Lankan conflict had angered the authorities there. The perceived trade-off between speech and action was being hotly debated within MSF, with some managers demanding that the organisation just keep quiet and deliver care. During an Al Jazeera interview several months earlier in the wake of the Darfur expulsion, MSF’s operations director had stated: “You have to be able to distinguish between human rights and international justice activists and relief organisations”.
MSF had little desire to risk its entire Yemen operation by denouncing a crime that didn’t affect it directly; nor did it want to demand publicly that the warring parties spare the hospital and guarantee the safety of its teams and their freedom of movement. As the fighting intensified, the teams decided to move the staff and patients to safety and evacuate the facility, saying nothing, seeing no immediate tangible benefit to speaking out. On 5 October, however, once the few caregivers who had stayed to receive patients after MSF’s departure had all left the hospital, MSF issued a statement to the national press agency and several Yemeni newspapers. Hoping to be able to relaunch its activities in Al Talh someday and fearing the hospital would be looted and bombed, it “called for respect for [Saada governorate] healthcare facilities and their purpose”—in this case, for the deserted building itself and the equipment.
Idle Words
Every year MSF compiled and published its “Top Ten Humanitarian Crises”, a public relations effort aimed at increasing its visibility in the media. December 2009 was no exception and Yemen was on the list.
In particular, MSF said that, “Violence escalated sharply in August as Yemeni army forces began carrying out air strikes and artillery assaults against Al Houthi rebels”, and reported that “tens of thousands [of civilians fled] into neighbouring Hajja, Amran, and Al Jawf governorates, where they had little to no access to healthcare services”.
The information was picked up by Al Jazeera and many other Arab media outlets. The Qatari satellite channel even ran a special edition on MSF’s statements on Yemen in December 2009, its analysts wondering publicly about the negative impact this speaking out would have on the credibility of President Saleh.
The government’s response was instantaneous. Right in the middle of the war, it immediately suspended authorisation for all of the organisation’s activities in Yemen—the movement of people and vehicles, imports, new projects, and the renewal of MSF’s framework agreement. In a meeting, government representatives laid out their main grievances to the head of mission: MSF had failed to remain neutral in the conflict by only condemning military violence and not that committed by the Houthists, and it had offered an unfounded evaluation of the healthcare services in government areas where it worked little, if at all. One of MSF’s government contacts concluded, “It was this kind of purely political report that got you expelled from Darfur”. MSF internal report, Dec. 2009.
Yet listing Yemen as one of the Top Ten Humanitarian Crises served no clear political or operational objective—other than “to attract media attention to a neglected crisis”.Interview with deputy director of communications, MSF-France, Jan. 2011.
That lack of intention and objective resulted in a vague description of the conflict and its consequences in which the government may have seen a kind of empathy with the insurgents’ cause. And the brief account did present the government as the main culprit in escalating hostilities and impeding aid, cracking down on an uprising “claiming social, economic, political, and religious marginalisation”.
The authorities were explicit regarding the terms of the negotiation: if MSF agreed to deny that the Yemeni government was creating problems of access and that there was a lack of healthcare services in government zones, and to stress that the media’s sole use of the Yemen case out of the Top Ten report reflected that same media’s viewpoint only, the government would lift the sanctions. MSF accepted the deal. In December 2009, MSF operational managers sent the Yemeni government a letter acknowledging that the report may have appeared biased, and that the issues with civilian access to healthcare services were not sufficiently documented. The national press agency issued two press releases with headlines that spoke for themselves: “MSF apologizes for ‘inaccurate’ report on Saada”, and “MSF: apology to Yemen for wrong report on the health conditions of IDPs”. These were texted to a number of Yemeni mobile phone subscribers and picked up by about twenty national media organisations and a few international news agencies. The government immediately lifted all sanctions against MSF.
When Al Talh was being shelled, MSF saw speaking out publicly as a threat to its operations, rather than as a way to pressure the government to guarantee the safety of civilians and aid teams. It would have been difficult for the government to challenge immediate and first-hand testimony by a medical organisation treating the civilian victims of the air strikes, and itself affected by the lack of safety. But the Top Ten episode—which proved how sensitive the Yemeni government was about its media image during the war—showed how vulnerable MSF can be when it speaks out without a clear political or operational objective. At that point, the association had nothing to bring to the showdown with the national authorities. It had given the government fodder for its propaganda by denying that there were problems with access to care—problems for which both the government and the rebels were to blame.
Translated from French by Nina Friedman
***
Afghanistan. Regaining Leverage
Xavier Crombé (with Michiel Hofman)
On 28 July 2004, two representatives of MSF held a press conference in Kabul to announce the organisation’s decision to pull out of Afghanistan. They explained that on 2 June five MSF aid workers had been assassinated in Badghis province and, almost two months on, the Afghan authorities in Kabul had made no attempt to arrest and prosecute the identified suspects. In addition, an alleged Taliban spokesman had claimed responsibility for the killings and justified further attacks by accusing MSF of “spying for the Americans”. These facts had led the agency to conclude that “independent humanitarian action, which involves unarmed aid workers going into areas of conflict to provide aid, has become impossible” in Afghanistan.
Although these were the main reasons for the withdrawal, the MSF spokespersons also made clear that the international forces had to share the blame for the deleterious context in which those recent events had taken place. The US-led Coalition’s systematic attempts to co-opt humanitarian aid and use it to “win hearts and minds”, they claimed, had seriously compromised humanitarian aid workers’ image of neutrality and impartiality. MSF press release, “After 24 Years of Independent Aid to the Afghan People, Doctors Without Borders Withdraws from Afghanistan Following Killings, Threats, and Insecurity”, 28 July 2004.

To many of those attending the press conference and who recalled MSF’s twenty-four years of presence in Afghanistan—including through some of the worst times the country had known—the decision came as a surprise. “Aren’t there ways for you to stay […] and deal with the security situation?” someone in the audience asked.Transcript of the press conference, July 2004, MSF archives.
In an article published in The Wall Street Journal a few weeks later, Cheryl Benard, an American scholar close to the Bush administration, had a ready solution to offer: It’s a different world out there […] The principle championed by Doctors Without Borders—that civilian professionals providing medical help to the suffering will be granted safe passage—is now part of our nostalgic past […] An objective assessment of the facts would lead organizations like Doctors Without Borders to demand more military presence, not less; closer cooperation with the military, not a separation of spheres. Alternatively, they will have to withdraw not just from Afghanistan, but also from most of the conflicts of the 21st century.Cheryl Benard, “Afghanistan Without Doctors”, The Wall Street Journal, 12 Aug. 2004. Cheryl Benard’s husband was then the US ambassador to Afghanistan.
“In the ‘war against terror’, all factions want us to choose sides”, the president of the International Council of MSF fired back. “Ms. Benard’s ‘objective assessment’ […] is merely another example of this logic. We refuse to choose sides”. Dr Rowan Gillies, “The Real Reasons MSF left Afghanistan”, letter to the editor, The Wall Street Journal, 19 Aug. 2004.
The controversy was not new. It had been raging ever since the Bush administration had launched Operation Enduring Freedom (OEF) in Afghanistan in retaliation for the September 11 attacks on American soil and had called on humanitarian NGOs to join in the war effort. Yet, in the months that preceded the killing of its personnel, MSF found itself in an ambivalent position where the western forces and Afghan authorities it wanted to distance itself from were, in effect, its main interlocutors. While opting out of the reconstruction plan designed by an “international community” in open support of the Karzai government, MSF had had no contact with the armed opposition since the fall of the Taliban regime and had considerably reduced its programmes, including in those areas where the insurgency was reportedly gaining ground. The legitimacy that many at MSF felt they deserved, given the organisation’s twenty years of history in Afghanistan, was not enough to secure respect for a “humanitarian exception” increasingly at odds with the agenda of the main political, military and aid players on the Afghan scene.
What made it possible then for MSF to return to Afghanistan in 2009 and relaunch programmes, not only in Kabul, but also in Helmand province, one of the areas most contested by western troops, the Afghan security apparatus and armed opposition groups? The deadliest year for aid workers had been 2008, and 2009 saw civilian and military casualties reach unprecedented levels. In short, there had been no magical re-opening of the “humanitarian space”. Yet, the “different world out there” had grown to have implications quite opposite to those asserted by Cheryl Benard only a few years previously. As this chapter argues, the evolution in the dynamics of the conflict and the interests of the various players in Afghanistan have contributed to reestablishing the relevance of MSF’s services, granting it renewed leverage to negotiate access to people caught up in war.
Unlike usual representations of humanitarian action—associated with emergency intervention and rapid deployment of resources—the following account shows the ongoing process of reinserting MSF into the Afghan field to be a long and sustained effort to identify and engage negotiating interlocutors on all sides and at all levels along their respective line of command.
“A Different World Out There?”
The most obvious change in the wake of September 11 was that, after years of neglect, Afghanistan was to become the theatre of major and direct intervention by western armed forces. Initially MSF did not have much to say about the US-led OEF, endorsed by the United Nations in the name of legitimate self-defence. As several voices in the international MSF movement stated, the role of a humanitarian agency is not to judge the reasons or objectives of a war, but rather the means used to carry it out. In this respect, the Bush administration’s rhetoric of “infinite justice” and “war against terrorism”, its reference to NGOs as a “force multiplier” for the US armyComment made by Colin Powell at a State Department press conference, Washington DC, 26 Oct. 2001 and its rejection of the applicability of international humanitarian law to “enemy combatants”, soon caused concern. In the first phase of the war, however, calls for restraint and respect for the distinction between military and humanitarian responsibilitiesFor instance: MSF press release, “Médecins Sans Frontières casts doubt on military’s ‘humanitarian airdrops’ in Afghanistan”, 8 Oct. 2001; Rony Brauman, “Des mots magiques aux cruelles désillusions”, Le Monde, Nov. 22, 2001. carried little weight. All the more so as MSF, like most humanitarian agencies, had all but evacuated Afghanistan before the start of the US bombing campaign when the Taliban regime warned it could no longer guarantee the safety of foreign aid workers. Further undermining the relevance of the humanitarian voice at that stage, the expectation of a refugee crisis and of the subsequent emergency needs that had led to massive deployments of aid at the borders of the country proved unfounded.
When, in November 2001, MSF expatriate teams returned to Afghanistan only days after the fall of the Taliban government and the seizure of Kabul by the Northern Alliance, there was no significant emergency situation to address. And, when a few weeks later reports emerged of alleged war crimes by the US army and its Afghan allies— notably the bombing of Taliban prisoners in the prison of Qala-e-Jangi— the MSF movement did not set itself apart from the international community’s muted reactions. No consensus could be reached between those who considered a public denunciation of these crimes to be part of the organisation’s legitimate role and those who feared it would be seen as overly political, particularly as no humanitarian worker had actually witnessed the events.See Jean-Hervé Bradol, “Questions gênantes à une coalition au-dessus de tout soupçon”, La Croix, 17 Dec. 2001 and MSF-France president’s Moral Report, May, 2002, MSF archives.
Over the following year, the MSF sections that had been present in Afghanistan prior to the Coalition’s intervention resumed most of their previous programmes as security conditions allowed. With operations in fifteen provinces by the end of 2002, the MSF movement could again claim to be one of the leading healthcare providers in the country, as it had been for most of the previous decade. However, the implications of such a role were soon to become a problem. With funds now available from a variety of state donors anxious to show their contribution to the American effort, the aid community began to soar. The United Nations agencies were now under the authority of the UN Assistance Mission to Afghanistan (UNAMA) headed by Lakhdar Brahimi. The country was to be the test case for the new integrated approach to UN peace operations that Brahimi himself had played a leading role in designing. Politics and aid were now integrated into the same structure, with politics firmly in the driving seat. This soon translated into an endorsement of the Coalition’s military objectives and a requirement that the aid programmes serve the goal of strengthening the legitimacy of the new Afghan government which had emerged from the December 2001 Bonn Agreement.
For the main donors—the United States, the European Commission and the World Bank—health was a prime locus of political legitimacy and a multi-million dollar programme was established in 2003 to allocate the provision of basic healthcare in rural areas of entire provinces to NGOs selected by the Afghan Ministry of Public Health (MOPH) and international donors. The health programme, consistent with the general shift of donor funding towards long-term reconstruction aid, signalled the political will to portray Afghanistan as a “post-conflict” environment. The US army had already delivered this message in November 2002 when it announced the creation of Provincial Reconstruction Teams (PRT), mixed civil-military units “designed to improve security, extend the reach of the Afghan government and facilitate reconstruction in priority provinces”.Department of State, Department of Defense, USAID, Provincial Reconstruction Teams in Afghanistan: An Interagency Assessment, June 2006, p. 10.
While the aid community, which by mid-2003 amounted to 200 international NGOs and private companies and 800 Afghan organisations, for the main part rejected the PRT’s offer to coordinate their actions, most of them readily signed up to the donors’ scheme which effectively made them “implementing partners” of the Kabul administration in return for funds.
MSF Leaving Afghanistan: No Compromise Possible
Disbelief was probably the overwhelming feeling of the MSF teams at the time, regarding both the “post-conflict mood” of the international stakeholders and the stated ambitions of development health policies that combined de facto privatisation with bureaucratic control by weak government institutions. Refusing publicly to participate in the reconstruction-funding scheme, they declared instead that the ongoing conflict involving international forces, whether part of the US-led Coalition or the UN-mandated International Security Assistance Force (ISAF), justified the sustained provision of independent and impartial humanitarian assistance.
Although the five MSF sections were united in this position of principle, they were less consistent in translating it into operational terms. By then, most of their programmes were located in relatively stable areas in the centre and north of Afghanistan where they met with the typical uncertainty, associated with “neither war nor peace” situations, as to what distinguished humanitarian medical aid from development-oriented health projects. Throughout 2003 and early 2004, a number of MSF-supported health facilities were handed over to other NGOs or officially to the Afghan Health Ministry. At the same time, MSF attempted to identify what were termed “unaddressed medical needs”, such as tuberculosis or malaria, in an effort to retain a useful medical role on the sidelines of the national health policies. Limited in size, such programmes were no doubt of value to their direct beneficiaries, but were of little interest to the Karzai administration and its international backers who were bent on demonstrating quick results on a large scale.
While weakening its position vis-à-vis the Afghan government, MSF’s operational choices could hardly appeal to the armed opposition and convince it of the agency’s neutrality. Despite maintaining medical programmes in the southern cities of Kandahar and Ghazni, MSF had little visibility or impact on the effects of the relatively silent war building up in the surrounding areas. In fact, it had made no real attempt to restore contact with the Taliban since their fall from power. The murder in Uruzgan province of an ICRC delegate ordered by a Taliban commander in March 2003 made that option even harder to envisage and contributed a few months later to MSF’s decision to withdraw its expatriate staff from Ghazni. But the Taliban were not the only threat hanging over humanitarian organisations: they were also easy targets for disgruntled warlords acting as “spoilers” to assert their power and influence and this, in all evidence, accounted for the assassination of the MSF personnel in Badghis province. In spite of all the arguments put forward at the press conference to justify its departure from the country, the killing was felt by many within the MSF movement to be a tragic conclusion to an ongoing process of retreat.
It was, in fact, not the first time the relevance and viability of the organisation’s operations had been called into question in Afghanistan. The significance of MSF’s cross-border missions in the country in the 1980s was based on a powerful symbol: the “French doctors” were one-sided in their public denunciation of the Soviet occupier’s war crimes and the medical aid provided to populations in areas controlled by the mujahedeen displayed solidarity with their cause. Jihad party leaders and local commanders granted the MSF teams protection in return for the assistance they provided to their constituency and for the financial and military support from western states some of them hoped the visible presence of MSF would favour. With the Soviet Union gone and vast US funds having spurred corruption and rivalry among party leaders and the hundreds of aid agencies present in the refugee camps in Pakistan, Fiona Terry, Condemned to Repeat? The Paradox of Humanitarian Action, London: Cornell University Press, 2002, pp. 71–80; Olivier Roy, “L’humanitaire en Afghanistan: entre illusions, grands desseins politiques et bricolage”, CEMOTI, No. 29, Jan.–June 2000, pp. 21–30. the pertinence of the small MSF medical teams started to fade. Amid growing disagreements within the organisation over the nature and impartiality of its operations, tensions with mujahedeen escortsMSF-France president’s Moral Report, 1989, MSF archives. and security incidents escalated until the murder of an MSF expatriate in a clinic in Badakhshan province led to the closure of all programmes in Afghanistan in 1990.
When MSF returned after the fall of the communist regime in 1992, it addressed a very different context with very different means. Initiating operations in Kabul, now the scene of an all-out civil war among the different factions, the organisation was able to make use of the logistical capacity developed during the previous decade in other set-tings—cars, radios and the airlifting of medical supplies. Size of operations mattered more than symbols at the time and it was the presence of three to four MSF sections across the country’s multiple frontlines that enabled the organisation to earn its reputation and acceptance. Yet, in early 2001, the relative peace imposed by the Taliban and the destitution in the country, submitted to harsh rule and international sanctions, led to growing unease regarding MSF’s continued presence.
An Invitation to Return
Between 2004 and 2008, two significant developments opened the way for some in MSF to reconsider options for a return to Afghanistan. Firstly, it was not long before the “post-conflict” success story started to unravel. Over-confident and anxious to reallocate forces to Iraq, the Bush administration unilaterally decided to reduce US troops in the south and called on its ill-prepared NATO allies to take over. This was the opportunity for the armed opposition based in Pakistan to launch a major offensive in the spring of 2006. Ahmed Rashid, Descent into Chaos. How the War Against Islamic Extremism is Being Lost in Pakistan, Afghanistan and Central Asia, London: Penguin Books, 2008.
In their heartland, the various arms of the Taliban were able to build on the population’s growing discontent with the corruption of the government and its local officials, the lack of effective public services in the provinces and resentment against the foreign presence. Their influence gradually extended to other parts of the country, including the north. Gilles Dorronsoro, The Taliban’s Winning Strategy in Afghanistan, Washington: Carnegie Endowment for International Peace, 2009.
The international forces’ response relied heavily on aerial bombing, resulting in high death tolls among civilians and still further alienation. As revealed in a UNAMA human rights report, civilian casualties caused by armed opposition groups in 2008 only slightly outnumbered those caused by “pro-government forces”, two-thirds of which were due to air strikes. That same year, thirty-eight aid workers were killed and 147 kidnapped, leading the UNAMA to conclude that “humanitarian space had shrunk considerably”. UNAMA, Afghanistan: Annual Report on Protection of Civilians in Armed Conflict, 2008, Kabul: United Nations, 2009.
The report signalled a belated realisation by the UN and aid groups of the price being paid for their years of association with the post-conflict agenda of these same “pro-government forces”.
Secondly, and in opposition to the first development, the ICRC had undertaken, during the same period, a unique endeavour to restore dialogue with the armed opposition and to gain recognition of its neutrality. The assassination of its delegate in 2003, followed a few months later by the murderous attack on its delegation in Iraq, had led to much soul-searching within the ICRC. In 2004, while MSF was deciding to withdraw from Afghanistan, the ICRC instead began to make use of the wide range of activities included in its mandate, such as access to detainees, orthopaedic programmes and donations, to demonstrate its operational relevance to the opposition and open up channels of communication with its leadership. The ICRC’s approach received its first public recognition in August 2007, when the Taliban granted the organisation a mediation role in the negotiations leading to the release of South Korean hostages. ICRC news release, “Afghanistan: ICRC facilitates release of twelve South Korean hostages”, 29 Aug. 2007.
It was right in the middle of this hostage crisis that an MSF team carried out an assessment in Afghanistan. Its findings conveyed the sense that innovative approaches were needed if MSF was to return to the country. Given the context, the standard practice of having several autonomous sections in the field and programmes run by expatriate staff prone to a high turnover was cause for concern, but much uncertainty remained among MSF sections over what an acceptable alternative could be. With the war now in the open, internal discussion gained momentum in 2008, thanks to a large extent to the ICRC’s readiness to share its experience with MSF and facilitate the organisation’s return through contacts and advice. The armed opposition appeared to be asking for increased medical assistance for its combatants and the people in the war zones, and the ICRC wished to have other humanitarian actors in the field to help meet the growing needs stemming from the conflict. For MSF to gain credibility with the opposition, ICRC delegates warned, its operations must reach a “critical mass”, but having several sections and representations as in the past might jeopardise the ability to develop a reliable network of contacts.
Despite persistent security concerns, these recommendations and offers of support helped to strengthen the case for a return within MSF. There was now a consensus on the necessity for a single representation and, to this end, it was the Belgium section of MSF that was selected to conduct negotiations and assume full operational responsibility in Afghanistan on behalf of the movement for a period of two years. At the same time, preliminary contacts were made with representatives of the armed opposition over the course of 2008, during which the Tali-ban denied responsibility for the Badghis murders. Although the level of authority and influence of these contacts was still unclear, they seemed to confirm the ICRC’s analysis that the armed opposition was now seeing more potential benefits in securing access to medical aid for themselves and their social base than in preventing it. It was now up to the designated operational team to develop a pertinent humanitarian role for MSF in Afghanistan.
Finding Common Ground with the Afghan Government
The broad outline of the operational strategy was set out in February 2009, at the end of a ten-day visit to Kabul led by the newly appointed head of mission. He recommended that the mission be geared toward providing medical care in areas where the health system had been the most disrupted by the conflict. In spite of the lack of reliable data, the war-torn areas in the south and east of the country appeared to be most in need, but accessing them could only be seen as a medium-term objective. Security conditions made travel by road to these areas all but impossible—not only for expatriates but also for Afghans from other parts of the country—let alone conducting health assessments. From the political point of view, these assessments risked being perceived as undermining the Kabul government’s authority. According to the official line supported by the international donors and their “implementing partners”, the primary healthcare funding programme was now successfully covering 85% of the country’s rural districts, a figure based on funds disbursed rather than on effectively running health facilities. It was therefore preferable for MSF to opt for less sensitive operations as a first step to gaining credibility and to develop a reliable local network that would help achieve its longer-term goal. The head of mission recommended focusing on improving secondary healthcare in towns either close to conflict zones or accessible by plane. This would respond to an obvious medical need, since the hospitals in many provincial capitals, and even Kabul, had largely been excluded from donor funding, and it would enable expatriate teams to be sent to the field. The presence of expatriates, albeit limited in number and confined to their accommodation and places of work, was deemed necessary to ensure effective monitoring of the activities but, above all, to conduct direct negotiations with the warring parties, as recommended by the ICRC. “As expectations are high from all sides it will be important to have ‘something to show for’ reasonably quickly, but also clearly aimed at different parts of the country and different populations”, the head of mission noted in his report. MSF internal report, “Strategic choices for MSF in Afghanistan”, Feb. 2009, MSF archives.
It was thus decided that MSF would support two public hospitals. One was Boost provincial hospital in Lashkar Gah, the capital city of Helmand province, a region where intense fighting had been taking place for several years between the international forces, the Afghan army and the armed opposition; the other was a district hospital in the east suburb of Kabul, an area which was drawing a growing number of migrants and displaced people. By opting for existing public health structures rather than setting up independently-run MSF facilities, the organisation’s coordination team hoped to facilitate the negotiation process with the Kabul government on which it depended for visas, work permits and authorisations to import medical equipment, allowing MSF to start operations quickly. As Helmand province was the stronghold of the insurgency and MSF’s opposition contacts had expressed an interest in setting up medical programmes in Kabul, it was assumed the two locations could appeal to both sides in the conflict.
As for the Afghan government, political timing played in MSF’s favour. Since its departure, the authorities had drawn up new regulations with the tacit support of the UNAMA and international donors to strengthen their control over the NGO community. The NGOs involved in medical activities now had no alternative but to become subcontractors of the Ministry of Public Health (MOPH), through which donor funding was channelled. Yet, with the upcoming presidential election scheduled for the summer and his position at stake, the minister of health saw in MSF’s planned operations a way to improve his image. He was therefore willing to exempt the organisation from the subcontracting framework and to press other government departments to legally register MSF in the country. The Memorandums of Understanding (MoUs) for the projects were the subject of little discussion and both were signed on 30 June 2009. The Afghan press agency reported the event in two separate press releases, which left little doubt as to the different positions of the two signatories. In one of them, the minister of health was quoted as saying: “We invited MSF to resume activities in Afghanistan and assured them the government will provide every facility and opportunity to it to implement the [national] strategies”. “Health Ministry, MSF ink MoUs”, Pahjwok Afghan News, 30 June 2009.
The other one, actively solicited by MSF to counterbalance the MOPH’s public relations exercise, cited the head of mission: “MSF will rely solely on private donations, thus safeguarding its independence from political and military powers”. “MSF to support 2 hospitals”, Pahjwok Afghan News, 30 June 2009.
The provisions of the two MoUs gave MSF control over its medical activities and stipulated the application of humanitarian law within the healthcare facilities. While it was agreed that MSF would provide medical assistance “in support of” the MOPH in the two hospitals, drugs and equipment were to stay under MSF supervision right to the patient and all services were to be provided free of charge. Weapons were prohibited within hospital compounds, which from then on would be under the control of MSF-employed guards. Any third-party support for the hospital, notably by international forces, was to be subject to prior agreement. Lastly, in keeping with the Geneva Conventions, patients were not to be harassed or arrested by security forces during treatment and, as long they were not deemed medically fit, to be subjected to interrogation. As for the medical staff, they could not be prosecuted for treating patients, whoever they were. Memorandum of Understanding between the Ministry of Public Health, Islamic Republic of Afghanistan and Médecins Sans Frontières, 2009.
Disarming International Forces in Health Facilities
Enforcement of these clauses entailed further negotiations, however, especially in the case of Boost hospital in Lashkar Gah. British troops from the ISAF (International Security Assistance Force), private security companies protecting British government development officials, the police, the army and the Afghan secret services—the National Directorate for Security (NDS)—were used to moving around freely and heavily armed inside the hospital premises. While the MoU was effective in getting the Afghan police and army to put a stop to the practice, the others would only comply if ordered to do so by their hierarchy.
Negotiations with the international forces thus started by establishing contact with the British authorities. The coordination team initiated the process in Kabul through meetings with the British ambassador before going to London to meet with the relevant inter-ministerial and military departments. These negotiations enabled MSF to obtain the suspension of the PRT’s activities and the definitive withdrawal of soldiers from the hospital. Then, in August 2009, MSF’s US-based section set up a series of meetings with US officials from the State Department in Washington and the US military Central Command (CentCom) in Florida. The objectives of the MSF delegation were to inform the US political and military leadership of the medical programmes it planned to develop in Afghanistan and to request that all military forces under US command, including Special Forces, respect the protected status of the MSF medical mission. At the time of the visit, the still-new Obama administration was preparing a second strategic review of the war in Afghanistan. General McChrystal, appointed commander of US and NATO forces in Afghanistan in June, was finalising his assessment of the situation, which was rumoured to be grim. For all that, the US government’s public relations policy towards NGOs seemed to have changed little since 2001. In April 2009, Richard Holbrooke, United States special envoy for Afghanistan and Pakistan, had claimed “90% of US knowledge about Afghanistan lies with aid groups” “Envoy laments weak US knowledge about Taliban”, Associated Press, 7 Apr. 2009. and at the beginning of August, General Petraeus had promoted a new “Civil-Military Fusion Centre” “Rising threat to aid agencies in Afghanistan”, Global Post, 18 Sept. 2009. to a panel of UN diplomats and NGOs in Geneva. Nonetheless, State Department and CentCom officials did recognise MSF’s need for security guarantees from all the parties to the conflict. In sharp contrast with the usual reactions from the PRT officers in the field, they made no objection to the remark made by the representatives of the organisation that, from a humanitarian perspective, MSF made no difference between its relations with the US military and with the Taliban.
The meetings did not result in any formal commitment, but MSF’s objectives appeared to have been met in the field. In the autumn of 2009, “US troops stormed Afghan hospital, aid group says”, CNN.com, 7 Sept. 2009. ISAF troops raided several health facilities run by international NGOs, but no such incident has taken place in MSF-supported hospitals. The international negotiations may have incidentally led to other benefits. In October, the NDS general in Helmand informed the head of mission that he had received new instructions from Kabul and ordered his staff “to start application of international humanitarian law in Boost Hospital”, before adding “the hospital should be a safe place for all patients, whether they are associated with the opposition or not”. MSF Afghanistan Situational Report, Oct. 2009, MSF archives.
Engaging with the Opposition
Full compliance with MSF’s “no weapon” policy was to be the starting point for the medical programmes. They were launched officially in Kabul in October, but remained effectively on hold in Lashkar Gah until January 2010. The teams were on the wards, but had to wait for drug supplies to arrive as their transport by truck from Kabul to Helmand depended on obtaining permission from the Islamic Emirates of Afghanistan (IEA), the most influential armed opposition group, also known as “Quetta Shura”. This was in essence a sovereignty issue, as most districts in the southern provinces, and consequently road traffic, were under effective control of this group.
Since MSF’s return to Afghanistan, there had been several setbacks in engaging the Taliban leadership. Getting approval for the Kabul project had been relatively straightforward as MSF’s initial opposition contacts judged the selected hospital located in a Pashtun area to be easily accessible by their constituency, and planned surgical activities opened up the prospect of treatment for their wounded combatants. But the scant interest and commitment they had shown from the outset regarding MSF’s intended projects in the southern provinces, including Helmand, known to be the heartland of the IEA, had cast doubts over the breadth of their connections.
Hence, in the spring of 2009, MSF set about establishing different contacts with the opposition, this time relying on its own network of former Afghan staff and, by the summer, had been able to initiate communication with known IEA members. Right from their first discussions, these new interlocutors made clear to MSF that its earlier contacts were not legitimate representatives of their group. Their connections lay instead with the Haqqani Network, whose influence extended over Kabul and Afghanistan’s southeast, as well as the Waziristan region in Pakistan. The IEA was rooted in the south but was also influential in the rising insurgencies in the west and north. The two groups were partner organisations, but they had distinct constituencies and interests. From then on, the two channels should be engaged separately for negotiation, depending on the area at stake.
While MSF had been successful in expanding its network, time had nonetheless been lost in identifying the right contacts to secure guarantees in Helmand. Moreover, soon after a first and promising encounter, the organisation was informed that the IEA council had rejected its two projects, on the grounds that working in MOPH facilities displayed unacceptable support for the Karzai government, derisively referred to as the “Labour Department” of the American forces. This decision effectively prohibited the safe transport of drugs by road from Kabul to Helmand.
It took six more months to resolve the issue. MSF defended its operational choice as a necessary first step to import drugs and insisted that, with its teams already on the ground and drugs waiting in Kabul, it was too late to cut the project short. Assessments for future projects, MSF argued, would consider areas suggested by the IEA. The agency also stressed it had received assurances from foreign and Afghan forces that they would not interfere in the hospitals. On the part of the IEA, security considerations were inseparable from issues of legitimacy and the authorisation for the transport of drugs MSF was asking for was used as a bargaining chip to extract further guarantees and concessions from the organisation. Airing their distrust of the MOPH doctors in Lashkar Gah and of US respect for the Geneva Conventions, the opposition demanded that MSF give a commitment in writing stating that it had control over the hospital staff and provide an official MoU with the US military to prove their compliance with humanitarian law. MSF was careful not to commit itself regarding the behaviour of the international forces, stressing instead its ability to hold them to account through the media.
In January 2010, the IEA eventually gave permission for the drugs to be transported to Helmand. Wishing to be recognised as an able and legitimate government in the regions where they were gradually gaining control, the opposition leadership was seemingly more interested in medical aid as a tool to win “hearts and minds” than as an actual asset for their combatants. When MSF asked if the IEA had suggestions for future projects, one representative answered: “The biggest needs are with civilians, especially maternity care; we can take care of our fighters”.
Improving the Quality of Care
The launching of medical activities didn’t mean negotiations were over for MSF. At Boost hospital, they were now held on a daily basis between the expatriate team and the local medical staff. Prior to the organisation’s arrival, the doctors and nurses had used the provincial hospital as a waiting room for their own private clinics in Lashkar Gah. Even if they hoped to benefit from MSF’s support of Boost, many of the provisions they had agreed to during the MoU negotiations in Kabul went against their own business interests, which were potentially threatened by the drugs and treatment now available free of charge at the hospital. The MSF team’s effort to organise fixed working hours to ensure continuity of care for patients also created tension as the local doctors resisted being kept away from their highly profitable private practices. These habits and vested interests were hard to change, to the detriment of the quality of care. Negotiations on setting up good management of the hospital were all the more difficult to conduct during the early stages of the project as, in a dangerous environment where MSF was a newcomer, the expatriate team was small and could not take the risk of alienating the local medical team.
By the end of 2010, the mission coordinators considered they had enough guarantees to expand the international medical team in Lashkar Gah. MSF’s credibility with the population and the local armed groups required rapid improvement in the services provided by the hospital, all the more so as the issue of quality of care was compounded by that of access. In November 2010, a patient survey concluded that the majority of people in Helmand could neither afford nor risk going to Boost hospital for treatment. Taking a taxi from the districts to the city cost an average of 100 dollars and mines, fighting and intimidation were constant threats that few people would risk, even in cases of dire emergency. The high profile operation carried out by international troops in Helmand province in the spring—part of the “surge” decreed by the Obama administration—had obviously done little to improve the situation. “We’re between two forces”, one man complained to the survey team, “the Taliban say don’t go out at night, the British army patrol checks us during the day”. An old man from the Taliban-controlled district of Nawzad was recorded as saying, “They will not stop their fighting for our patients. They are killing each other by the hundreds, why would they stop for just one patient?” Commenting on Boost hospital, he added: “I don’t see any weapons here—that means you don’t have any problems with the Taliban”. Statements such as these came as an endorsement of MSF’s approach; they also confirmed the necessity for the team in Lashkar Gah to develop contacts with local opposition leaders in order to gain access to those districts thought to be most affected by the conflict. But as the old man interviewed in the survey concluded: “The Taliban is not under one command. It might be all right for you to be here, but can you come to my district?”Quotes from MSF internal report, “The challenges in accessing Boost hospital in Lashkargah city, Helmand province”, Nov. 2010.
Indeed, divisions among opposition commanders in Helmand have up until today prevented MSF from getting the agreements and security guarantees that would allow it to do so.
Scaling Up
A common downside of supporting public structures, the operational difficulties encountered in Boost hospital in Lashkar Gah did not come as a surprise to the mission’s coordinators. They had resigned themselves to this option in order to be able to secure the authorisations from the Afghan government that would afford them more latitude with other programmes as quickly as possible. After the first round of negotiations, expectations ran high among the leaders of the armed opposition for the opening of new projects in the regions under their control. While seeking to consolidate its existing programmes, MSF thus undertook, as early as the spring of 2010, to assess new areas for interventions, hoping they could be set up in independent facilities. The two provinces chosen for this second operational phase were Khost and Kunduz.
The heartland of the Haqqani network in southeast Afghanistan, Khost was also the location of the main OEF (Operation Enduring Freedom) base in the country from where counter-terrorism operations across the border with Pakistan were carried out. Suspicions were therefore running high when the MSF team met with the elders of the local tribes, but the organisation’s Haqqani contacts and the unique asset it had to offer helped to build confidence. In line with the available health data, the elders expressed a need for mother and child healthcare. MSF could set up a programme involving female expatriates, which, as the elders had to acknowledge, was the only way to ensure that local women would be cared for. Emboldened by this perspective, one of the elders suggested including mental health in the programme to address what he saw as a worrying trend of suicides among women in the region. For an expatriate team to be able to settle in the town of Khost and launch such a programme, MSF first had to undertake a new round of negotiations to obtain security guarantees from all the warring parties.
Access to the city of Kunduz was less of a security issue, but the situation in the districts was a different matter altogether. Kunduz had been the first northern province where the IEA had expanded its influence and fighting had increased over the previous year. As armed confrontation was a relatively recent phenomenon, the local health system had not yet experienced the same disruption seen in the southern provinces such as Helmand. But Kunduz had become a strategic location; a new supply route for international forces crossing the province from Tajikistan and a recent arrival of American troops under OEF command were creating widespread anticipation of an upcoming escalation in the conflict.
MSF’s assessment therefore concluded that a medical presence should be negotiated as soon as possible, so as to be able to provide a timely and appropriate response to the consequences of the expected increase in violence. An expatriate team was positioned in the town of Kunduz to initiate discussions with the many local armed groups upon whom access to the districts was dependent. It was later decided to set up a trauma centre in the provincial capital to cater to the direct victims of the conflict. The project was to be housed in a private building to ensure full independence. In December 2010, the Kunduz authorities approved the project. But the war had flared up more quickly than anticipated with fighting and suicide bombings killing many of MSF’s contacts in government and the opposition alike. This further complicated negotiations, and still the conditions for the organisation to start its project had not been met. In particular, without agreement on a referral system allowing wounded patients to be taken in safety from the districts to the MSF facility without risk of arrest or attack, not all the parties would be able to benefit from the project.
Negotiations regarding MSF’s intervention in the provinces of Khost and Kunduz are still ongoing in the spring of 2011, at a time when domestic and international pressure on the Karzai government, the increasing stakes in the political negotiations between the belligerents and the Obama administration’s commitment to begin withdrawing US troops in the summer, are all bringing about rapid changes in the political and military environment in Afghanistan. In this context, expectations weighing on MSF remain high. As a representative of the IEA bluntly put it: “We cannot guarantee your safety if you don’t produce some real work”.
When the two MSF members conducting an assessment mission in July 2007 met with various departments of the Karzai government, they noted that for all the expressions of welcome they received, there was a degree of ambivalence regarding the possibility of the medical agency coming back to Afghanistan: “MSF represents the past, the war and in different ministries there are also concerns and misunderstanding […]. [Some officials] make clearly the link between our return and a deterioration of the situation in the South”.Assessment visit report, “Afghanistan: What humanitarian space and role for Médecins Sans Frontières?” Aug. 2007, MSF archives.
Again, in December 2010, as the Kunduz provincial authorities were about to sign the agreement authorising MSF to start its war-wounded programme, an official remarked in essence that he saw MSF’s return to the province as both a good sign and a bad sign.
These remarks point to the same evidence, namely that humanitarian action is a symptom of war, not a cure—of war, at least. They also highlight what this chapter has attempted to show: for MSF’s action to be accepted, the main political and military stakeholders in the war have to recognise the conflict as such and to have an interest in the medical services the agency can deliver. The situation prevailing in Afghanistan today is no less polarised than it was when MSF left the country in 2004 and it is no doubt far more violent. The key change from the perspective of the humanitarian actor is that medical operations in conflict-ridden areas are now seen by the competing warring-parties as building, to varying degrees, their own claim for legitimacy.
MSF has been able so far to play along with these evolving perceptions by demonstrating that its medical assistance could appeal to each side. It remains no doubt a fragile equation, which to date has allowed little improvement in access to the population trapped in war-affected rural areas. To be sure, the current scaling-up phase does contribute to a higher standing for MSF in the eyes of its high level interlocutors, but for this to last, continuity in interactions and perceived interests is crucial. This in turn depends not only on MSF’s negotiating skills but even more so on the dynamics of the war—or of a violent peace. Therefore, rather than trying to gauge the size of the “humanitarian space” in Afghanistan, it may well be more accurate to consider the passing opportunities and risks of this humanitarian moment.
***
Pakistan. The Other Side of the Coin
Jonathan Whittall
Between 2008 and 2010, internal conflicts and the so-called “global war on terror” in the northwest regions of Pakistan led to the displacement of 4.2 million people.International Crisis Group, Pakistan: The Worsening IDP Crisis, Asia Briefing, Islamabad/Brussels: ICG, 16 Sept. 2010.
Since 2007, the people in the Federally Administered Tribal Areas (FATA) and Khyber Pakhtunkhwa Province (KPK)Formerly called North-West Frontier Province (NWFP). have been living with the threat of fighting between the Pakistani army and armed opposition groups such as Tehrik-el-Taliban Pakistan (TTP), US drone attacks and sectarian violence. The Afghan Taliban now use the FATA region that borders Afghanistan as a launching pad for its operations against the Coalition forces. The TTP also uses the FATA as a base for its attacks against the Pakistani state. Given its very limited access to the tribal areas, MSF knows little about the population’s medical needs. Most of MSF’s programmes are confined to the province of KPK, close to the FATA, where the army allows the organisation to address the inadequacies in hospital services. However, the need for medical assistance is in all probability even more vital in the FATA where health workers are often unwilling to work due to the lack of security. MSF’s position in Pakistan has been largely based on its principles of independence, neutrality and impartiality— which have been implemented through its decision not to accept any funding from governments for its operations in the region. The organisation has made every effort to distinguish itself from the counter insurgency humanitarianism promoted by the authorities. But how successful have these efforts been in securing access to the most vulnerable populations?
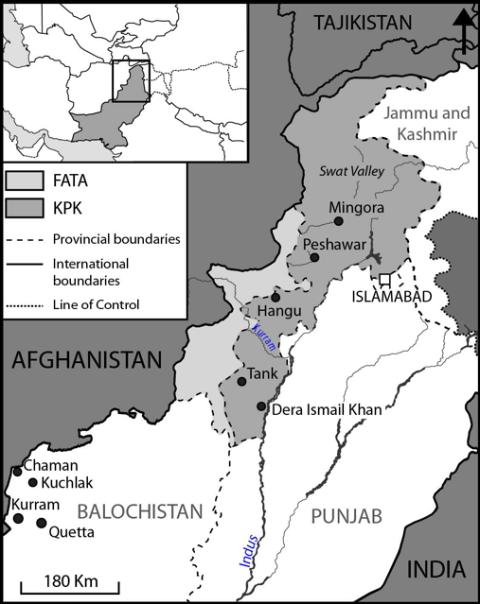
In northwestern Pakistan, the army and international donors accord humanitarian aid a pivotal role in their “stabilisation” strategy intended to establish the government’s legitimacy. In practice, counter-insurgency (COIN) priorities determine where national and international aid is delivered and who receives it. The army denies humanitarian organisations access to regions where it is conducting counter-insurgency operations until such a time as the area is pronounced “cleared” and ready for “reconstruction”. This is the case for all of the FATA as it was for the districts of Dera Ismael Khan and Tank in KPK in 2010, where displaced people had gathered. In 2009 and 2010, MSF made an attempt in vain to support the health facilities in Dera Ismael Khan. Even after the floods of 2010, these areas remained off limits to MSF despite the increase in need for healthcare assistance. The official explanation given to MSF by the army was its inability to ensure the safety of international staff. But as of 2009, the army has prohibited all discussion between MSF and the TTP, even if only to negotiate guarantees of security that it couldn’t deliver itself.
Although the army responded to the food, shelter and healthcare needs of the people displaced by its military operations, there was a significant lack in the delivery of assistance, particularly to those communities considered as having links to “terrorists”. A collective punishment enshrined in the Frontier Crimes Regulation Act (FCR) results in aid being distributed according to region of origin rather than need. Areas that people have fled from have to be “notified” as “affected” before a person can be considered for assistance. Khyber Agency in the FATA is an example; never having been officially recognised as “affected” by conflict, the internally displaced people (IDPs) there have received almost no assistance.
This manipulation of aid has been largely supported by the United States and the United Nations, which, in effect, endorse Pakistan’s stabilisation policy. As illustrated by the UN’s 2010 Humanitarian Response Plan, which was introduced by a letter from the Pakistani government explaining its counter-insurgency activities in KhyberPakhtunkhwa/FATA, the UN and even its specialised agencies such as the HCR and WFP are clearly supporting one of the parties to the conflict. In addition, US funding is allocated according to objectives of “stabilisation through development” to which the “capacity building” actions of many NGOs contribute—often to the detriment of the capacity for emergency response.
According to one IDP interviewed in March 2010, “America is paying the people who are fighting against us and destroying our homes [referring to the Pakistani army] and then they are giving the relief. We don’t trust that”.IDP Summer Bagh Camp, 10 Mar. 2010.
Based on MSF’s experience in the region, such suspicion is widespread and has consequences on the ability of the broader NGO community to respond. Aware of the mistrust of the armed opposition groups and part of the population due to NGO links to US funding and the UN, many NGOs often restrict their interventions to areas where they don’t run the risk of becoming targets.
In this context, MSF tried to move way from a role of assisting the counter-insurgency and stabilisation strategy in the region by extending its programmes to “non-cleared” areas and “terrorist populations”. The main challenge was to gain the acceptance of all the different political and military agents—those who either supported or opposed the government. This tension was well illustrated by MSF’s response to the healthcare situation in Swat.
MSF and US-Supported Stabilisation in Swat
MSF first worked in the Swat valley in KPK province in 2008 to 2009 when the armed opposition groups were in control of the area. Pakistani nationals ran operations with the support of international staff who made occasional visits. In order to be authorised to work in the valley, the Pakistani authorities demanded that MSF obtain security clearance from the opposition. The organisation had direct access to the opposition high command who themselves maintained dialogue with the state at that time. MSFs strategic partnership with the Swat Doctors Society, the supply of medicines and equipment for emergency rooms, and the setting up of an ambulance service enhanced the reputation of the organisation as a recognised medical service provider. MSF accepted to intervene without the presence of any international staff, as the parties involved in the conflict did not want to be responsible for the security of expatriates. This compromise was made because it was possible to talk to the opposition. Following a series of security incidents, which included the murder of two MSF staff in a clearly marked ambulance, MSF was forced to close its projects in the district in May 2009.
Between May and July 2009, the Pakistani army launched a major offensive in the Swat valley which caused the displacement of over three million people and led to the opposition losing control over the region. By 2010, the centre of the conflict was confined to the FATA where MSF had no access, apart from a small project in the Kurram district. MSF returned to Swat in May 2010 to re-open the emergency room at Mingora district hospital after the offensive had been proclaimed a success by the Pakistani government and the area proclaimed “cleared” and accorded priority status for “development for stabilisation”.
The government of Pakistan outlined its stabilisation strategy for Swat in the “Malakand comprehensive stabilisation and socio-economic development plan”.Government of NWFP, 2009. Malakand comprehensive stabilisation and socioeconomic development strategy. Swat is one of the districts of the Malakand division.
In the section on “delivery of basic social services”, there is specific reference to the need to restore, expand and upgrade health infrastructure. In addition to this infrastructure funding, the US government provided approximately 36 million dollars of direct aid to the KPK government, with 12 million dollars earmarked for Recovery, Staffing and Supplies for the Department of Health. http://www.usaid.gov/pk/downloads/impl/ILNo.MLK.01MalakandDivision.pdf
Where there are funds, there are NGOs. In the case of Swat, it is estimated that up to eighty national and international NGOs arrived in the Swat valley after the military offensive.
MSF’s decision to return to Swat after the offensive was based not on a desire to rebuild the area in support of a stabilisation agenda, but on medical needs. The Mingora hospital emergency room was barely functioning and, despite claims that the conflict was over, insecurity remained, as witnessed by the sporadic influx of numerous wounded patients. The principal challenge faced by the organisation was how to function in these conditions without compromising its ability to be accepted by local groups opposed to the government and its COIN strategy in and around Swat. This was particularly important as the authorities made clear to MSF that they would not tolerate MSF treating “militants” in its health facility.
As a preventive measure, MSF, bolstered by the trust of the population gained during its previous intervention in the region, decided to make a public statement as part of a broader strategy to engage with the population in Swat. A press release in the local media explained what its intentions were in returning to the area. “MSF is coming back to Swat to address very specific medical needs that we have identified at Mingora hospital. As an emergency medical organisation that is focused solely on providing lifesaving care, MSF is not involved in rebuilding Swat after the offensive, nor are we part of any military or political strategy. For our activities in Pakistan, we do not accept any government funding, choosing only to rely on private funds from individuals”. MSF press release, 25 July 2010.
MSF also decided to no longer refer to itself in its contacts with different parties as an NGO—synonymous with US funding, connections to the UN and faith-based organisations—but rather as a private medical organisation and, later, as a medical humanitarian association. It was also necessary to find the right partners to implement its programmes. This required extensive networking with various groups within the community, in Swat and in the region. Specifically, MSF tried to establish relationships with madrasas (religious schools) and national NGOs, who played an important role in the response to the displacement caused by the conflict and the floods in 2010. The fact that MSF engaged with organisations considered by the west as the competition in the scramble for the population’s “hearts and minds”, was both a vital step in realigning people’s perception of the organisation and ensuring its programmes reached those most in need.
In the other areas of northwest Pakistan where MSF had been unable to negotiate access after 2009, the organisation might have been able to operate, had it agreed to work through national NGOs or with Pakistani nationals exclusively. This is how MSF managed to set up its project in the district of Kurram Agency in the FATA, as it had in Swat in 2008. This would have allowed MSF to access places such as Dera Ismail Khan and parts of the FATA. Yet the decision was taken in 2010 not to replicate this strategy in other parts of the FATA and KPK: in such a highly political and contested context, and without direct dialogue with the opposition, MSF considered it essential to have mixed national and international teams, because international staff can provide a buffer between national staff and community pressures, including pressures from armed groups. This was a lesson learnt from Swat where the MSF national staff running the projects were put under immense pressure to take increased security risks to respond to the needs of their community, resulting in the loss of two MSF ambulance staff in 2009.
The organisation’s international staff would have been allowed access if it had decided to resort to Pakistani army escorts. But, as these would have been provided by one of the parties to the conflict, they would have made MSF a target.
Navigating Dangerous Waters
In a context such as Pakistan, MSF’s ability to increase its safe operating environment, at least in the eyes of the armed opposition, is less about how its principles are understood and more about how its politics are perceived. The affirmation of “neutrality and independence” that MSF lobbies for so vigorously in Pakistan is so against the practices of state-led humanitarianism at the service of counter-insurgency and stabilisation that it becomes a political position in itself that can lead to a degree of acceptance. Because humanitarian organisations in Pakistan embrace western political priorities, the opposition accords a certain value to MSF’s distinct position.
MSF is still only able to operate in those areas to which the government allows it access. Ultimately, MSF’s ability to navigate in the COIN context should be judged in the light of its actual capacity to conduct its activities for those who are denied assistance. MSF’s access to parts of KPK such as Hangu and Timergara, particularly by its international staff, represents a significant achievement. The extent of its operations in these areas is far greater than any other humanitarian organisation has achieved. However, despite these successes, MSF has been unable to gain enough leverage to access FATA, where needs are likely to be most acute, with compromises that the organisation deems acceptable.
***
Somalia. Everything is Open to Negotiation
Michaël Neuman (interview with Benoît Leduc)
This chapter is the result of conversations held from June to December 2010 between Michaël Neuman, director of studies at CRASH—MSF and Benoît Leduc, head of mission and then operations manager for Somalia for the French section of Médecins Sans Frontières from December 2006 to September 2010. As a result, the positions of the Belgian, Spanish, Dutch and Swiss sections also operating in Somalia are not covered in any detail.
Introduction
Médecins Sans Frontières, which had provided assistance to Somali-Ethiopian refugees in Somalia since 1979, quickly came to see the risks and challenges of working in the country. In January 1987, ten members of a team in Tuj Walaje in the north were kidnapped by Somaliland separatists and, in April 1988, the Dutch section of MSF was working in Hargeisa when the town was hit by a heavy bombing raid. The decade that followed began with a conflict that was the outcome of a process initiated years earlier and combined the collapse of the government with an explosion in the number of private armies built around individuals, clans and entrepreneurs.See in particular Roland Marchal, “Mogadiscio dans la guerre civile”, Les Etudes du CERI, no. 69, Oct. 2000.

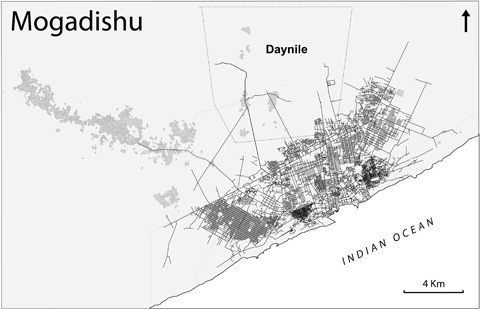
Following the fall of President Siad Barre in 1991, MSF embarked on a series of operations in a Mogadishu torn apart by clan rivalry, in rural areas with displaced people and in Kenya among the Somali refugees who had fled the war. One of MSF’s main concerns was to limit the consequences of the famine which, from spring 1992 onwards, was to trigger one of the first international “military-humanitarian” interventions of the post-Cold War period. Relief operations were carried out in one of the most dangerous environments MSF had ever encountered. The intensity of the fighting as well as the direct threats made against MSF’s employees led to a number of personnel evacuations.
From April 1992 to March 1995, the United Nations ran several consecutive missions intended to ensure compliance with a ceasefire by the main warring factions, as well as the safety of humanitarian aid. Successive reinforcements of the international force, however, were to contribute to its becoming directly involved in the conflict. Civilian and military losses increased, while the international forces themselves perpetrated war crimes. The confusion between humanitarian aid and international military intervention reached a climax. Not wanting to be further associated with violence perpetrated in the name of humanitarianism and facing growing security threats and the Somali population’s hostility towards foreigners, the French section of MSF decided to withdraw from the country in May 1993. This decision was also based on the decline in mortality caused by the famine. Over the years that followed the country remained a focus of confrontation between political-military leaders.We have used this term in preference to “warlord”. Roland Marchal covers the latter in detail, as the term primarily used by institutions and the international media to describe the Somali leaders in charge of the warring militias. For a critical analysis of the term and the consequences of its use on the shortcomings in the analysis of the situation in Somalia, see Roland Marchal, “Warlordism and terrorism: how to obscure an already confusing crisis? The case of Somalia”, International Affairs (83), 2007.
In spite of regular interruptions, MSF continued to work on projects to provide assistance to the Somali population. In 1997 expatriate doctor Ricardo Marques was assassinated in the hospital in Baidoa supported by the French section, which had returned to the country two years earlier. This incident prompted a second withdrawal.
A letup in the fighting in Mogadishu nine years later enabled MSF-France to return to Somalia. During the summer of 2006, the Islamic Courts Union (ICU), established in the mid-1990s in an attempt to restore order in Mogadishu, took control of the capital, which they intended to use as a testing ground for an Islamic Somalia. The population of Mogadishu saw a period of calm it had not known for fifteen years and the international airport, closed since 1995, reopened. A window of opportunity emerged for relief organisations that hoped security conditions were about to improve. The opportunity turned out to be short-lived. In December 2006, the Ethiopian government, fearing the establishment of a radical Islamist regime on its doorstep, launched a large-scale offensive against the ICU and defeated it.
The conflict escalated with renewed vigour, exacerbated by its internationalisation against the backdrop of the “global war on terror”, and opposed transnational Jihadist networks to western powers, the United Nations (UN) and their regional allies. The rebel movement became increasingly radicalised, which resulted in a series of breakaway groups. One of them, Al Shabaab, initially an ICU “youth movement”, became an independent organisation with a small number of highly radicalised individuals. The troops confronted the Transitional Federal Government (TFG), supported by the UN and the AMISOM, an African Union mission created in 2007. Yet the TFG, divided and powerless, was never able to control more than a few districts of Mogadishu.
It is in this context that the French section of MSF did its utmost to find a way to provide assistance in the country. The organisation was forced in a series of never-ending negotiations to compromise in a number of areas: the security of its personnel, the recourse to armed guards, the choice of its action, the standard of its relief operations, its contribution to the war efforts of the warring parties, as well as its ability to speak out.
Discussion
> For many at MSF in Paris, the situation in Somalia could be summed up in a few words: clans, the memory of the death of Ricardo Marques, and complexity. It was the embodiment of operating in unacceptable security conditions and dependence on armed groups. The French section, which had withdrawn from the country in 1997, examined the possibility of a return in 2006. What was the background to the debate?
In the wake of their victory over the Alliance for the Restoration of Peace and Counter-Terrorism (ARPCT)The Alliance for the Restoration of Peace and Counter-Terrorism was a coalition of political-military leaders, supported by the United States. Although it has not been established whether or not it was formed at their instigation, the alliance was supported by the US in order to counter Al Qaeda’s influence in Somalia. It quickly turned into a group with a focus on combating the Islamic courts. According to International Crisis Group, the CIA is believed to have provided the ARPCT with between 100,000 and 150,000 dollars a month. (http://www.guardian.co.uk/world/2006/jun/10/rorycarroll.oliverburkeman)
in June 2006, the ICU took control of Mogadishu. The residents of the city who were, in appearance at least, completely unarmed, returned to a level of security they had not enjoyed for fifteen years. The change in circumstances afforded those who supported a return of MSF’s French section to Somalia the opportunity to float the idea once again. An exploratory mission was carried out in the summer of 2006 in Mogadishu and in the port city of Merka in the south of the country, to establish contacts and assess the reality of the situation on the ground. The return to war following the Ethiopian army’s intervention in Somalia at the end of 2006 encouraged this approach. It was then that I was charged with monitoring the situation and looking at potential projects for the country.
There were numerous discussions at MSF on whether we should start up a new project. The director of operations was opposed to the use of armed guards, and brought up the question of the potential security risks for our teams in re-launching activities in Somalia. In addition, four sections of MSF were already working in the country, and that gave some people sufficient grounds to argue that there was no need for the French section to be there.
> Let’s go back to the issue of armed guards. In Afghanistan, in Eritrea and on many occasions in other situations, the organisation has used combatants to ensure the safety of its teams and convoys. Whilst humanitarian aid should not be imposed by force, the use of armed escorts has sometimes been seen in the history of the organisation as a condition for providing assistance. What were the arguments in the debate that prompted MSF to resort to armed guards in carrying out its operations in Somalia?
During the discussions that preceded the decision to resume operations, the reasons put forward to oppose the use of armed guards were based on MSF’s experience in Somalia and in other countries: the risk of getting involved in funding the conflict, putting the teams in greater danger and becoming dependent on the militias sometimes added to the issue of the neutrality of operations. In the early 1990s, the use of militias was a prerequisite for taking action, from which it then became impossible to extricate ourselves. Although they were supposed to defend the organisation, they would themselves create incidents to generate a further reinforcing of the system. From the mid-1990s onwards, the teams began to reduce the number of guards and to limit our contractual relationships with the militias: MSF, if only to a small degree, was potentially able to play a part in creating the conditions for violence. Using guards meant that we ran the risk of a member of MSF staff killing someone. The numerous security incidents we had faced in the past meant this was a legitimate argument.
But in Somalia, armed guards were above all a necessity, not a choice. On our first visits to the country, we also said we didn’t want armed guards. And then we realised that even the smallest of shops had a guard armed with a Kalashnikov. Since the 1990s, security in Somalia had been completely privatised. It was simply something that was accepted by the MSF teams working at the time and that we came to acknowledge. All Somali hospitals are equipped with a kind of cloakroom where owners check in their weapons in exchange for a number. That’s just the way it is. So, after talking it through, that was the reality MSF decided to accept.
> What were the stages involved in re-launching operations?
One of the members of the exploratory mission in summer 2006 had been the head of mission in 1997, and he met his former deputy at the hotel in Mogadishu. Like many other Somalis, the latter had come to see what was happening in the city with a view to starting up activities again. He was based in Kismayo, in the south of Somalia, and helped us with a visit to Jamaame, a town in the region. A rural area that had for the most part been spared from the fighting, it had a landing strip. This was vital as travelling by car quickly became too dangerous.
Then, of course, there were clearly identified medical needs, as is the case in all Somali rural areas and, above all, the fact that there was no one to provide care. We carried out a few exploratory missions in the surrounding villages. There were heavy floods between November 2006 and January 2007. According to what we were told, children died of diarrhoea because of a shortage of drinking water—the people drank water from the river. Aware of the impact of the floods on the harvest, we feared that the nutritional situation would deteriorate too.
There were many discussions over whether it was appropriate to intervene in Jamaame. Many people felt that the process would slow down our objective of starting up in Mogadishu, which was seen as a priority insofar as the capital was heavily populated and the focus of the conflict. In fact, the project in Jamaame started up very quickly. Some people in the region were already familiar with MSF through our work in Kismayo in the 1990s. The village representatives quickly appointed a single point of contact to manage the vehicles, recruit unskilled staff and rent buildings. We explained and emphasised the principles that underpin MSF operations, namely neutrality in relation to the conflict, our independence from the political authorities and the imperative of being able to provide care for everyone. We had a team in place as of March 2007. In April, we turned our attention back to starting the project in Mogadishu.
I think the work we did in Jamaame was invaluable. It’s important to remember that we had started working in Somalia on the basis of a few previous experiences. It was as if we were paralysed, we understood nothing—or maybe we only understood the risks. In Jamaame we were able to learn again how to operate in Somalia in the right conditions: how to travel around, how to carry out swift nutritional assessments, and how to talk to our contacts to gain an understanding of the health situation.
There was only one clan, which had a reputation for keeping out of the conflict, and the people were asking for help. This enabled us to understand the role of the elders in the village and that of the chiefs who represent each of the clan’s seven sub-clans, and to tackle the question of sorting out cars, houses and armed guards, all issues we would face in Mogadishu. Hiring a car in Somalia results in a series of compromises. You have to forget what you learned as a logistician; that a car should drive straight, brake and have safety belts. There, it’s first and foremost about finding out who owns it, what the power relationships are between clans and individuals and evaluating the risks of reprisals against the teams. We would never have been able to figure all that out in Mogadishu, what with the war, population displacements, the multitude of clans, and so on.
Besides, there was an advantage in having a rural base and a project with seemingly more long-term viability in terms of security. So, until 2008, there were almost no team evacuations. Some of the reasons behind starting up the project in Jamaame were institutional. We didn’t know how long it would take to set up a project in Mogadishu, so it was also a way of getting off the ground and a justification for setting up a team in Nairobi to support Mogadishu.
As far as armed guards were concerned, we discussed different options in order to rid ourselves of some of the constraints they engender. MSF’s guards are not under contract and we do not manage them directly; we give the people’s representatives a sum of money and they decide and run the organisational aspects. But the questions remain. What instructions should we give the guards? How do we manage their relationship with us?
> The team that carried out the first exploratory mission in Mogadishu during the summer of 2006 had proposed working on maternity and obstetric care, but this was rejected. There weren’t sufficient indicators and the risks the teams would be taking seemed too high. The fall of the Islamic courts and the return to fighting in early 2007 prompted a fresh round of discussions. In the end, it was agreed to make surgery the focus of the project. Why not reconcile both priorities? How did the launch of the project in Mogadishu go?
We were faced with the difficulty of obtaining reliable indicators right from our very first visits to Somalia. There is no official data and the numbers can be rigged because they can’t be verified. MSF, with its culture of working with numbers and used to dealing with epidemiological tools, finds it difficult to go ahead with a project based merely on the teams’ gut feelings or intuition. How to grasp the concept of need, when the whole situation feels like an emergency: population displacements, recurring nutritional crises, mediocre immunisation rates, general insecurity, etc.? It was difficult to carry out the actual assessments as the lack of public health facilities was, to some extent, compensated for by pharmacies and private surgeries. We really had no understanding of Somali healthcare practices.
In some ways it was a little simpler in Mogadishu after the Ethiopian intervention; there was a war, and people were wounded. Given the security conditions we were facing at the time, we felt it was important to act where there was risk to life. Surgery was the obvious choice. We carried out an assessment in January 2007 and another in April 2007. At the time, the Somali capital was in turmoil. Ethiopian and government troops were engaged in major offensives against the Islamist combatants in the northern districts of the city. According to the UNHCR, the fighting left over 1,000 civilian casualties and 350,000 people were displaced, primarily in the Afgooye corridor, located some thirty kilo-metres to the west of the capital. The Ethiopians systematically looted and destroyed the medical centres that could have provided assistance to the Islamist rebels.
Evaluation missions were carried out in various facilities in and around the city. We wanted to be based in an existing facility, to make the procedures required for launching the project and the negotiations regarding security easier. We looked at what was available. Of the 800 hospital beds available in January 2007, there were only 250 left by June. The only surgery facilities were those supported by the ICRC. But they were not fully accessible to the opposition forces, partly because of their location.
The hospital in the suburban district of Daynile in the northwest of the city was thought to be a potentially good location. It had received an influx of patients and was struggling, but it was in good condition. Located right in the middle of a displaced persons’ camp, it was some way from the centre. This was crucial, because a facility in the centre of the city would have put us right in the firing line and people would have found it hard to reach.
But warlord and local entrepreneur Mohamed Qanyare, a key figure in Mogadishu, already controlled the hospital. Our relationship with Qanyare was the subject of some profound disagreements with other sections of MSF, which saw it as a risk for the security of our projects. First close to the TFG, he had moved away and then joined again. He had been bankrolled by the United States, notably within the framework of the 2006 Alliance for the Restoration of Peace and Counter-Terrorism (ARPCT).
We explained to Mohamed Qanyare the importance of providing access for everyone. He seemed to accept this and withdrew from the management of the hospital. He said: “I’ll deal with security in the area. As far as the rest goes, talk to so-and-so, and so-and-so, and so-and-so”.
Qanyare is a Murusade chief, a sub-clan of the Hawiye clan. There were Murusades more or less everywhere, both among Al Shabaab and within President Yusuf’s government and the National Security Agency, which is responsible for intelligence and counter-terrorism. These multiple allegiances, of course, result in a highly complex situation, but we can also put them to our advantage to create opportunities for discussions with the various players involved.
We were able fairly quickly to secure guarantees that combatants from all factions would be able to receive care at the hospital. Everyone agreed to play the game, albeit reluctantly. To some extent, Qanyare took a gamble on his reputation in the operation. He had stood in the 2004 presidential elections and was still counting on carving out a political career for himself, and wanted to show that he was open to all the clans. I think he both played this role and acted as a gatekeeper, opening the door to foreigners and thereby making an agreement with the clan possible.
From the rebels’ point of view, it was in their interest to support assistance for their wounded and displaced populations and to encourage the aid organisations to attest to the crimes committed by the Ethiopian army with the support of the government militias. They knew that we were going to work with someone who they had been at war with, while Mohammed Qanyare knew that he was giving us access to a hospital that would be used to provide care for enemy combatants.
> Taking into account the interests of the parties to the conflict raises questions over how operational decisions are made, demonstrating that they are not purely the result of MSF’s assessment of the needs of the population.
The decisions were based on a combination of different criteria. There were discussions on whether we should gear our operations towards paediatrics or surgery. Paediatrics would have met some real needs and would have been easier to put in place as the technical requirements would have been less complex. But we started with sur-gery—for which there was also an overwhelming need—because it was what the key players and leading figures we were able to meet asked us to do. If we had opened a nutrition or paediatric centre, the rebels, the radical Islamist militias, the Murusades and all the other groups would have been less tolerant in their attitude towards the project. It is likely the hospital would have been looted at some point or another.
During our visit in April 2007, at the same time as the discussions on starting up our project in Mogadishu, we were put in contact with a group of doctors who were close to the rebel movement. They were operating in secret and described the violent actions of the Ethiopian army against medical facilities. They stressed the importance of a neutral facility able to treat the wounded, regardless of who they are. We talked to them about our project in Daynile and working with Qanyare. Although they were reluctant, they understood that rebel combatants would have access to the hospital. To support them in their medical intervention, we donated medical equipment, a radiology device and operating tables worth over 120,000 euros. Opposition doctors no longer had the resources to care for the population and wanted treatment facilities to re-open. The donations gave us the opportunity to meet their needs and build relationships with the doctors; it was also a way for us to pay the price of our relationship with Qanyare while negotiating the setting up of a project in Daynile. We had no direct control over what use they would make of the equipment. But we decided to go ahead in spite of the fears of other MSF sections, who maintained that this so-called support for the Islamist opposition could jeopardise all our projects in the country.
We also implemented water supply projects in the displaced persons’ camps established around the hospital after the wave of displacements during spring 2007 and distributed jerry cans of water and blankets. Supporting the local people was a way of protecting the hospital.
> While setting up the project, MSF was keen to formalise the sharing of resources with its various key players. What were the strategies adopted?
Our ability to set up and maintain the project relied primarily on establishing a body to govern the hospital, namely a sort of Board of Directors independent of MSF. We continue to provide “indirect” management, avoiding as far as possible any involvement in personal, political and local clan disputes. We do not select the dozen or so members of the Board, who are co-opted. Usually leading figures in the district, they are frequently relatives and friends of Qanyare and the Murusades.
If there’s a problem, we say to them: “You’re the Board, it’s your hospital, you manage it and we’ll support it”. When we wanted to pull out of supplying water by lorry to drill instead, we discussed it with the Board. It was the Board that negotiated access to the land and then sorted out terminating the lorry rentals. We find these negotiations unfathomable, and do not get involved. All we do is convey messages: “If MSF is threatened, we might have to cut short the projects”.
As far as recruitment is concerned, we decided to take a gamble: if we focused on skills, we would find the diversity of clans vital to reach our patients. We recruit using written tests and questionnaires supervised by international staff. We have promoted the transparency of the system in conjunction with the Board. If everyone is entitled to take part and staff are recruited for their skills rather than their clan, people are ready to go along with it. In April 2008, we organised a test to recruit twenty nurses which was taken by 535 people.
As in Jamaame, security is arranged at arm’s length. The budget allocated to armed guards is included in a package we give to the hospital designed to fund its running costs, including non-surgical medical activities in which we have no direct involvement.
> Since the project began, over 12,000 patients have been treated in the hospital, with over 50% of injuries caused by the war. That said, the situation has changed hugely. The region is now controlled by Al Shabaab and Qanyare’s influence has decreased. Given this context, can civilian populations and combatants from different factions still access the hospital?
During the first months of the project, patients came primarily from areas in the immediate vicinity of the hospital. There was a significant proportion of women and children among the injured who had been victims of the bombing raids: over 56% between October and December 2007, and over 53% in 2008. Gradually, patients started to come from a wider area and we were reassured that the whole of the population, whatever their clan, had access to the hospital. We are now effectively in a neighbourhood controlled by the Islamist opposition, with the war-wounded coming from this area. This is less the case for patients not wounded in the war and who come from a much more diverse range of geographical areas.
It’s highly likely that some armed factions refuse to go to the hospital, but that is certainly not the case for women and children. It’s difficult to be sure. They have fallen as a proportion of all those treated for war-related injuries since 2008, but the figures vary as the conflict evolves along with the nature and location of the fighting. As soon as there are bombing raids in residential areas, the proportion increases again. Conversely, during periods of intense and direct clashes such as we have seen since the beginning of the year, more of our admissions are combatants. But we must continue to closely monitor this issue of access without distinction to the hospital.
In these conditions, we are sometimes seen by some political players, the African Union mission officers, for example, as the opposition’s war surgeons. This is when we need to remind people of the fundamentals of providing access to medical facilities in times of war, namely that injured and unarmed combatants are classed as non-combatants. What’s more, they only represent a proportion of our patients. We can also remind people of our support for the medical department of the hospital, where 70% of in-patients are women and children.
In Jamaame too we have had to deal with a change in authority and the fact that Al Shabaab has taken power. At the beginning of our intervention, the elders were in power and in charge of the judicial system, the police, the prison and the market—even if a representative of the TFG was present. When Al Shabaab regained control of the town in May 2008, the elders were removed from power and in some cases accused of corruption. They have now been partially reintegrated into the community, because Al Shabaab has probably understood the advantages of having their support in administering the region.
> In January 2008, an attack on a team from the Dutch section of MSF in Kismayo caused the death of three employees, a Somali, a Kenyan and a Frenchman. These murders and an ongoing deterioration in the country’s security situation instigated a major review of MSF’s operating methods. All projects switched to what is known as “remote management”, which means that day-to-day project management is carried out by national staff working remotely with international staff. It is, to some extent, comparable to the armed guards’ issue; it shatters the idealised vision of the giving of aid. Is humanitarian aid not fundamentally about our relationship with other people: the doctor from here who goes to care for people there? The arguments opposed to this method of management raise questions about the neutrality and independence of national staff, as well as the issue of control of resources. How do we resolve these dilemmas?
The attack in Kismayo in January 2008 led to the withdrawal of international staff from all MSF projects but, after a few weeks of internal discussions, we sent teams back to Jamaame and Daynile. The assassination of Al Shabaab leader Aden Hashi AyroOne of the leaders of Al Shabaab, Ayro was considered to be a representative of Al Qaeda in Somalia. by the United States in May 2008 created a power vacuum that a number of Jihadist factions were able to take advantage of and which drove some of them to become more radical, more quickly. This fragmentation of the Islamist rebellion had a very high cost in terms of humanitarian workers’ security. At the same time, we saw an escalation in the rejection of humanitarian aid—seen purely and simply as providing support to the Islamists—by many supporters of the TFG. Until Sheikh Sharif Sheikh Ahmed was elected head of the government in January 2009, attacks on humanitarian workers by TFG fighters were no less dangerous than those carried out by Al Shabaab.In 2008, forty-five humanitarian workers were killed in Somalia, compared with thirty-three in Afghanistan, nineteen in Sudan and thirteen were kidnapped, Stoddard A, Harmer A, DiDomenico V. “Providing aid in insecure environments: trends in violence against aid workers and the operational response” (2009 update), Apr. 2009, London: Overseas Development Institute”, 2008 was deadliest year for aid workers—study”, Reuters, 6 Apr. 2009.
In the period that preceded Ayro’s death, we had been able to maintain contact with the opposition via the Murusade and medical networks, and established a constructive working relationship with Al Shabaab. The organisation even wrote to us in January 2008 to offer us their encouragement. But as soon as non-Murusade Islamist rebels arrived in Daynile, it became more difficult for us to negotiate visits, particularly as the journey between the airport and the hospital became even more dangerous, due to the fighting and the risk of kidnap.
We were forced to restrict ourselves to organising occasional visits to Jamaame, where we had an expatriate team. In Daynile, we had started the project without any international staff present on an ongoing basis, not only because of the risks of foreigners being targeted but also the potential for collateral damage—getting caught in crossfire, attacks, etc. Our decision not to get involved in non-surgical medical activities was also due to insufficient expatriate staff. We moved from this kind of intermittent mode to making infrequent and last-minute lightning visits. The expatriate team is still based in Nairobi, so project management now relies much more heavily on Somali personnel than it did in the past. Of course some people have been able to adjust to a situation where they are paid a salary and have access to resources and drugs with less supervision. Organising visits to Daynile is an additional source of stress for staff because they have to organise and pay close attention to our security.
The future of the programme will depend on the relation between the security issue and the obligation to monitor; from their side, a member of the Board in Daynile explains that, “We know that if something goes wrong, it’ll be the end of the hospital”; and from our point of view, as our head of mission explained, “If nothing happens, meaning that if we don’t go there, that’ll be the end of the hospital too”. And that’s where we are today.
Our biggest constraint is our limited ability to expand our activities and our capacity to respond to emergencies. In August 2010, the number of displaced people living in the camps in the Daynile area was probably around 110,000. There was a very high level of need and the aid provided was inadequate. A few organisations, such as the Red Crescent, do a small amount of work in the camps. In normal times, we would probably decide on a major intervention, supplying water, purification and distribution systems, providing medical care, etc. But the camps are Al Shabaab’s constituency and are under its tight control. Our staff are not always comfortable with the idea of working in them. Generally speaking, the threats faced by the local employees are immense and the risk to their safety huge and incessant.
As for checking that the resources provided by MSF are properly used, we look at as much medical, logistical and financial information as we can and, up to a certain point, all the elements of a normal project are there. We have to examine supervision, the quality of medical care and monitoring. We analyse the quantities of drugs used, activity reports and the number of registered patients. We then examine the consumption of certain sensitive and expensive drugs, as well as the reasons for and data on admissions and discharge in nutritional activities. There’s some information we’re not able to get hold of, such as the number of children in the nutrition programme, for example, and we do have some fictitious patients. But we encounter the same challenges in projects where expatriates are involved. Our visits to Daynile—and we haven’t been back since April 2009—are, in fact, relatively ineffective. We spend our time dealing with the unplanned events that crop up on a day-to-day basis while the medical side, such as carrying out an inventory of the pharmacy, monitoring a patient, checking the quality of care and prescriptions, is reduced to a bare minimum.
This is an ongoing situation and the quality of care provided by MSF gives cause for concern. Our standards of care in Daynile are not those of our programmes in Haiti, for example. It is even hard sometimes to check our doctors’ qualifications. Because of this and despite our discussions with the staff and the training we have put in place, fracture repairs and infection control are not carried out in conditions as satisfactory as we would like.
As long as the security situation continues to remain this problematic, we are unlikely to see a return to a regular expatriate presence in the near future. What’s more, new constraints may well be on the horizon, notably Al Shabaab’s demands regarding the nationalities of the expatriates it will authorise to visit the projects.
> In January 2008, Al Shabaab proclaimed its unequivocal allegiance to the leaders of Al Qaeda. At the same time, the international intervention was operating in a context increasingly influenced by the “war on terror”. What has been the impact of this polarisation on our activities?
We are seeing a new period where the parties to the conflict are attempting to co-opt aid, in a country that has seen many such attempts. In January 2010, the WFP, against a background of accusations of misappropriation and corruption, announced it was suspending its aid programme in the centre and south of the country because of the growing number of attacks on its staff. Then, in February, Al Shabaab itself prohibited food aid from the WFP on the pretext that its operations were “politically motivated” and that they were undermining the local market. In November 2009, it issued a list of eleven conditions for the continuation of international aid, including payment of a 20,000 dollar tax every six months and the dismissal of all female staff, except for those working in treatment facilities. In August 2010, Al Shabaab announced it had banned NGOs such as World Vision, ADRA and Diakonia, accusing them of proselytising. The group is now demanding that Somali employees working on MSF projects in the area under its control pay a tax equivalent to 5% of their salary, in addition to “registration costs” of 10,000 dollars per project. It also tries to impose taxes for using the airports. Daynile is not affected, or at least the Board has been able to block the demands, which proves how important the project is to Al Shabaab.
Each Al Shabaab demand leads to more discussions on the restrictions we are prepared to accept or that it is reasonable to accept in such a complex situation: a combination of the considerable medical needs, questions regarding our ability to manage such complicated programmes and the impasse in which international intervention and the country, now embarking on yet another peace plan, find themselves.
But, international sanctions and anti-terrorist legislation do tend to limit the ability of aid organisations to work in rebel-controlled areas. It is civilians’ access to aid that is undermined. As the United Nations sends out on a daily basis ever more alarming messages on the “humanitarian situation”, in 2009 American donors suspended some of their funding, fearing that they could be prosecuted for providing assistance to Al Shabaab, classified since March 2008 as a terrorist organisation by the US State Department. In March 2010, the United Nations itself adopted a resolutionResolution 1916 (2010), adopted on 19 Mar. 2010. that potentially sets up the conditions for imposing sanctions on aid organisations working in areas controlled by opposition groups. In an article published in June 2009, the United Nations’ special representative in Somalia, Ahmedou Ould-Abdallah, wrote that “those who claim neutrality may also be the accomplices” of the opposition. Even if it has no immediate consequences, this process makes the need to differentiate international initiatives in the eyes of both the people and the parties to the conflict all the more vital.
However, insofar as Al Shabaab controls the majority of the country and Mogadishu in particular, all we can do is accept reality. It is crucial that we ensure that patients are not selected on the basis of their allegiance to or membership of certain groups, and that we don’t choose whom we talk to—including those claiming to be from Al Qaeda.
> Violence against civilians is frequent, attacks on hospitals are not irregular and our activities are restricted by security issues. In the public arena, however, we hear much more from the United Nations than from MSF, which doesn’t appear to be saying much at all. What do we want to say? What are we not allowing ourselves to say?
Initially, our communications policy was coherent with that of our operations. Keeping a low profile was the order of the day. We didn’t want to say anything at all. We were afraid of everyone. Responsibility for the attack in Kismayo against MSF-Holland has never been clearly established. We were afraid of Al Shabaab, the Ethiopians, the clans, the warlords, the government and the lack of government.
In the beginning, everyone in Daynile—the local people, the staff, the rebels and then Al Shabaab—told us, “Don’t talk politics, don’t get involved in politics”. This was the message we were given very clearly on several occasions. Maybe the strategy has paid off, given that Al Shabaab in Jamaame has expelled all other NGOs, but not MSF.
The risk we run when we speak out in such a complex situation is huge. As a result, our current public communications are purely factual and very closely linked to our activities, such as our treatment of malnourished children and the wounded in Daynile. Fear of Al Shabaab is even greater and MSF’s communications must be pragmatic, as it is now more important to distance ourselves from international efforts focused on defeating Al Shabaab and offering absolute support to a transitional government running out of steam. While we were able to publish a press release appealing to the African Union not to bomb residential neighbourhoods, we have never asked Al Shabaab not to use civilians as a human shield when its members take cover in the market in Bakaraha.
Given the immensity of the medical needs and the complexity and difficulty of meeting them, we are afraid of losing what we have managed to put in place. It seems to us essential that we set ourselves apart from other international players, by not calling for the reinforcement of AMISOM, for example. But speaking out about who is responsible for the conflict is certainly more difficult to define and accept.
Translated from French by Karen Stokes
***
Gaza. Strip a Perilous Transition
Caroline Abu-Sada

MSF began working in the Palestinian territories in 1988, a few months after the outbreak of the first Intifada. Since then, various MSF sections have attempted to attenuate the effects of Israel’s occupation on Palestinians’ access to certain types of healthcare. But the existence of an efficient health system has made it difficult for the organisation to find its place. For example, in Gaza in 2007, there were almost 3,800 doctors, more than 4,200 nurses and around twenty hospitals for a population of just over 1.5 million. It counted 13.6 hospitals beds per 10,000 inhabitants, against seventeen in Jordan. Furthermore, the main causes of mortality in Gaza are cardiac and cerebrovascular diseases,2007 data, WHO office, Gaza. the same as in high or intermediate income regions. MSF’s projects are operating in the midst of a conflict that has been internationalised from the outset, attracting a huge amount of media attention and generating intense transnational political mobilisation. The imperative for MSF to be present in such a symbolic conflict is complicated by the difficulties in finding relevant medical programmes.
This chapter focuses on MSF’s actions in the Gaza Strip between 2007 and 2010. During this period the organisation was seriously rethinking its political and operational positioning—a rethink that would call for concessions by both MSF and the government of Gaza.
The French section of MSF has been working in Gaza since 2000. Until 2005, its project was centred on psychological care, accompanied by medical-social care for people living in areas particularly hard-hit by the conflict (families whose houses had been requisitioned by the army, or were living near the settlements or in parts of the Gaza Strip where military authorisation was needed to enter or leave, etc.). After Israel’s disengagement from the Gaza Strip in August 2005, MSF focused its attention on the border areas, considered to be the worst affected by the violence. Its programmes included the procurement of medicines and medical supplies for health facilities in preparation for a possible inflow of casualties. At the start of its interventions in Gaza, MSF was in contact with its usual political interlocutors: Israel, with which it negotiated visas, access to Gaza and administrative issues, and the Palestinian Authority, a nascent state body established by the 1993 Oslo Accords, based in Ramallah, in the West Bank, with which it coordinated care activities.
In January 2006, Hamas (the “Islamic Resistance Movement”) won a decisive victory in the Palestinian elections. There followed a year of political tension between Fatah, the main party of the Palestinian Authority, and Hamas. In the spring of 2007, armed fighting broke out in the Gaza Strip, and in June, after a battle left more than a hundred people dead, Hamas took power. But the Palestinian Authority still had control of the West Bank, so there was now a government led by a democratically-elected party, Hamas, in the Gaza Strip, and a nonelected government led by the Fatah Party in the West Bank. The government in Gaza was immediately boycotted by part of the international community, including the United States and the European Union. Israel set up a land, air and sea blockade from which humanitarian aid was supposedly exempt. The main institutional donors made funding for non-governmental organisations dependent on an undertaking not to enter into contact with Hamas, forcing some NGOs to limit or even suspend their activities. MSF, whose projects were financed from private funds, was not affected by these constraints which, in the name of the fight against terrorism, discriminated against Palestinians unlucky enough to be living in the wrong place. In September 2007, Israel declared Gaza a “hostile entity”. From that point on, Hamas was determined to demonstrate its ability to manage Gaza or, in other words, to transform itself into a ruling party. All of Hamas’ strategies with the actors present, and notably MSF, were established with this one aim in mind.
In 2007, healthcare in Gaza underwent some important changes. The high number of casualties in the fighting between Palestinian factions tested the limits of its care system. In June 2007, the “Battle of Gaza” alone left more than 500 people wounded. The Palestinian hospitals coped remarkably well with the surgical requirements, but could provide little post-operative care. The climate of insecurity and the tension between the two factions also limited access to public care facilities for any patients considered to be opponents of Hamas. Furthermore, the healthcare system suffered from the rivalry between the two health ministries in Gaza and Ramallah. Fatah which ran the Palestinian Authority, ordered its health workers posted in Gaza to strike if they wanted to continue to be paid, while Hamas duplicated the administrative facilities and appointed its own health officials. The embargo—in spite of Israel’s claims that medical aid would be exempt—combined with the unwillingness of the Health Ministry in Ramallah to cooperate with Gaza, made it increasingly difficult to procure medicines and medical supplies for the hospitals.
The change in context provided MSF with an opportunity to step up the medical dimension of its programmes, in addition to the psychological care it was already providing. It opened a centre offering postoperative care and physiotherapy for casualties admitted to the Palestinian hospitals in Gaza City, and set up mobile physiotherapy teams throughout the Gaza Strip. These mobile teams provided a care solution for patients whose physical incapacity kept them housebound, and for anyone whose links with Fatah prevented them from seeking treatment in Hamas-controlled health facilities. A paediatric clinic was also opened in Beit Lahiya to make up for gaps caused by the blockade and the health worker strikes. All these new activities were run out of private MSF facilities to ensure access for all patients—and because the public hospitals were already full to overflowing.
Hamas: From Indifference to a Power Struggle and Imposed Negotiations
In a context marked by the Israeli blockade, international sanctions against Hamas and animosity between Palestinian factions, the new political situation in Gaza created problems for MSF, used to dealing only with the Palestinian Authority and the Israelis. Since arriving in the Gaza Strip in 2000, MSF had occasionally met with the leaders of Hamas, but that was before the race for the elections when it was just another opposition party. In the months following Hamas’ accession to power, MSF continued to negotiate the legal conditions governing its presence in Gaza with the Palestinian Authority. The formal agreements on the provision of post-operative outpatient care and the opening of the paediatric care unit were signed in Ramallah in August 2007 and May 2008. As for the Hamas government, it initially devoted very little time to establishing formal relations with international NGOs. Its representatives, whose responsibilities were still somewhat vague as the structure of the new government was still being decided, seemed happy enough with the informal discussions they held with MSF during which they were told about the organisation’s objectives and activities.
But by continuing to negotiate the legal framework of its interventions with the Palestinian Authority in Ramallah, MSF ran the risk of being seen to support Fatah in its fight against Hamas for sovereignty. Yet in September 2008, MSF called public attention to the responsibility of the political authorities, including Fatah, in the deterioration of the health situation. A press release entitled: “Gaza: politics take precedence over health”, stated that: “The Palestinian Health Workers Union [pro-Fatah] is encouraging striking members to volunteer their services free of charge to patients being cared for in facilities managed by NGOs. But MSF has neither the capacity nor the legitimacy to deal with the repercussions of this crisis. Nor is it our mandate to ensure a “minimum level of service”, as certain parties to this conflict have asked us to do. MSF refuses to play this role. We cannot and must not attempt to replace an entire public health system. […] Rather than considering healthcare as an essential service, humanitarian and vital, it is being used to apply political pressure by two parties equally heedless of the consequences this could have for the population”.“Gaza: la politique prime sur la santé?”, MSF, Sept. 2008, http://www.msf.fr.
But this was the only time since Hamas had come to power in Gaza that MSF had publicly pointed the finger at the Palestinian Authority. Substituting for inadequate health systems might well be nothing new for MSF, but here it was crucial not to appear to be taking sides in the intra-Palestinian struggle, and to highlight the uncomfortable position in which all the parties to the conflict were placing it.
At the beginning of October 2008, Bernard Kouchner, France’s foreign affairs minister at the time, announced after an official visit to Gaza that the French government was being provided with information by French NGOs working there. MSF immediately issued a press release, as did Médecins du Monde (MDM), refuting these unfounded and dangerous allegations which cast doubt on its intentions and jeopardised its activities. These statements by the very minister who had co-founded MSF in 1971 and MDM in 1980 only served to heighten Hamas’ mistrust of foreign aid organisations.
On 27 December the Israeli army launched “Operation Cast Lead” in the Gaza Strip. The first three days of the offensive were particularly violent. As Gaza City’s main hospital, Al Shifa, was struggling to cope with the massive inflow of casualties, MSF decided to increase surgical capacity by setting up a hospital in inflatable tents. The initial plan was to put these tents up in the hospital grounds, but MSF eventually set them up at the end of the offensive outside the hospital to ensure its services would be accessible to all the victims. This project was discussed with administrative staff at the Gaza Health Ministry, but the health minister himself was not informed. In January 2009, MSF signed an agreement with the Health Ministry in Ramallah to extend its post-operative activities in the Gaza Strip.
The military offensive in December 2008 and January 2009, which left 1,300 Palestinians dead, more than 5,000 injured“The Gaza Strip: Operation Cast Lead, Dec. 27, ‘08 to Jan. 18, ‘09”, Btselem http://www.btselem.org. and caused large-scale material damage, marked a political turning point in Gaza. In the eyes of the population, Hamas emerged victorious. The Palestinian Authority, on the other hand, was seriously weakened, in particular due to statements made by its president, Mahmoud Abbas, on the first day of the conflict, in which he blamed Hamas for Israel’s attack on Gaza. At the end of the offensive, as a number of its leaders had been killed in the fighting, Hamas reorganised its administration. These changes led to the start of a new phase in relations between MSF and the Gaza government, which soon turned into a power struggle.
Following a visit to the tent hospital in mid-July 2009 by inspectors from the Gaza Health Ministry, the minister decided to close the facility down with immediate effect on the grounds that MSF did not have the necessary authorisations and that carrying out surgery in tents was not appropriate in Gaza. Between October 2009 and April 2010, a series of meetings took place during which Hamas voiced a number of criticisms and demands. The criticisms focused on MSF’s recruitment policy and the fact that it was not sufficiently integrated into public facilities, while the demands were related to access to patients’ personal files and home visits by medical teams. As far as Hamas was concerned, MSF had to become an integral part of its planned re-organisation of public health facilities in order to “avoid duplication and wasting money”.Expression used in a letter sent to MSF by the ministry in Mar. 2010.
It believed that incorporating the organisation into its public facilities would also allow the transfer of competencies to ministry staff. It also felt that, as no agreement had been signed with the ministry on surgical activities (intensive care unit and operating theatre), it could not guarantee the quality of care for which it deemed itself responsible. With regard to recruitment, MSF was accused of employing the ministry’s surgeons without its knowledge and paying them much more than they received from the ministry as public sector employees. Two surgeons had indeed been hired by MSF in 2008. They were paid on a piecework basis and the increase in the number of interventions carried out after Operation Cast Lead meant they were earning up to 8,000 dollars a month. Lastly, the ministry demanded that MSF, like the other medical organisations working in Gaza, should stop making home visits and hand over the patients’ full medical files so it could carry out the necessary follow-up in the event of complaints about medical treatment.
These criticisms of a legal and administrative nature were compounded by other factors. During the discussions between MSF and Hamas, frequent references were made to the behaviour of the teams, both national and international, and to “parties” held at MSF’s offices where Palestinians mixed with expatriates and alcohol was consumed. This was “not how [Hamas] wished society to be organised”.Minutes of a meeting between Hamas and MSF, Nov. 2009.
Marked by Bernard Kouchner’s statement and its rejection by the western world, Hamas also continued to express doubts about MSF’s neutrality. It took issue with the weekly security meetings—intended to update the teams on travel conditions—which it saw as information-gathering sessions. In September 2009, two MSF employees were summoned by the internal security services and subjected to tough interrogation about MSF’s work. However, their main criticism seemed to be directed at conduct outside of work, which they considered to be incompatible with the new social order that Hamas was endeavouring to establish.
These areas of dissension were a reflection of Hamas’ determination to be recognised as the legitimate health authority in the Gaza Strip. Meanwhile, the Ministry of Health in Ramallah was still asking MSF to sign framework agreements and provide it with “information on its activities”. Interview with the director of international cooperation at the Palestinian Authority’s Ministry of Health, 12 Jan. 2011
At the end of 2009, the authors of MSF’s strategic plan recognised the need to react to the new political and administrative reality in Gaza. “We will continue ongoing discussions with the authorities in the Gaza Strip to try to negotiate the freedom to get on with our work (Hamas is clearly determined to maintain strict control within the Strip). Our presence in Gaza will therefore depend on the compromises Hamas asks us to make”.Strategic plan, MSF-France, 2010.
But many of Hamas’ demands were rapidly deemed legitimate as they emanated from a sovereign authority. The organisation undertook not to recruit any more health workers from the public sector and to provide Hamas with more information on the project. It also undertook to draw up a global agreement defining the framework of its intervention and to develop the plastic surgery project it wanted to set up in Nasser hospital in collaboration with the Gaza Ministry of Health. However, MSF refused to hand over the full patient files, citing its duty to respect medical confidentiality. The ministry finally agreed that this information should only be shared between doctors from MSF and the Ministry of Health. It also gave way on the issue of incorporating MSF’s psychological and post-operative care facilities into the public system. MSF had argued that there was a danger of the confidentiality of information concerning patients receiving psychological care being jeopardised and that the choice of patients requiring physiotherapy should remain MSF’s responsibility. However, the organisation promised that ministry staff would be offered physiotherapy training and agreed to stop home visits for functional rehabilitation and mental health patients at the end of February 2010.
These events highlight the difficulties encountered by MSF in adapting to the political changes in Gaza and to the demands being made by the new authorities with regard to health policy. Clinging to the belief that power over Gaza was still being exercised from Ramallah, the teams reacted relatively slowly in dealing with the new political authorities; this is viewed as one of the weaknesses in the action carried out by the organisation since 2006. There is no written evidence of an explicit choice being made by MSF, but based on a series of personal accounts by international staff, managers at headquarters and Palestinian employees,Interviews carried out in Dec. 2010, Jan. and Feb. 2011. there appear to be two reasons for this attitude. Firstly, the national team, recruited when Fatah was in power in Gaza and composed essentially of people close to Fatah and to left-wing Palestinian nationalist parties, probably influenced the way the international teams perceived events in the Gaza Strip. Secondly, it is likely that this influence was even more potent because most of the involved expatriates and project managers, including those at headquarters, had already accepted the prevailing representations of Palestinian political actors and accorded more legitimacy to the Palestinian movement that had signed the Oslo Accords, embodied by the Palestinian Authority and its main component, Fatah, than to Hamas. This ideological proximity, although doubtlessly implicit, combined with the perspective from which MSF was viewing the situation, goes some way to explaining why MSF found it so hard to alter its reading of what was happening in Gaza.
MSF saw the Hamas government as wishing to impose both health policy choices and its own vision of society and did not want to be dictated to on how it should behave and how it should run its activities. This stance was due partly to a political desire to limit its collaboration with Hamas and partly to its difficulty in understanding the deep mutations underway in Gaza. The organisation gave the ruling authorities the impression that it had put itself beyond their reach at a time when there was a real need to organise services for the population and consolidate their legitimacy.
Hamas finally left MSF no choice but to negotiate the scope of the organisation’s operations in the Gaza Strip. These negotiations focused on both medical and administrative issues. However, after the political and military defeat of Fatah, its long-standing interlocutor in the Gaza Strip, MSF’s relations with Israel were to be determined by matters of a completely different nature.
Israel and the Humanitarian Management of the Gaza Strip
Israel had evacuated its settlers and the military from the Gaza Strip in August 2005 as part of a non-negotiated withdrawal. However, it continued to control all entries and exits. For MSF, maintaining its activities therefore depended to a large extent on its relations with the Israeli authorities. This was all the more true after the Gaza blockade had been set up which, in theory, allowed through certain essential goods and humanitarian aid. In reality, however, orders of medical supplies and medicines sometimes remained stranded for days or even weeks if all the necessary permits hadn’t been obtained, or if the contents of the crates contravened some aspect of the relatively vague rules governing the embargo—or even for no apparent reason.
The Israeli “Cast Lead” offensive was a perfect illustration of the role Israel intended humanitarian aid to play in Gaza. It also goes some way to explaining the relations between MSF and Israel, which was anxious to demonstrate its concern for humanitarian issues. Thus, in response to a French proposal for a “48-hour ceasefire on humanitarian grounds” on 1 January 2009, and in spite of the fact that 400 people on the Palestinian side had already been killed, the Israeli foreign minister, Tzipi Livni, explained that “aid convoys [were] being allowed through the border crossings” and that consequently there was “no humanitarian crisis in Gaza and […] no need for a truce”. When, on 31 May 2010, the Israeli army attacked a flotilla of six ships transporting humanitarian aid to Gaza, Israel’s deputy ambassador to the United Nations, whose task it was to defend the blockade, took the same position, thereby minimising the consequences of the “strategy designed to throttle Gaza” that had been adopted by successive Israeli governments.Rony Brauman, “La flottille de la liberté: humanitaire ou politique?”, 4 June 2010 http://www.msf-crash.org.
Interviewed in early 2011 about intervention opportunities for MSF during Operation Cast Lead, the head of NGO relations at the Israeli Defence Ministry and Coordinator of Governmental Activities in the Territories (COGAT) retrospectively justified the authorisations given to MSF in the following terms: “During operation ‘Cast Lead’ we authorised entry to any humanitarian operator providing real humanitarian assistance. We allowed MSF entry because we knew it would be useful. MSF asked us if it could take in tent hospitals, medicines and humanitarian workers. And nothing is more humanitarian than medical assistance. If your movements are coordinated with the Israeli Liaison Office (DCL) and you are providing medical assistance, why would we refuse authorisation? Some NGOs wanted to go in just to see what was happening, not to help, and that’s why they were refused access”.Interview carried out in Tel-Aviv, 16 Jan. 2011.
For MSF, along with other humanitarian organisations, difficulties in getting aid into Gaza increased once the embargo was in place. For the organisation, 2007 started badly even before the “Battle of Gaza”, with an incident that had serious consequences for its action. On 17 April, during a trip to Jerusalem to attend a meeting with the coordination team, a Palestinian employee from Gaza was arrested for taking part in a “conspiracy” against Israel. In addition to the dramatic personal consequences of the incident, this arrest and subsequent conviction had numerous repercussions for MSF. Rumours circulated in Gaza that MSF had betrayed its employee and handed him over to the Israelis. In Israel, the organisation was the victim of a short but virulent press campaign during which it was accused of promoting terrorism. See “Doctors without borders gave terrorist entry pass to Israel”, 17 May 2007, www.israelnationalnews.com.
For the authorities in Tel-Aviv, this episode was a real opportunity: not only was MSF’s credibility undermined, but the risk of attack could be used as justification for restricting movements between the West Bank, Jerusalem and the Gaza Strip. Yet the organisation managed to keep up its activities, to the extent that some organisations who experienced more difficulty than MSF in obtaining travel permits at the Erez terminalThe only crossing point for pedestrians separating Israel and the Gaza Strip. border crossing believed it was getting special treatment. The Association of International Development Agencies (AIDA) published a communiqué in December 2008 in which it referred to differences in treatment between organisations: “Consequently, the use of a “security” justification to restrict entry by NGO staff to Erez for over twenty consecutive days beginning the first week of November is not consistent with prior security responses. Furthermore, the granting of permission for entry to MSF, UN, and ICRC staff is also not consistent with the justification of “security””.AIDA, “Unprecedented denial of humanitarian access to Gaza must not continue say International Agencies”, http://www.kvinnatillkvinna.se.
However, although MSF had very little scope for negotiation with Israel, it appeared to content itself with this. For example, it didn’t ask for more access to Jerusalem for staff in Gaza, and vice versa, in a conflict where access and the free movement of goods and people were major issues.
In such conditions, is it possible for medical aid organisations such as MSF to avoid becoming the healthcare assistants of the occupying power? The issue of NGOs assisting the occupation was explicitly raised by the president of MSF in 2002: “Until now, international humanitarian aid has only played a peripheral role in this conflict, but there is a danger of it being expected to assume that of assistant prison guard at the centre of a pitiless system of domination and segregation. After the capacity for resistance of the Palestinian population, it is now the independence of foreign relief workers that is being put to the test”.“Palestinian Chronicles: Trapped by War”, report, supplement to Messages, MSF newsletter, July 2002, p. 63.
Left-wing Israeli intellectuals also questioned the role of humanitarian aid at a time when four-fifths of Gaza’s population were reliant upon it.OCHA. Special focus—Occupied Palestinian Territories, Dec. 2007.
In their opinion, it was serving to “suspend the catastrophe” and freed Israel from the obligation of finding a way out of the conflict. For Adi Ophir and Arielle Azoulay, “the normal operation [of humanitarian and human rights organisations] is an extension of the ruling
apparatus, one of its branches, the one responsible for the suspension of the catastrophe and the creation of chronic disaster”.Arielle Azoulay, Adi Ophir, “The ruling apparatus of control in the Occupied Territories”, symposium proceedings, Jerusalem: Van Leer Institute, Apr. 2004.
Dov Weissglas, adviser to Prime Minister Ehud Olmert, in an attempt in early 2006 to justify the blockade after Hamas’ victory in the legislative elections, commented: “It’s like an appointment with the dietician. The Palestinians will get a lot thinner, but they won’t die”. “As the Hamas team laughs”, Haaretz, 19 Feb. 2006.
Some Palestinians also criticised the presence of NGOs in the occupied territories, believing that assistance programmes helped “normalise” the situation and relieved Israel of its responsibilities as the occupying power.
It should be noted that this notion that humanitarian aid can potentially collude with an oppressive system is not, however, confined to the Palestinian Territories. Furthermore, MSF has only a minor role in the aid operations conducted in the Territories in general, and in Gaza in particular.
There are settings in which it is hard to avoid polarisation, and the Palestinian Territories is one of them. MSF has only ever worked with the Palestinian population and never in Israel, something that it is reproached for on occasion in the Israeli press. Consequently, the issue of its “neutrality” in the Israeli-Palestinian conflict has often been raised. It has also been raised with regard to its relations with the two Palestinian political factions, especially as, after the violent transfer of power between Fatah and Hamas in Gaza, its teams were confronted with what was for them a whole new scenario.
The imbalance in the forces involved, the media attention attracted by the conflict which offered countless opportunities for public statements, the proximity of the international teams to the Palestinian staff, as well as their daily exposure to the conflict, made political neutrality difficult and fostered the international teams’ empathy with the Palestinians, whom they perceived as victims. In 2001, the subject was discussed in a board meeting: “Many of them [members of the field team] are asking why their testimony gathering is not being reported by MSF; why we are not publically denouncing Israel’s policies and practices in the Palestinian Territories”. It was in response to these demands that MSF began publishing its “Palestinian chronicles”“Palestinian Chronicles”, Messages. in 2002. Presented as “an account of the day-to-day reality of a population trapped by war and whose suffering is largely ignored”, these chronicles contained the highlights of MSF’s testimony activity in the Territories and helped soothe tensions between the field teams and headquarters.
Recordings of discussions at board level reveal that several members of the team were considered to be “overly-invested in ‘testimony’ gathering”.Minutes of the Board of Directors meeting, 27 Apr. 2001.
Bearing witness to the living conditions of the Palestinians and to the violence they were suffering had become an end in itself for some of the team who expected to see MSF make its position public. Yet the organisation acknowledged that the requirement for “neutrality” was pushed to the limit when, as remarked by its president: “The military occupation is accompanied by such violence against the inhabitants of the Territories, the balance of power is so unequal, that there is a certain indulgence of the weakest, even when they commit crimes”.Minutes of the Board of Directors meeting, 26 Apr. 2002.
A few years later, the programme managers raised the issue again in very similar terms: “Are we neutral? We don’t expect individuals to be completely neutral given their proximity to the Palestinians and the frequent imbalances in the conflict, but the organisation itself must use neutral language. We expect international staff (and, as far as possible, national staff) to try to maintain a certain degree of objectivity, to avoid biased and critical language and to stick to the facts”.Internal paper, 2007.
The support by some of the teams for the secular and national programme of Yasser Arafat’s party, the recruitment of employees ideologically close to Fatah or to left-wing parties, an intervention initially designed for a situation opposing Palestinians and Israelis—and not two Palestinian factions—were all factors that contributed to make the political transition in Gaza a perilous experience for MSF.
Translated from French by Mandy Duret
***
Myanmar. “Golfing with the Generals”
Fiona TerryThe author would like to thank Richard Horsey for his comments on an earlier draft.
Whether or not international aid organisations should operate in the repressive, authoritarian state of Myanmar provokes passionate debate. On one side are many exile groups and their supporters—predominantly based in Thailand, the US and the UK—who argue that it is impossible to provide aid inside Myanmar without strengthening the military regime. On the other side are aid organisations that have chosen to work inside the country. They argue that aid can be delivered responsibly and reach people in need of assistance without undue advantage to the junta. The debate is acrimonious and brings out half-truths on both sides: the exile groups exaggerate the regime’s excesses and the benefits accrued from international aid, and in-country agencies, in response, downplay the constraints imposed on them by the military regime.
The experience of Médecins Sans Frontières in Myanmar falls squarely within this polemic. The French section of MSF withdrew from the country in 2006 after five years of efforts to mount an effective malaria treatment programme in conflict-affected areas bordering Thailand.

It publicly denounced “the unacceptable conditions imposed by the authorities” which, if accepted, would render MSF “nothing more than a technical service provider subject to the political priorities of the junta”. “Prevented from working, the French Section of MSF leaves Myanmar (Burma)”, Médecins Sans Frontières press release, Paris, 30 Mar. 2006.
At the other end of the spectrum lies the Dutch section of MSF which runs the largest medical programme of any aid organisation in Myanmar. It treats twice as many AIDS patients as the government and all aid agencies combined, and runs clinics across four of the country’s states and divisions.In 2008, MSF-H was treating 10,000 HIV-seropositive patients and MSFCH 1,000 with antiretroviral therapy compared with 4,000 for the government and other aid agencies combined. See “A Preventable Fate: The failure of ART scale-up in Myanmar”, Amsterdam: MSF, Nov. 2008.
Somewhere in between these positions, wracked with uncertainty, sits the Swiss section of MSF. It has faced major impediments to its projects since it intervened in 1999, but chose to quietly challenge government restrictions and persevere with its medical programmes.
The common explanation—whispered in the corridors of aid offices in Yangon and throughout the MSF movement—for the Dutch section’s success operating in this authoritarian state is that “the head of MSF-H plays golf with the generals”. Like all good rumours, it is part based on fact. Unable to secure a meeting with the regional commander to discuss opening a clinic in a mining area of Kachin State, the head of MSF-Holland visited the golf club in Myitkyina where he knew the commander to be playing, and asked for his authorisation. The request was granted and MSF established the clinic. In the moralistic tones often employed in the aid world, particularly in MSF, this story grew into a generalised myth that the head of MSF-Holland— who stayed an unprecedented fifteen years in the same post—had special relations with certain generals and was for all intents and purposes “a collaborator”. The person in question did little to dispel the myth, avoiding debate on activities proposed, rejecting suggestions of public advocacy construed as critical of the regime, and publicly denying the difficulties of operating in Myanmar.
Nevertheless, that “playing golf” has become a euphemism for “collaboration” is indicative of a broader difficulty all MSF sections faced adapting their principles and methods of working to the Myanmar context. After all, playing golf is a small price to pay for good relations with a commander who determines what MSF can and cannot do for the population. It might be different were MSF asked to buy the commander golf clubs, or renew his club membership. But rather than ana-lysing how MSF-Holland mounted this ambitious programme in such a difficult context and questioning the methods employed, all MSF sections, including the Dutch section’s headquarters in Amsterdam, preferred to stick with, and then turn a blind eye to, the fallacy of an unhealthy and privileged relationship.
This chapter explores the political choices made by the three MSF sections in response to the constraints and dilemmas they faced working in Myanmar. How could two sections of the same organisation have reached such different conclusions over the ability to work in a country? What were the compromises made and strategies pursued by each that lead to such different levels of engagement with the Myanmar people?
The Choice to Intervene
Having no official mandate to determine the types of situations to which it ought to respond, MSF freely chooses where it will and will not offer its humanitarian medical assistance. The French section of MSF began working with refugees from the Karen ethnic group in Thailand in early 1984 and was active until the 2000s in villages and camps along the border and in running cross-border operations into territory held by the rebel Karen National Union (KNU). Although the refugee context was highly politicised, it seemed less problematic to assist victims of the junta outside the country than from within. So when MSF-Holland requested authorisation to enter Myanmar in 1989, it faced considerable scepticism from within the MSF movement.
The Dutch section’s primary rationale for intervening was to investigate health needs in border areas beset by armed conflict, and to be a witness for the outside world of what was going on.“MSF Policy for the Near Future”, Amsterdam: internal document, undated (but from content, circa 1993).
The Myanmar army was conducting brutal counterinsurgency campaigns in several ethnic states bordering Thailand, Laos and China, which aimed to deprive insurgents of a support base by forcing villagers to move to government-controlled settlements and razing their homes and crops. Reports of rape, forced conscription and labour, and summary executions circulated among the communities of 140,000 refugees who escaped to Thailand. Less was known about the hardships faced in Kachin State bordering China, where the Dutch section initially wished to go. Speaking publicly about the causes of suffering constituted an important element in MSF’s desire to intervene.
Repression elsewhere in Myanmar also “qualified” the country for MSF’s attention. Northern Rakhine State is home to Muslim Rohingyas and smaller Hindu minorities who are denied citizenship, and as such are more vulnerable than most to the arbitrary abuse of power by Myanmar officials. Harsh laws govern almost every aspect of their lives, from the age at which they may marry to whether they may travel outside their home village, with sometimes dire consequences for their ability to access medical services. Unlike the Karen and Mon in Thailand, most Rohingyas who fled state repression were not given sanctuary in a neighbouring country, but were twice pushed back from Bangladesh, once in 1978, and again in 1994–95. They returned to similar repression and brutality from which they had fled, exacerbated for many by the seizure of land and property by the government in their absence. Both the Dutch and French sections of MSF worked with the refugees in Bangladesh and were vocal critics of the government’s refoulement to Myanmar and the complicity of the UNHCR in the process.See, for example, “The Rohingyas: forcibly repatriated to Burma”, MSF-Paris, 22 Sept. 1994.
In addition to the border conflicts and generalised repression, the Myanmar people suffer from a state of abject poverty brought about by the incompetence and investment priorities of the junta, which are sharply skewed towards maintaining power and military might over internal and external enemies—both real and imagined. This is especially felt in the health sector, on which a staggeringly low 0.3% of GDP is spent. Millions of people do not have access to affordable and effective healthcare, and are vulnerable to suffer and die from preventable and treatable diseases such as malaria. Myanmar faces one of the worst HIV epidemics in Asia and among the worst TB prevalence rates in the world. Inadequate treatment is causing multidrug-resistance to TB, with repercussions that are likely to be felt well beyond Myanmar’s borders.
Thus there was no shortage of serious health problems to justify MSF’s attempts to work in Myanmar. Although the country has rarely experienced an acute emergency in which large numbers of people were at risk of imminent death (the obvious exception being in the aftermath of Cyclone Nargis in 2008), the “chronic emergency” from which its population suffers is extremely widespread. The problem with intervening lay less in the “what to do” than the “how to do it”. How can MSF assure that in helping the victims, it does not inadvertently strengthen the hand of their oppressors?
Entering the Country
Right from the outset, MSF-Holland faced a major hurdle in its efforts to, quite literally, get a footing in Myanmar. Its request to work there in 1989 was prompted by a small opening in the regime’s isolationist stance which, until then, had limited the presence of aid organisations to a handful of UN agencies and the ICRC. In the wake of international condemnation of the crackdown on pro-democracy demonstrators in 1988 and the imposition of sanctions by many western governments, the regime took a few steps to improve its image, including opening the door a crack to international NGOs. But in an early prelude to demands made after Cyclone Nargis, the military regime was prepared to accept foreign aid but no MSF personnel on its soil. This was a condition that MSF could not accept—it would be impossible to assess needs or monitor the use of aid without the presence of foreign staff. It took two years of negotiations before an international staff member was authorised to stay in the then capital, Yangon. He arrived in January 1992.
In an effort to distance itself from the activities of MSF in Thailand and Bangladesh, MSF-Holland adopted the Dutch version of its name, Artzen Zonder Grenzen (AZG) for use inside the country—a name by which it is still known today (and hereafter will be used). It also entered Myanmar under the auspices of UNICEF, setting up an office in the same building and using UNICEF’s “good name” to establish its credentials.“Situation report, Feb.–16 Mar. 1992”, Yangon, MSF-Holland.
Although the use of “AZG” continues to raise eyebrows in the MSF movement, this was a small price to pay for access if it was indeed the difference in name that shielded AZG from the scrutiny to which MSF-France was subjected when it sought permission to work in-country in 1995. The health minister supported the French section’s request but the higher echelons of the military rejected it, allegedly due to MSF’s cross-border activities and association with the KNU.
It took a much larger opening in the regime’s attitude to the exterior before MSF-France was able to return to Myanmar in 2000. By this stage MSF-Switzerland had also opted to enter Myanmar, having undertaken an exploratory assessment in 1998 at the invitation of the Health Ministry. At this time, international aid organisations were surfing on a wave of unprecedented—albeit relative—openness, instigated by the number three of the regime, Khin Nyunt. The junta had opened its prisons, labour camps and some border areas to the ICRC’s scrutiny, and AZG and other NGOs were expanding operations. The honeymoon was not to last.
Negotiating Humanitarian Activities
Once inside the country, all MSF sections faced constraints as to what they were allowed to do, necessitating some difficult choices and tradeoffs between competing objectives. There were three main areas of compromise that each section made on their ideal ways of working: in their independence to choose where and with whom to work; in their ability to fully control and monitor their aid; and in their ability to speak freely about the underlying causes of health problems in the country.
Independence of Choice
The mistrustful atmosphere into which AZG landed in 1992 did not bode well for much freedom of movement or choice of target population. During the long period of negotiations to enter the country, AZG’s attention focused on the plight of Rohingyas in Rakhine State, following a government crackdown on dissent in 1991 and 1992 which provoked 250,000 to flee to Bangladesh. But access to Rakhine State was not what the government had in mind, and in its first year AZG was directed towards providing healthcare in Shwepyithar township on the outskirts of Yangon. AZG agreed to this proposal for “strategic” reasons, as a “foot-in-the-door” through which to build relationships of trust with officials, and encourage openings in areas with more pressing needs.
AZG was soon confronted with knowledge of a more impoverished township built on paddy fields across the river from Yangon called Hlaing Thayar. In an early test of whether it could, at least at the local level, prioritise assistance to those most in need, AZG requested permission to include Hlaing Thayar in a nutritional survey planned for Shwepyithar in July 1992. In what was a promising sign of AZG’s negotiating potential, the government accepted, and high rates of malnutrition found among children helped to convince the authorities to allow AZG to assist both townships.
Yet, these townships were no ordinary suburbs of Yangon but were areas to which residents of dozens of shanty-towns were forcibly relocated after the regime burned down their homes in the wake of the 1988 student uprising. The shanty-towns had provided a ready source of protesters to join street demonstrations, and passageways through which they could escape capture by police, and so the government wanted them destroyed and cared little for the welfare of their occupants. Fifty thousand “squatters” were moved to Hlaing Thayar in 1989, a figure which had swelled to 164,000 by 1995. “Urban Displaced Program Shwepyithar and Hlaingthayar Townships, Yangon Division, Burma (Myanmar), Jan. 1992–July 1995”, MSF-Holland, 1996, p. 6.
AZG did not fully recognise the dilemma it faced, one which is recurrent in situations of forced relocation. By providing healthcare to the displaced, AZG certainly eased their hardship. But by its presence and participation in the government-run system, AZG was tacitly condoning the government’s forced relocation policy, especially as relocations continued despite AZG’s presence.
The Dutch section did express concern at the forced relocations, raising the health implications with government interlocutors, and showing visiting donors the townships to help expose the regime’s practices. “Burma (Myanmar): Evaluation of the MSF-Holland Programs”, Amsterdam, 1998, p. 24.
But as I discuss later, the impact of lobbying for change within the regime and particularly through outsiders was extremely limited. Had AZG eluded government controls and forged decent relations with the population, perhaps a stronger case for its presence could be made. In an indictment of the limits imposed, one programme review from 1996 recommended holding talks with the highest levels of the Health Department to establish whether an MSF staff member, facing an emergency at the hospital when there was no other doctor or nurse present, was permitted to save a life. “Or should s/he just note down what s/he observes and let the patient die?”“Urban Displaced Program” at note 4, p. 19.
AZG did not lose sight of its target population, and its persistence paid off when it was allowed to visit Rakhine State in April 1993. It was not permitted independent access, but was accompanied by Ministry of Health officials in addition to a police escort for outlying areas. AZG wanted to work in the predominantly Muslim townships from which the highest proportion of refugees in Bangladesh had fled and to which many were returning, but it again had to compromise on its choice of location, obliged to base itself in the state capital, Sittwe. Given that malaria was the leading pathology in Rakhine State, AZG set up a malaria control programme which included training microscopists to diagnose malaria, prevention activities and treatment. AZG also ran mobile malaria clinics in nine townships, which exposed the teams to some of the problems of discrimination and forced labour meted out to the inhabitants of the region. But according to one project coordinator, AZG’s primary goal of advocacy on behalf of the Rohingyas soon gave way to a medical focus. “Although this time was spent travelling in Rakhine, the emphasis was very much on high quality medical and laboratory activities and very little seems to have been reported or written down about the political or advocacy aspects of Rakhine”. “Background of MSF-H Rakhine State Project, Myanmar, 1994–1999”, MSF-Holland, Maungdaw, May 1999, p. 12.
It took another four years before AZG was finally permitted to establish a base in the Muslim enclave of Maungdaw, in January 1998.
An attempt to expand operations to conflict-affected populations in Kachin State ended in last-minute failure in 1995 when AZG did not present the local commander with a personal gift as another NGO had done. But impediments on the political front during this time began to be offset by unexpected successes on the medical front, reorientating AZG’s approach from the “foot-in-the-door” confidence-building efforts to one of “medical diplomacy”—acquiring leverage through its medical expertise and operational volume. The break-through came when AZG was pseudo-officially permitted to carry out a malaria drug-resistance study in Rakhine State with Health Ministry staff in late 1995, which showed the ineffectiveness of the national treatment protocol.The study was published in an international journal as F.M. Smithuis, F. Monti, M. Grundi, A. Zaw Oo, T.T. Kyaw, O. Phe and N.J. White, In vivo sensitivity of Plasmodium falciparum to chloroquine, sulphadoxinepyrimethamine, and mefloquine in Rakhine State, Western Myanmar, Transactions of the Royal Society of Tropical Medicine and Hygiene 91 (1997), pp. 468–472.
The health minister was furious when he saw the publication, but by that time AZG had received permission from lower down to change treatment in Rakhine State from chloroquine and sulphadoxine-pyrimethamine to mefloquine artesunate. When a civilian medical doctor took over as deputy health minister in 2001, the protocol officially changed to the more effective treatment. Through “medical diplomacy” the Dutch section was also instrumental in breaking the taboo over mention of the growing AIDS epidemic in Myanmar, and received permission to start health education and condom distributions in Hlaing Thayar township. Pushing for more, AZG started to care openly for people living with AIDS, both treating opportunistic infections and addressing the widespread stigmatisation of AIDS sufferers through social programmes. Then in August 2003, AZG pioneered treatment of AIDS patients in Myanmar with antiretroviral drugs, challenging the prevailing dogma among health agencies that in-country capacity was too low to allow for little more than health education and social marketing of condoms.“Burma Trip Report, 26 Nov.–5 Dec., 2002” (Draft).
Within five years, AZG was providing over 10,000 patients with these life-saving drugs.
This pragmatic shift to a medical focus reorientated AZG’s target population from those affected by repression or armed conflict to those affected by deadly disease. Malaria clinics, once “alibi projects” to gain access to certain areas, were joined by sexually transmitted disease (STD), HIV and tuberculosis treatment programmes to become ends in themselves. From the late 1990s, project areas were selected by the vulnerability of inhabitants to infectious diseases: (STD) clinics were opened in the jade-mining areas of Kachin State to reduce transmission of venereal disease, and hence HIV, among the itinerant population, sex workers and intravenous drug users. AZG began harm reduction and needle exchange activities, and increased health education about the causes and consequences of HIV infection. Similar projects began in Shan State. With a virus rather than army brutality as the cause, together with growing concern at its spread, the regime placed fewer impediments in the way of AZG’s requests to establish clinics in new areas. This shift proved to be a shrewd political choice that dramatically increased the number of people AZG was able to assist.
Turning to the Swiss section of MSF (MSF-CH), it also had to compromise on its choice of location when it first entered the country in 1999. Although it gave a medical reason—among the highest rates of drug-resistant malaria in the world—as its rationale for wanting to work in the three states of Kayin, Mon and Kayah that border Thailand, MSF-CH had to start work in the coastal region of Tanintharyi Division. “We had to compromise from the beginning and accept to sacrifice our independence with regards to where we wanted to work”, remembers the first head of mission, Patrick Wieland. “We thought that little-by-little we would gain the confidence of the local authorities and gradually reach the border regions”. But the strategy was only partially successful.
We did gain some ground towards the border with malaria mobile clinics, but we were never able to put a fixed clinic where we wanted to. We pushed to get as close as we could and people would come, sometimes from up to 40 kilo-metres away, to access our clinics.E-mail correspondence between Patrick Wieland and Jean-Clément Cabrol, 31 Aug. 2007, p. 2.
As the country continued to open under the influence of Khin Nyunt, MSF-CH obtained access to Kayah State, something no other aid organisation, including the ICRC, had managed beyond visiting the state prison. The Swiss section established a fixed clinic north of the state capital, Loikaw, in March 2004. In the everyday frustrations and constraints of working in Myanmar, simply establishing a base was considered a major achievement in “opening humanitarian space”, even though MSF-CH was unable to reach conflict-affected areas of Kayah State where it assumed—on the basis of reports by border-based agencies—that thousands of civilians were in need of humanitarian assistance. It had to be content that it was at least providing a primary healthcare clinic to which people displaced by the army could come and receive treatment. From that base, MSF-CH kept pressing for authorisation to move closer to areas of low-level conflict with mobile clinics and through its partnership with a local NGO, Karuna.
The French section, when it started programmes in 2001, did not face the same dilemma as MSF-CH and MSF-H in having to begin operations in a different area to that which it proposed. It began a project to improve diagnosis and treatment of malaria, first in Mon and later in Kayin State, through both fixed and mobile clinics, also pushing the limits of areas to which it was authorised to go, often by boat. MSF made large improvements in the medical care of malaria patients in the first year: the case fatality rate among hospitalised malaria patients in Mudon halved between July 2001 and June 2002, and no malaria deaths occurred in the hospital in the second half of 2002.“Activity Report 2002, Objectives 2003”, MSF-France, Paris, 2002, p. 2.
Furthermore, the “foot-in-the-door” approach worked to a certain extent, with projects permitted to expand into new areas such as Ye Township and Kayin State. In the newly accessible areas, the 7,500 consultations held between April and August 2004 exceeded predictions for the entire year.“Myanmar Project Overview 2005”, MSF-France, 2004, p. 5.
This convinced MSF of the need to continue to expand activities towards the border, eventually perhaps to link up with cross-border activities from Thailand. But the purge of Prime Minister Khin Nyunt and his entire military intelligence apparatus in October 2004 sounded the death knell for further expansion for several years.
Control and Monitoring of Aid
The second main compromise the MSF sections made in Myanmar was to relinquish control over their ability to monitor the use of aid at all times. The government periodically imposed tight restrictions on travel to project sites—sometimes affecting only foreign personnel, sometimes all staff—which hindered the supervision of MSF’s projects. As shown above, travel restrictions had long been a feature of working in Myanmar, but these intensified after the purge of Khin Nyunt in an effort to reign in the aid agencies that had expanded operations on his authority. Hardliners replaced more moderate ministers in the government and controls over aid organisations increased: limits on the length of time allowed outside Yangon; prior approval of all new expatriate staff; lists of national staff submitted regularly to the government; lengthy process of registration with a central and line ministry; and more frequent renegotiations of the Memorandums of Understanding (MoU). Aid agencies were also obliged to take a government “liaison officer” with them on every field trip, which had to be organised weeks in advance.
All sections of MSF had to weigh up the effects of these rules on their ability to control and monitor the use of aid, versus what they were still able to do and might be able to do if they persevered. Contrary to claims of some exile groups, government diversion of aid—the common fear when unable to properly monitor its use—was never of serious concern. Unlike the government-sponsored scams seen in North Korea or Ethiopia, any theft of aid that did take place was done at the local, individual level: an area commander commandeering a boat or car for his personal use; the local Township Medical Officer stealing drugs for his private clinic; or Ministry of Health staff selling polio vaccines rather than providing them free of charge. MSF-CH HoM (Nov. 2005–Feb. 2008) “End of Mission report”, Yangon, 12 Feb. 2008, p. 22.
Although frustrating in themselves, the scale of these problems was a far cry from government-sanctioned taxation or the re-direction of aid to “worthy” groups seen elsewhere. It is the fungibility of aid that caused more discomfort than its diversion per se: all MSF programmes assume responsibilities in the health field that should be the remit of government, thereby allowing state resources to be directed elsewhere. Many MSF staff expressed their unease at this, although less so at the macro level, since few believe that the government would allocate more to the health sector if MSF left—the callous disregard shown by the regime towards Nargis survivors in proceeding with the referendum while they buried their dead, put pay to any lingering doubts about the government’s priorities. Rather, this dilemma was felt more acutely at the local level where MSF’s efforts to avoid collaborating with the regime resulted in the establishment of independent health structures—sometimes only metres from a government clinic—further undermining local capacity.Report of Myanmar Visit June 2006, Geneva, 2006, p. 11.
The increased controls over aid activities that followed the purge of Khin Nyunt in late 2004 affected each MSF section differently. MSFCH projects in Kayah State and Tanintharyi Division were deemed off-limits for months on end. MSF-CH persevered with the endless bureaucratic procedures now needed to get staff in-country, only to have them blocked in Yangon. Some even finished their assignment without ever having reached their project site.Interview with Asis Das, former medical coordinator for MSF-France (2005 to 2006) and AZG (2007 and 2009).
The waste of money and human resources this entailed reignited long-standing debates in MSF-CH over whether it should remain in Myanmar or leave. In the end, it was the “stay” view that prevailed, carried by the argument that MSF could not abandon the 500 patients it had recently put on antiretroviral drugs. To do so would be to sentence them to death. Hence in many ways, MSF-CH became hostage to their AIDS treatment programme, changing the parameters of what the section would and would not accept to compromise on in Myanmar. MSF-France, which did not have any patients on ARV treatment, decided to the contrary. The latest wave of restrictions came just as MSF had finally negotiated a permanent base in Ye from which to expand medical coverage. The regime put a stop to it all, preventing any potential witnesses to its crackdown on insurgents and those deemed to support them. The French section withdrew in March 2006, with the programme manager explaining:
“For humanitarian organisations, the issue is to recognize when our role has been reduced to being a technical service provider of the Myanmar authorities, subject to their political agenda and no longer to the goals that we have set for ourselves as a humanitarian organisation. Speaking for the French section’s programmes, we believe that we have crossed that line. It is with great bitterness that we have had to decide to leave the country”. “Why the French section of MSF has ended its activities in Myanmar”, interview with the programme manager, 30 Mar. 2006, http://www.msf.org/msf/articles/2006/03/why-the-french-section-of-msf-ha... (last consulted 26 Jan. 2011).
But even in leaving, MSF-France made a final compromise, stifling its tendencies to rally public opinion and stoke debate about the limits of humanitarian action in such a context.
The Sound of Silence
The French section’s relatively low-key departure subscribed within the logic of self-censorship that marked the third main compromise MSF sections made in Myanmar. “Witnessing” and “speaking out” (témoignage in French) had become an important part of MSF’s action since the 1980s. Cf. infra, Fabrice Weissman, “Silence heals…”, pp. 177–97.
By mobilising public opinion and political players, MSF aims to pressure for change. But in Myanmar, all sections believed that any public comments construed as critical of the regime would jeopardise operations, to the detriment of hundreds of thousands of patients that MSF treats annually. The teams also worried about the safety of national staff if MSF were to incur the wrath of the regime.
For these—and several other reasons related to internal organisational changes at MSF in Paris—the French section left in a half-hearted manner. AZG and MSF-CH have seldom commented publicly on the causes of suffering and constraints to addressing it—except in relation to insufficient AIDS treatment and only then in 2008“A Preventable Fate: The failure of ART scale-up in Myanmar”, cf. note 2.
—in all their years of operation.
Treating the symptoms of repression while unable to address the causes produced discomfort among AZG staff. AZG had intervened in Myanmar to be a witness for the outside world, yet without much discussion or debate, had mounted a medical programme that could be jeopardised by any criticism of the regime’s policies and practices. The obvious tension between the more advocacy-oriented “humanitarian affairs” department (HAD) in Amsterdam and the coordination team in Yangon gave rise to incoherence in programmes and objectives. The HAD produced in-depth internal papers on the plight of the Rohingya and instructed field teams to collect and compile data on incidents, which were shared behind closed doors with donors and non-operational agencies working on these issues. But without a consistent purpose for the data collection over the long years, efforts waxed and waned. It is difficult to discern whether, in fact, the purpose was more about improving the situation for the Rohingya or fulfilling a self-prescribed “duty” of MSF to “witness and speak out”. The disconnect between the perspectives of Yangon and Amsterdam is well illustrated in the Myanmar policy papers from 2001 to 2009, produced at headquarters. Yangon’s bottom line was clearly determined by its medical programme: it was not going to jeopardise its ability to treat 200,000 malaria patients in Rakhine State each year. Yet Amsterdam clung to the belief that witnessing was the primary reason for which AZG should stay in Myanmar.
There might be more that AZG could do to try to ease hardships for the Rohingya if the medical and “advocacy” components of the programme were more in sync. Documenting, compiling and reporting in private to the relevant authorities on impediments to healthcare—such as travel restrictions impeding referrals and the prohibitive cost of passing through checkpoints—could be a less threatening way to bring about change than public statements on these issues, and more effective than back-door discussions with donors.
Influencing the Myanmar regime’s behaviour is notoriously difficult. Richard Horsey, former head of the International Labour Organisation’s office in Myanmar, describes the regime’s strange contradiction that works against both back-door and public pressure:
[The regime] is at once dismissive of outside criticism, but at the same time curiously sensitive about how it is perceived. It seems to genuinely believe it is acting in the national interest, and feels deeply misunderstood, and unfairly treated, by the world at large.Richard Horsey, Ending Forced Labour in Myanmar: Engaging a Pariah Regime, London: Routledge, 2011.
On the one hand, this dismissiveness limits the leverage and influence of external powers, even fellow Asian states, on the regime’s behaviour, rendering futile the efforts of aid organisations to get Myanmar’s allies to pressure for improvements. On the other hand, the regime’s sensitivity to its image provokes a backlash when it is publicly criticised. The generals expelled the head of the UN, Charles Petrie, in October 2007 after he dared suggest in his UN Day speech that the government was not doing enough to address basic human needs. Petrie also raised the monk-led “saffron revolt” of a month earlier, saying “the concerns of the people have been clearly expressed through the recent peaceful demonstrations—it is beholden on all to listen”. “Statement of the United Nations Country Team in Myanmar on the Occasion of UN Day”, Office of the Resident and Humanitarian Coordinator, Yangon, 24 Oct. 20007.
This statement came in the wake of several other public criticisms from agencies working in the country, beginning with the ICRC’s rare public denunciation of a government in June 2007,which accused Myanmar of major and repeated violations of international humanitarian law. The ICRC condemned the use of detainees as porters for the army, and lamented the regime’s refusal to engage in dialogue or to allow the institution independent access to prisons “Myanmar: ICRC denounces major and repeated violations of international humanitarian law”, ICRC press release no. 07/82, Yangon/Geneva, 29 June 2007.
A few months later, thirteen NGOs issued a joint statement calling on the government to ease restrictions on their attempts to help the poorest.Violet Cho, “International Aid Groups Ask Junta to Eliminate Barriers”, Burma News Network, 20 Oct. 2007. No MSF section signed this joint statement.
Petrie’s expulsion quelled further outbursts, and the ICRC’s continued absence from prisons or border areas provides a reminder of the resistance of the regime to all outside influence and pressure.
Neither MSF section lent their support to these initiatives which publicly questioned the regime’s practices. They adopted a more discreet approach, challenging the rules through actions rather than words. Both sections frequently work without proper authorisation, sending teams of national staff to assess the needs of the newly displaced and working for long periods without a valid MoU. They also engage with outlawed groups like sex-workers and drug users, which carries risk of imprisonment for MSF’s national staff, and work on the basis that it is better to apologise after the fact than be denied permission from the outset. In the wake of Cyclone Nargis, for example, AZG did not await permission to send a team to the delta region. Its Bangladeshi and Chinese doctors managed to remain inconspicuous and stayed on long after all other foreigners were told to leave. MSFCH has developed a strategy of “access by annoyance”, repeatedly requesting authorisations to travel, constantly asking for explanations when denied permission, and reiterating time and again its desire to reach those most in need. MSF-CH also sent teams and medical supplies to the sites of street protests during the saffron revolt in 2007 and tried to help the injured, even becoming blocked inside Sule Pagoda at the centre of Yangon when the area was cordoned off by police.MSF-CH HoM (Nov. 2005–Feb. 2008) “End of Mission report”, footnote 2, p.4.
Although largely symbolic in its impact—injured protesters were probably afraid of visibility if treated by foreigners so stayed away—MSF-CH felt this show of solidarity was important, especially in the absence of assistance from other organisations except the ICRC. “Field Visit Report”, Geneva: MSF Switzerland, Oct. 2007.
But for all these acts of “resistance” and the number of patients treated, it is hard not to wonder whether MSF has become too mechanical in its approach, too detached from the context—seeing people in terms of the illnesses they bear rather than who they are and what they are suffering in the larger sense. A recent programme evaluation speaks of the Rakhine project as sclerotic:“MSF in Myanmar: Doubt and Certainties”, Geneva: MSF International Office, Sept. 2008, p. 18. that despite early successes in changing protocols and influencing acceptance of HIV in the country, AZG has not used its sizeable weight enough to push for change, which could include easing travel restrictions on patient referrals.
Whilst it is understandable that MSF prioritises operational presence over public criticism in Myanmar when so little might be gained and so much lost by the latter, it is less so to hear what is said publicly—downplaying the constraints faced by aid organisations, and showing little solidarity with those who would rather change the system and do away with the need for international aid, than merely accept its handouts. The polarised environment is partly to blame for the former, as any admission of difficulties is seized upon by activists and used in arguments against giving aid. But this does not justify the tone and extent of the denial. When asked in an interview what conditions MSF-CH has to accept in order to work in Myanmar, the head of mission mentioned only the MoU, and said that this was no different to what exists in other countries: “The military junta has the right to monitor our activities, exactly as the government would do in France”. He blamed false rumours for concerns about working conditions for NGOs and claimed that MSF knows how to work in Myanmar: “We are very conscious of the practices going on in this country. We know what tone to adopt when we want to intervene in disaster areas, but we also know [how to] denounce when things don’t work as they should”. He ended the interview comparing the lives of the people to that of “almost all developing countries” and blamed the foreign media for “exaggerating” the poor living conditions of the Burmese. “Les conditions de vie des Birmans ne sont pas aussi catastrophiques qu’au Darfour”, Interview conducted by Christelle Magnout, TV5 Monde, Birmanie—l’humanitaire toléré, http://www.tv5.org/cms/chaine-francophone/info/Les-dossiers-de-la-redact... (last accessed 20 Dec. 2010).
In a similar vein, the head of AZG showed a distinct lack of interest in the fate of injured monks and other protesters during the saffron revolt of October 2007. When asked by CNN whether AZG had a moral obligation to demand access to the injured and detained, the programme manager merely said, “If they come to us or if we know where they are we will treat them like anybody else”. Evidently surprised by this response, the interviewer asked the question again. This time the response was more elaborate:
You see, we have a very large programme. We have treated last year more than one million patients, for malaria, AIDS. These programme activities are still going on. We are working for deadly diseases. So it is very important for us to continue the treatment of these patients and this is actually where our staff is busy in these clinics serving these more than a million people.
CNN NEWSROOM TRANSCRIPTS, 7 OCT. 2007, HTTP://ARCHIVES.CNN.COM/TRANSCRIPTS/0710/07/CNR.03.HTML (LAST ACCESSED 10 FEB. 2011).AZG’s shift from concern for victims to concern for “diseases” was complete.
What emerges from the analysis above is that the three sections of MSF pursued very different approaches towards working inside Myanmar, with varying success. AZG initially aimed to assist conflict-affected populations by speaking publicly about their plight, but after several years of failed attempts, greater success on the medical front, and a realisation that public advocacy is likely to prompt an end to its projects, switched its focus to the less controversial area of disease. Given the state of public health in Myanmar and the certain death awaiting those infected with HIV, severe malaria and multidrug-resistant TB, few could argue that this was not a legitimate choice. Moreover, by establishing clinics in high-risk mining areas, AZG probably assisted many displaced by conflict who migrated to these zones.
But the downside to AZG’s approach is that it came at the cost of turning a blind eye to the larger picture. In the narrow focus and routine of the medical programmes, the context became “normal” and the unacceptable accepted, such as forced labour on the street outside a clinic or the crackdown on monks protesting in the street.
MSF-CH, for its part, pursued a relentless quest to access victims of the regime’s brutal policies, which it assumed were found in the conflict-affected border regions. Incredible energy and resources were spent over four years trying to reach sensitive areas of Kayah State. Yet only one year after finally succeeding, MSF-CH transferred its programmes to another NGO for lack of patients. MSF-CH had been understandably reluctant to believe the junta’s claims that few people remained in these areas, preferring to trust the population estimates given by border-based activist groups. But these turned out to be inflated, giving greater validity to AZG’s choice to focus on areas to which the displaced might have gone, such as mining towns. As a consequence, MSF-CH is now following in the footsteps of AZG, tackling infectious diseases in its clinics and in Myanmar’s prisons.
The French section’s strategy, or lack thereof, in Myanmar was the most disappointing. The decision to close operations in Myanmar inspired little debate in Paris and, unlike in contexts such as the Rwandan refugee camps, no thought was given to how MSF’s withdrawal might be used to the advantage of those aid agencies who chose to stay. Few were even informed. MSF-France lacked the imagination and passion it has shown elsewhere to find alternative ways of reaching the population, in defiance of the authorities. Instead of beefing up existing cross-border operations, the French ceased medical runs into Mon State and all but a small TB programme in the Thai camps. This was a far cry from MSF’s determination to continue assisting North Koreans once it had withdrawn from the country in 1998, finding innovative ways to help refugees in China in spite of Beijing’s opposition. Furthermore, in masking its operational inertia with claims to “have been gullible to have believed humanitarian space could exist in Myanmar”,Translated from French, La section française de MSF met un terme à ses activités en Birmanie”, interview with the programme manager, 30 Mar. 2006.MSF-France gave fuel to those arguing that international aid to the country should stop.
Critics of aid in Myanmar are incorrect when they suggest that aid is propping up the Myanmar regime, or that it is a uniquely difficult context in which to work. Nevertheless, aid organisations make some serious compromises when working in the country, particularly in relation to whom they are permitted to assist. Whilst MSF teams on the ground grapple with the dilemmas and difficulties they face, there seems to be little consistent discussion of parameters or benchmarks against which to judge acceptable from unacceptable compromises within any section and particularly across sections. MSF just drifts from one compromise or victory to the next without much assessment as to what worked and what did not, or any overall plan. Both MSFCH and AZG are carrying out some remarkable work in the medical field, assisting large numbers of people. But rather than seeing this as an end in itself, MSF and especially AZG need to rethink how they can use this influence to improve the plight of people whose essential problem is not illness per se but the repression and deprivation at its source. The delicate challenge is to find a way to push for change without exposing patients, MSF staff and allies within the regime to punishment if falling foul of those in charge.
***
Nigeria. Public (Health) Relations
Claire MagoneThe author of this chapter was head of mission in Nigeria in 2006.
It was via a dispatch published in early February 1996 by Agence France-Presse that MSF’s French section in Paris (MSF-F) learnt of the meningitis epidemic affecting the north east and north west of Nigeria. Nigeria is divided into six politico-administrative zones called geopolitical zones: South South; South East; South West; North Central; North West; North East. This chapter focuses on the states of Kano and Katsina, both of which are part of the North West zone.
Deploying a new system of intervention “whose stated objective [was] to build a nationality-less team bearing the MSF label”MSF-France Board of Directors, 22 Dec. 1995(the Emergency Team), MSF’s operational sections in Amsterdam, Barcelona, Brussels and Paris organised a response to the epidemic on a scale unprecedented in the organisation’s history: ninety international staff were sent out to the three worst-hit Nigerian states of Kano, Bauchi and Katsina where, between March and May 1996, they vaccinated 2.9 million people and treated 30,000 patients.
The operation allowed MSF to assert its legitimacy as a responder to epidemics in “open settings” (“closed settings” being displaced persons or refugee camps). This legitimacy was consolidated later in 1996 with an international symposium entitled “Operational Reponses to Epidemics in Developing Countries”, organised to mark its 25th anniversaryInternational medical symposium: “Operational responses to Epidemics in Developing Countries”, Epicentre, MSF Foundation, organised on 25 Oct. 1996 at the Lariboisière Faculty of Medicine. and then, in collaboration with the WHO, UNICEF and the International Federation of the Red Cross, the establishment in 1997 of the International Coordination Group (ICG).

The purpose of the ICG was to ensure the availability of emergency supplies of meningococcal polysaccharide vaccines as world stocks had been exhausted by the epidemics in Nigeria. MSF’s concern with epidemics echoed that of the WHO which devoted its 1996 world health report to the resurgence and emergence of new forms of infectious diseases, which it saw as announcing an imminent “global crisis”.“Fighting disease; fostering development”, WHO Annual Report, 1996.
MSF’s objective was to provide a response to the “epidemic of epidemics”Impact Médecin Hebdo, no. 339—25 Oct. 1996. that its teams had been confronted with since the beginning of the 1990s: cholera in Mali, Côte d’Ivoire, Liberia, Cape Verde, Senegal and Somalia; yellow fever in Liberia, Ebola hemorrhagic fever in Zaire and meningitis in Niger. But this response would also provide the organisation with an opportunity. In the words of Philippe Biberson, president of MSF-France at the time, “aid to refugees currently concerns […] only a tiny proportion of MSF’s projects […]; much of the know-how and experience we have gained is of little use to the missions we’re developing now”. Thus, responding to epidemics in open settings was a chance for MSF to develop new projects while continuing to deploy the medical and logistical expertise it had acquired in refugee camps.
But transferring its know-how from one intervention setting to another meant rethinking its relations with the national politico-administrative authorities. In exceptional settings, such as refugee camps, governments often keep their distance, delegating the health administration of these populations to international agencies and NGOs. This gives MSF the advantage of “extra-territoriality”. It has the margin for manoeuvre it needs to take rapid control of all the stages in the response to an epidemic, including setting up and exploiting a surveillance system for the on-going collection of health data, epidemic investigation (with diagnosis confirmation, when necessary using biological tests) and the introduction of measures for reducing the number of infections and mortality (early detection and treatment of cases, isolation and immunisation and vector control).
In open settings, however, each of these stages must, in theory, be authorised by the host government, meaning MSF’s willingness to take control of the response to an epidemic conflicts with national prerogatives. Should we then deduce from this, as suggested by MSF-France’s president in 1997 that “the freedom of action [of MSF in this type of context] is virtually nil, and the quality of aid provided is almost entirely dependent on the quality of the relations developed with the administrative authorities”?Moral report by president of MSF-F, 1998.
Should MSF’s teams see cooperation with the national politico-administrative authorities as a constraint, a tactical necessity or an objective in itself? To what extent, in what conditions and with what consequences can a government’s health priorities concord with those set by a humanitarian medical actor such as MSF in the management of an epidemic?
This chapter examines these issues by drawing on three specific periods in the history of MSF-Holland’s and MSF-France’s actions in the northern Nigerian states of Kano and Katsina (1996 to 2001, 2005, 2009). However, it is not our intention to imply that the entire history of the organisation’s actions in Nigeria can be summed up in these three episodes. MSF-Holland, for example, whose misadventures in Kano we will be recounting, began responding to medical emergencies in other north Nigerian states as early as 2005. It also ran an HIV treatment programme in Lagos for several years. MSF-France, whose operations in Katsina will be described in this chapter, opened a traumatology centre in 2004 in Port Harcourt in the Niger Delta in a situation of armed conflict and, in 2008, it began an obstetrics programme in the state of Jigawa, followed in 2010 by programmes to treat malnutrition. So this chapter tells only part of the story: MSF’s attempts to respond to epidemics in states where negotiations proved to be particularly complex.
Management and Perpetuation of Epidemics
Following in the wake of the 1978 Alma-Alta conference and the 1987 Bamako Initiative, the decentralisation of Nigerian health services was part of a much broader politico-administrative decentralisation that led to a series of changes in the way the country was divided up and administered. From twelve federal states in 1967, the number increased to twenty-one in 1988 and to thirty-six in 1996, with each state required to work alongside local governments (Local Government Areas, established in 1976), which were allocated a budget and run by a Local Government Council. The number of these Local Government Areas (LGAs) rose from 310 in 1989 to 774 in 1999.
This constant fragmentation has fostered competition and tensions between the different bodies, especially as the LGAs, “rather than representing a coherent community [could constitute] a zone of confrontation between factions associated in an arbitrary manner and opposing “majorities” and “minorities”, chiefdoms, diverse clientele and activist groups”.Guy Nicolas, “Géopolitique et religions au Nigeria”, Hérodote, Paris: La Découverte, 2002, pp. 81–122.
Competition between local, federal and national health services has been particularly apparent in two crucial areas for the response to epidemics: immunisation and epidemiological surveillance.
In 1990, responsibility for primary healthcare was officially delegated to the LGAs and vaccine procurement was decentralised. This led to a drastic reduction in their availability, as the LGAs neglected to budget for them. Immunisation coverage, which had improved considerably as a result of the proactive policy implemented by Babangida’s military regime (1985 to 1993) embodied by Professor Olikoye Ransome Kuti, his health minister, known in Nigeria as “the father of primary healthcare”, began a relentless decline. From 1996 to 2005, the National Programme of Immunisation (NPI), which channelled the huge resources provided by the Global Polio Eradication Initiative Campaign (100 million dollars in 2006),Unicef fact sheet, 2006. was headed by Dr Awosika, a personal friend of President Obasanjo’s wife. The Nigerian media attacked her probity“Why Dr Dere Awosika should go”, Daily Trust, Nov. 2005. and in December 2005, under pressure from donors, she was forced to resign. But she left a sorry legacy: national coverage for full immunisation of children under the age of one was less than 13%National Immunization Coverage Survey (NICS), 2003. Results of a survey of immunisation coverage among children aged twelve to twenty-three months. despite “Nigeria’s immunisation programme [being] by far the most expensive among developing countries around the world”.FBA Health System Analysts, 2005, “The state of routine immunisation services in Nigeria and reasons for current problems”, Nigeria.
Called upon by donors to “restore Nigeria’s dignity and honour in the international public health arena”,FBA Health System Analysts, “The state of routine immunisation services...”.
the country attempted new reforms. From 2006, initiatives financed by international donors were launched to boost primary healthcare and routine immunisation, particularly in the north of Nigeria where the situation was catastrophic. In 2005, the coverage rate in northern states for the full immunisation of children was only 4%. Three years later, it had still only reached 6% and outbreaks of measles were commonplace.
As for epidemiological surveillance, this has been hampered by an uncoordinated accumulation of public and private stakeholders. The federal Health Ministry admitted that “the existing health information system in Nigeria is characterised by extensive duplication of data collection, entry and analysis (no fewer than fifty data forms are in use at the federal level alone); multiple data pathways; lack of standard case definitions; lack of clarity with regards to data submission and responsibilities […]”.Federal Ministry of Health’s National Health Management Information System (NHMIS) unit, 2006, revised policy-programme and strategic plan of action.
Sentinel sites, the infectious disease notification system set up by the WHO, data collected from hospitals, health centres and epidemiology units, demographic statistics, NPI data and information gathered for international partners combined to create a silent cacophony. Health alerts rarely come through official channels, usually arriving too late via the press or individuals acting “unofficially”, such as this employee of the WHO, between 1996 and 2009, who provided MSF with off the record health data, trusting the organisation to ensure “this data [… would] be used to further the A-C-T-I-O-N”.E-mail sent to the head of mission, 2004.
To complicate things further, Nigeria has a system of fiscal federalism that fosters opaque management of public funds. The large majority of federal funding allocations destined for the country’s other two administrative levels are paid into a “Local and State Joint Account” to be shared between the states and Local Government Areas. This constitutional provision encourages clientelist relations, as the two levels are only accountable to each other, and “horror stories”Murray Last, “The peculiarly political problem behind Nigeria’s primary health care provision”, University College London, 2010.
often circulate about the misappropriation of funds. In 1996, federal allocations had just been paid to the Kaduna LGA in northern Nigeria to fund its response to the meningitis epidemic. When governmental medical personnel came to ask for the means to contain the increasing number of cases being registered in the villages, the head of the medical unit responded by saying that there were neither vaccines nor drugs. Instead, he advised them to give the villagers “water injections in place of vaccines for psychological satisfaction”.Elisha P. Rennes, “The limits to health intervention”, Health Transition Review, 7, 1997, pp. 73–107; pp. 91–4.
The absence of control, coordination and efficient management has created cracks in the system that allow interests totally unrelated to public health to take hold with an impunity that grew during the periods of disorganisation generated by the epidemics in Nigeria. MSF was a direct witness to this during a meningitis epidemic in Niger in April 1995 when its teams attempted to use part of a batch of 88,000 vaccines given to the Nigerian Programme of Immunisation the previous month by the Nigerian government and the state of Sokoto. The teams rapidly encountered problems with dilution and found filaments in the vaccines, so they refused to use them. Alerted by MSF, Laboratoires Mérieux, whose name featured on the vaccines, carried out an analysis. The vaccines turned out to be fakes, containing no traces of active products. According to MSF’s estimations, they had been administered to 60,000 people. Mérieux filed a counterfeit suit, followed by an international letter rogatory, but legal proceedings rapidly ground to a halt.Julien Claudel, Le Niger est victime d’une contrefaçon de vaccins”, La Croix, Sept. 1996.
In 1996, MSF was witness to a public scandal that is still being talked about fifteen years on. At the infectious diseases hospital in Kano where its team was based during the meningitis epidemic, Pfizer laboratories was testing a toxic drug called Trovan on children.The use of Trovan for children was never approved by the FDA (Food and Drugs Administration), and its use for adults was restricted in 1999 because of its hepatic toxicity. The drug is banned in Europe.
Four years later, The Washington Post published an article entitled, “As drug testing spreads, profits and lives hang in the balance”.Joe Stephens, “As drug testing spreads, profits and lives hang in balance”, The Washington Post, 17 Dec. 2000.
The article, backed up by testimony from MSF’s teams, revealed the conditions in which these tests had been conducted. It accused Pfizer of using the meningitis epidemic as an opportunity for carrying out large-scale clinical testing without adequate controls, monopolising the already overstretched Nigerian medical staff and neglecting to obtain the informed consent of families too distressed to make a rational decision. At a national investigation committee set up in 2001, MSF relayed the testimony of parents who complained of not having being told they were participating in research. These families, followed by the government of Kano, filed a lawsuit against Pfizer. The case was finally settled out of court in 2009 when the pharmaceutical company agreed to pay 35 million dollars to the families of the children involved in the trials and 30 million dollars to the state of Kano, despite suspicions of complaisance on the part of the state for having authorised Pfizer to carry out the trials. According to a number of observers, some Kano government representatives still hold a grudge against MSF for its role in bringing the scandal to light. Still in government or in other positions of influence, they are thought to have encouraged the Kano health authorities to shun the organisation.
This overview of the context in which MSF was working between 1996 and 2009 shows that it would be unrealistic to rely on the existing system to manage an epidemic with the sole aim of caring for those threatened by it. On the contrary, intervening in such a context implies working outside the system and seeking allies.
Reform from Within
MSF-Holland was the first to pursue the organisation’s objectives in the north of Nigeria, launching an emergency preparedness and epidemic response project which ran from 1997 to 2001.
The initial operational strategy was defined by members of the same team that had coordinated MSF’s action during the major meningitis epidemic in 1996, followed later that year by a measles and cholera epidemic. It analysed the situation as follows: “The federal State has no motivation whatsoever to manage epidemics […] unless they become a political issue. The regime (Sani Abacha’s military regime) is not willing to face the international consequences of declaring an epidemic or the political embarrassment of admitting it can’t control the situation […]”. The team also recommended that MSF carry out targeted projects of limited scope and avoid spreading its resources too thinly. They viewed cooperation with the authorities as a necessary evil: “As a partner in this endeavour, the Ministry of Health can’t always be avoided, but it is not recommended”.Internal MSF document, country policy paper, Nigeria, Apr. 1997.
When the project was first launched in 1997, MSF’s team worked closely with UNICEF and the WHO to train federal and state Health Ministry staff and Nigerian Red Cross personnel in epidemiological surveillance and the treatment of infectious diseases. In 1997, MSF trained forty people from the Ministry of Health in four states and in 1998 it trained 216 in ten states, only to conclude that the programme had had “no significant impact on the ability of the States to respond to epidemics”.Evaluation conducted in 1997 by MSF-Holland.
From 1999, the political situation in the north of Nigeria made it extremely difficult for MSF to pursue its objectives. After thirteen years of military government, Olusegun Obasanjo was elected president of Nigeria and dislodged the representatives of the northern states from the federal political arena. Between 1999 and 2007, these representatives seized every opportunity to assert their identity, threatened by a regime accused of favouring the interests of one region (the south), one ethnic group (the Yoruba) and one religion (Christianity). Control over public health initiatives became the object of a power struggle between the federal state and the states in the north, with MSF caught up in the middle.
In 1999, the MSF programme focused on Kano and set up a “sentinel surveillance system”, which had only just been put in place when a cholera epidemic broke out. Alerted by MSF’s teams, the Kano and federal health ministries denied the appearance of cholera for four whole weeks, refuting the results of laboratory analyses obtained by the organisation. They did not want to be accused of spoiling the FIFA (International Federation of Association Football) under-20s competition which Nigeria was hosting that April. MSF’s reaction was to bypass the system and go to the press. In doing so, it deliberately ignored a warning made by the government in 1996 in a thank-you letter sent by the federal Ministry of Health to MSF’s head of mission after the meningitis campaign: “I have been requested to advise you not to publish any data on these epidemics without the permission of the federal Ministry of Health and would ask you not to issue any statements on these epidemics that may cause embarrassment to the Federal Government of Nigeria”.
That same year, while helping the teams at Kano hospital to manage a sharp increase in the number of measles cases, MSF discovered that expired vaccines were being used on the children’s ward.
In April 2000, MSF’s teams diagnosed a case of yellow fever in Kano, confirmed by a test that had been carried out in a Nigerian laboratory. The risk of a yellow fever epidemic had been identified when the programme was first opened, as the last epidemic dated back to 1986 and there had been no mass vaccination campaign since. Yet there is no treatment for yellow fever and the case fatality rate can exceed 50%. MSF contacted the Kano Health Ministry offering to carry out a vaccination campaign to prevent the epidemic from spreading, in line with WHO recommendations. The ministry at first accepted before retracting and refuting the validity of the diagnosis. The head of mission turned to the religious authorities of Kano, the WHO and the federal government for support in convincing the health authorities, but to no avail. For a while, absurdly contradictory positions coexisted: MSF’s teams were training Kano’s medical personnel in yellow fever vaccination, while their supervisory ministry, in spite of the alert, refused to contemplate such an operation. But the expected epidemic did not occur. The head of mission summed up: “The health commissioner took a huge gamble with the health of his people and, as things turned out, he won”.Internal report, 1999.
After two years of virtually fruitless cooperation, a cholera epidemic and the threat of a yellow fever epidemic treated with nonchalance by the health authorities, in 2001 MSF’s frustration came to a head during the measles epidemic in Kano. The stonewalling, delays and negligence it was to encounter dramatically illustrated the deep-rooted problems in a system that MSF had spent five unsuccessful years trying to change. At the beginning of 2001, Kano’s main public hospital was overwhelmed by a measles epidemic. By March, the surveillance system operated jointly by MSF and the Kano Health Ministry reported more than 9,000 cases in just four weeks, more than ten times as many as the previous year at the same period. The Kano Health Ministry’s attempts to carry out a vaccination campaign were immediately complicated by its fraught relations with Dr Awosika, director of the National Programme of Immunisation (NPI), who requisitioned the medical and logistical equipment needed for the campaign in order to run the National Polio Immunisation Days.
For several weeks, the federal Health Ministry refused entry to the imported drugs which MSF had ordered; it was only after the governor intervened in March that they were eventually authorised. In April it took MSF several weeks of negotiations to obtain permission from the Kano Health Ministry to set up a tent in the grounds of the hospital, despite the fact that the hospital, overwhelmed by the influx of measles cases, had stopped admitting new patients several weeks earlier. MSF’s teams finally managed to take charge of the coordination of treatment in the hospital, working alongside governmental staff. The epidemic was at its height, but MSF struggled to coordinate an unmotivated care team, some of whom decided to go on strike. In May, when the measles fatality rate in the hospital exceeded 25%, MSF asked the health commissioner for permission to carry out an aware-ness-raising campaign to encourage parents to bring their children to hospital as early as possible. He refused, and proceeded to make a public statement in which he played down the health problem.
This was the last straw. MSF decided to confront the Kano health authorities with what it saw as a repeated neglect of their responsibilities and sent a letter terminating its intervention to the Health Ministry, copied to the National Programme of Immunisation, the federal Health Ministry, the religious authorities of Kano, the WHO and international funding agencies. The letter contained a series of criticisms and protestations about the attitude of the health authorities, describing five years of difficult cooperation and bitterly concluding that there was a “lack of political commitment and transparency”, and that “political interests [took] precedence over humanitarian interests, resulting in a senseless loss of human life”. The organisation expressed its “disappointment” in the lack of cooperation on the part of the Kano authorities, which had made no changes despite “numerous discussions with MSF”, and their lack of interest in the training delivered by MSF. The letter was followed by a diplomatic visit to each of its recipients. The main parties concerned gave MSF a good-natured welcome. The Kano health minister thanked MSF for everything it had done and said she would invite the organisation back soon, the federal health minister promised to look into the problems in Kano and the WHO advised patience. This is how MSF’s operational experience in Kano came to an end.
From 1997 to 2001, MSF’s teams were prisoners of their cooperation with the health authorities at a time when, in fact, they needed considerable operational latitude. The failure of MSF’s objectives, at first masked by the consensual nature of its initial collaborations and training programmes, was eventually confirmed by its inability to take action or convince the authorities, and sometimes even the state medical personnel, of the need to take action or, in other words, to change their attitude and their priorities.
In the years that followed, MSF published articles denouncing the Kano authorities’ lack of political commitment towards health issues,Helen Cox and Siobhan Isles, “The beauty and the beast”—The Lancet, 2003. Sally Hargreaves, “Time to right the wrongs: improving basic health care in Nigeria”, The Lancet, 2002.
but they found little resonance in Nigerian public debate.
Voluntary Capitulation
In 2005, MSF’s French section ran a malnutrition treatment programme for several months during a measles epidemic affecting the state of Adamawa in the north east zone of Nigeria. Then in June 2005, alerted by MSF’s mission in Maradi in Niger to the increasing number of malnourished children arriving from Katsina, the organisation decided to carry out an exploratory mission in this state bordering Kano. The situation discovered by the mission was worrying; the people had just been hit by a measles epidemic and, as MSF knew from experience, measles epidemics are usually followed by an increase in the number of cases of malnutrition. To make things worse, the price of cereals was much higher than the previous year at the same period.
After a meeting with the health authorities that included the permanent secretary for health, (second only to the health minister), it took just a few days for MSF to obtain the authorisations it needed to open a programme to treat severe acute malnutrition in Katsina. The permanent secretary was a close friend and the personal doctor of Umaru Yar’Adua, the governor of Katsina and a candidate in the presidential elections due to be held in 2007. The authorities’ initial reception was warm. Looking back, the head of mission at the time describes MSF’s first steps in Katsina as being something akin to “a honeymoon before the wedding”.
At the end of July, MSF opened a nutrition stabilisation centre in Katsina for cases of complicated severe acute malnutrition, as well as six outpatient centres for treating simple severe acute malnutrition, admitting more than 600 children a week. However, as the programme gained visibility and began attracting media attention, MSF’s official contacts quickly began to show signs of concern. The stabilisation centre in Katsina was overflowing and MSF was attempting to open other centres when, in August, a Reuters article was published with the headline: “Child malnutrition hits thousands in Nigerian north”. The article went on to say that Nigeria was not a “destitute” country like neighbouring Niger, which was facing serious food shortages, but a country with a “history of corruption and mismanagement [that had] failed to translate its oil wealth into basic services for the majority of its people”. Needless to say, Katsina’s authorities, who had just publicly announced that they were sending aid to Niger,“Northern Nigerian states send aid to Niger”, Agence France-Presse (AFP), Jul. 23, 2005. were furious. The permanent secretary of Katsina’s Health Ministry had no intention of letting pictures of emaciated children give the impression that the state was incapable of taking care of its people and risk spoiling the start of the governor’s election campaign, a campaign that he himself was supporting.
With MSF’s authorisation to work in Katsina due to expire on 13 September 2005, the situation became increasingly tense. Health Ministry representatives hammered home the same message at every meeting: MSF must leave as quickly as possible and let them take over the programme. And so began a race against the clock, with the ministry pushing MSF to train as many government staff as possible in preparation for taking over the programme and MSF attempting to admit as many children as it could to persuade the ministry that it was not capable of taking charge of such a large-scale project. MSF’s project coordinator commented at the time: “They still think they’re going to turf us out at the end [of the agreement] on 13 September, but if we keep up admissions in the first seven LGAs, and add a few more in the new ones, by the middle of September we’ll have over 2,000 people on the nutrition programme and it’ll be impossible for them to take over and cope with so many patients. We’ll see what happens, but we’re looking to boost the programme as much as we can to have as many beneficiaries as possible (dual objective: care and pressure)”.E-mail correspondence between the team in Katsina and the operational team at head office, 30 Aug. 2005.
As the situation escalated, the teams threatened to “go public” and at one point, after trying to convince the authorities that “without rapid and appropriate intervention 50% of the severely malnourished children [would] die”, MSF report “Results and orientation”, Aug. 2005. even considered opening new centres without authorisation.
In the end, there was no confrontation. The authorities gave MSF a few more weeks and, by the end of September, the number of patients started to decrease. The teams began closing outpatient centres with fewer than a hundred beneficiaries. This resulted in a reduction in the number of referrals of sick children to the stabilisation centre in Katsina and, from that point on, the teams adhered strictly to patient discharge criteria. Soon they were no longer arguing for the opening of a new stabilisation centre.
After fighting to maintain its nutrition programmes in what it had perceived as a severe crisis situation, MSF’s teams seemed increasingly convinced that the organisation had no further role to play when malnutrition was no longer “epidemic”, but had become “endemic”. In November, after a meeting between the coordination team and the team at head office, MSF began closing the programme. It briefly considered communicating publicly about the need to maintain some kind of malnutrition treatment service, but in the end left Katsina as discreetly as possible so as not to compromise its chances of returning in the future. The teams handed the activities over to the authorities, but had few illusions about what would become of them: “We knew that the government wasn’t serious about taking over the activities, although we tried to convince ourselves otherwise as we were leaving. But three days after our departure, the stabilisation centre was empty and they had stopped admitting children into the outpatients programme so they could close it down by the end of January”.Extract from the final report of the Katsina mission, Jan. 2006.
In closing the programme so hurriedly, the Health Ministry’s priority was to remove all trace of MSF and its embarrassing activities before the governor of Katsina began his campaign for the 2007 presidential elections—elections that he went on to win.
MSF’s action in Katsina allowed 12,000 children to be treated for malnutrition during a critical period, due to the teams’ success in negotiating an additional few weeks of operation beyond the original deadline. Once the visibility of MSF’s activities and the media attention they attracted became an embarrassment to the health authorities, the organisation was caught up in a battle of wills. It held its own thanks to two weighty arguments. Firstly, only MSF was capable of managing such a large number of patients and if it had been forced to abandon them from one day to the next, the authorities would have had an extremely difficult situation on their hands. Secondly, with the presidential elections looming, the authorities were more receptive to the threat of going public than usual. By making malnutrition visible, MSF was able to exert direct influence on the authorities. But, by then accepting to make it invisible again, even to itself, it gave up on regarding severe acute malnutrition as a public health problem that its knowhow, innovative skills and influence could help resolve.
Public (Health) Relations
In 2006, as part of a more global strategy for improving its capacity to respond to emergencies in the north, MSF-France set up a mobile surveillance and reaction team of Nigerian doctors. This “emergency pool” soon focused on Jigawa State, where the health authorities were cooperative, and Kano and Katsina States. Designed to be simple and responsive, it was based on a network of willing participants from within the Nigerian health system. The network, developed by MSF over the course of its misadventures relayed alerts to members of the emergency pool who would then try to verify the situation on the ground, assisted by other allies who facilitated their access to field data. Between 2006 and 2008, while managing to respond to a series of medical emergencies in those states willing to cooperate—measles and malnutrition in Yobe, cholera in Borno and meningitis in Jigawa— MSF also made several attempts to respond to alerts in Katsina and Kano. The organisation was never able to obtain official authorisation to gather data or conduct surveys on measles, malnutrition and cholera alerts during this period, and so had no objective justification for the intervention proposals it took to the health authorities. Yet these same health authorities were quite willing to discuss meningitis with MSF. In 2008, its teams were thus able to vaccinate almost 100,000 people in Katsina. Although the circumstances did little to help make the operation a success (late intervention and difficulties in establishing vaccination priorities because of incoherencies in the data from the surveillance system), at least they had the assent of all the health authorities. After a visit to Katsina at the beginning of April 2008, the Nigerian coordinator of the emergency pool remarked: “I must admit that the authorities welcomed the idea of MSF taking part in the meningitis vaccination campaign. But they were against any other form of ‘invasion’, especially in the area of nutrition”.Internal MSF report, Apr. 2008.
Indeed, meningitis, which affects both children and adults, is a disease that has considerable political advantages as far as governments are concerned. Whereas cholera and measles reveal, respectively, the insalubrity of water and sanitation infrastructures and the failures of routine immunisation programmes, and malnutrition highlights the fact that the state is incapable of feeding its people, meningitis epidemics “pose little threat to governments, because in the absence of prevention measures they do not get blamed when people are affected […]. Not only can the government not be held responsible for the scourge, it can ride to the rescue by organising mass vaccination campaigns”.Jean-Hervé Bradol, Marc Le Pape, “Innovation?”, in Jean-Hervé Bradol and Claudine Vidal (eds), Medical innovations in humanitarian situations. The work of Médecins Sans Frontières, Médecins Sans Frontières, 2011, pp. 3–21.
It goes without saying that the governments of north Nigeria were even more keen to organise a response given that what would be a useful public relations exercise was to be largely sponsored by external volunteers such as MSF.
Another occasion for conducting such a public relations exercise arose in 2009 during a large-scale meningitis epidemic which saw the Spanish, Dutch and French sections working simultaneously in nine different states. MSF-France initially concentrated on Jigawa and Katsina, skirting round the intransigent Kano where it had tried in vain to obtain authorisation to intervene before deciding, after two fruitless weeks of negotiation, also to concentrate on the state of Bauchi. In four months, the sections vaccinated over 4.7 million people, with more than 1.5 million in the state of Katsina alone. Immunisation coverage was good, “relations with the authorities [were] very satisfactory and the authorities [were] satisfied with MSF’s work”.Internal MSF document, report on operations, May 2009.
At first sight, the operation was thus a success; it allowed MSF’s teams to take large-scale action on a major public health problem with the assent and then the congratulations of health authorities who were traditionally recalcitrant towards MSF’s interventions. But what real impact did it have on the epidemics?
The polysaccharide vaccine used by MSFSince 2009, it is gradually being replaced by a conjugate vaccine which is supposed to be more effective. induces a weak and transitory immunological memory of about two or three years. It has no immunogenic power in children under the age of two and only limited power in children under the age of four, and it does not eliminate carriage.F. Marc LaForce, Neil Ravenscroft, Mamoudou Djingarey, Simonetta Viviani, “Epidemic meningitis due to Group A Neisseria meningitis in the African meningitis belt: A persistent problem with an imminent solution”, Vaccine, the Official Journal of the International Society for Vaccines, B13-B19, Vol. 27, Supplement 2 Jun. 24 2009.
As early as 1996, at the end of the mass vaccination campaign run by MSF in north Nigeria, research based on observation data gathered during the campaign concluded that because it had taken place several weeks after the epidemic thresholds had been crossed, the effect had been “marginal”, averting only 3.3% of cases in the state of Katsina.Hans Veeken, Koert Ritmeijer and Benson Hausman, “Priority during a meningitis epidemic: vaccination or treatment”, WHO bulletin, 1998.
The medical conclusions drawn from the operation therefore pleaded in favour of an increased focus on patient treatment and early and highly localised immunisation campaigns, rather than mass vaccination during an epidemic, all the more since this last strategy requires massive human and material resources that would be more useful to strengthen patient case management.
Thirteen years later, on the eve of the 2009 meningitis epidemic, the organisation was much better armed to respond effectively. It was no longer in terra incognita and its emergency pool of Nigerian doctors had increased its reaction capacity. Yet the operation was hardly an out-and-out success. A survey carried out by MSF revealed that the efforts of hundreds of its employees in vaccinating 1.5 million people in Katsina prevented the occurrence of 4.4% of cases. Matthew Ferrari et al, 2009, “Katsina State meningitis outbreak: impact of the mass vaccination campaign”, report Epicentre, Mar. 2010. “Time is (still) of the essence: quantifying the impact of vaccination response in Katsina State, Nigeria 2009”, internal Epicentre report 2011. To allow the comparison, we have presented the percentage of averted cases in 1996 and 2009 based on the same method of calculation (described in Robert W. Pinner & al, in “Epidemic Meningococcal Disease in Nairobi, Kenya, 1989”, The journal of Infectious Diseases 1992, pp. 359–364.)
Furthermore, the real impact of the campaign on the decline in the epidemic was as difficult to establish in 2009 as it had been in 1996, as the arrival of the rainy season in May interrupts the transmission of the bacteria.
Therefore, the speed of MSF’s initial intervention in Katsina, though quite remarkable, had only a marginal impact on the effectiveness of the vaccination campaign. For to be effective, the difficulty is “being sensitive enough to react as quickly as possible, but specific enough not to launch unnecessary campaigns”. Eugénie d’Alessandro, “Meningitis: From Practitioner to Prescriber”, in Bradol & Vidal (eds), Medical innovations..., 2011.
In other words, a vaccination campaign must be carried out very shortly after epidemic thresholds have been crossed. However, in Nigeria, organising a meningitis vaccination campaign that satisfies these criteria is an impossible task. The structural weaknesses of the surveillance systems and the time needed to organise such an operation mean that however rapidly the teams react, interventions are unavoidably late. According to the WHO’s epidemic preparedness and response coordinator, the operation was essentially a response to the demands of the authorities and the population, as claiming the right conditions existed for an effective meningitis vaccination campaign in Nigeria would be pure “science fiction”.Interview, Nov. 2010.
Furthermore, the health authorities had stressed the need to make the response appear equitable, the idea being to vaccinate as many people in as many places as possible in order to reassure the population as a whole. It was in order to satisfy this demand that in 2009 MSF’s teams in Katsina agreed to vaccinate certain zones, regardless of epidemiological considerations.
In 1996, during MSF’s medical symposium on infectious diseases, Dr Michel Rey, one of the experts on meningitis who helped devise the treatments the organisation uses today, remarked that: “Until now, all the mass vaccination campaigns intended to control a meningitis epidemic have been carried out after the epidemic peak. This type of action may be beneficial from a political point of view, but it is questionable from a public health standpoint”. Dr Michel Rey, Ligue française pour la prévention des maladies infectieuses—proceedings from MSF medical symposium, 1996.
What were the “political gains” from the 2009 vaccination campaign other than public relations benefits? The Kano health authorities, who MSF hoped would relent when they saw what was being done in neighbouring states, remained impervious to argument. However, those in Katsina opened up and, in 2010, MSF’s teams were occasionally invited in to support health facilities during measles and cholera epidemics. But MSF’s ambitions continued to be restricted to satisfying the demands of the health authorities. It is our theory that, ultimately, MSF’s setbacks with the most recalcitrant north Nigerian states imperceptibly influenced its objectives: in its desire to win over the health and political authorities, the need to act prevailed over the reasons for doing so.
The attempts to respond to epidemics in the north of Nigeria, which were as much attempts to bring to heel those in power, reveal the limits to cooperation between a humanitarian medical operator and health and political authorities. In the face of public health issues, mutual acculturation is not enough to make the divergences between these authorities and MSF disappear, as the organisation’s experience in Kano has shown. Nor can their priorities be influenced by the “saving lives” argument, as seen in MSF’s failed attempt in Katsina. Ultimately, the meningitis episode in 2009 shows that achieving convergence on health priorities between political authorities and MSF can be at the expense of the pertinence of its interventions and risks narrowing its operational horizons down to those of its hosts.
An alternative to this tempering of MSF’s ambitions would be to develop not good relations with the authorities, but the right conditions for achieving a balance of power with them. How? Perhaps by being less predictable, and so less vulnerable, in the negotiations with the north Nigerian politico-administrative powers: by curbing its taste for action when the reasons for acting do not require it, and by taking the risk of incurring the authorities’ displeasure by daring to expose, publicly if necessary, the neglected issues on which it can legitimately deploy its expertise, such as the treatment and prevention of acute malnutrition and measles.
Translated from French by Mandy Duret
***
India. The Expert and the Militant
Stéphane Doyon
In 2005, MSF’s work in the Maradi region of Niger proved the large-scale effectiveness of new strategies based on the use of ready-to-use therapeutic foods (RUTF)Ready-to-Use Therapeutic Foods (RUTF) is the generic name given to sachets of mineral- and vitamin-rich fortified milk pastes used to rehabilitate the nutritional status of malnourished children. Plumpy’nut, manufactured by French firm Nutriset, is a mixture of milk, groundnut, vitamins and minerals.
for outpatient treatment of severe acute malnutrition.Severe acute malnutrition occurs when reserves of fat and muscle disappear as a result of inadequate supplies of energy and micronutrients. The clinical presentation includes marasmus, severe weight loss (defined in terms of variation from the anthropometric norms) and, more rarely, kwashiorkor, characterised by the presence of oedema.
The MSF teams treated 60,000 malnourished children in just a few months and, by the end of the treatment, almost 80% of them were cured. Results as good as these were unattainable using previous treatment protocols, which necessitated the hospitalisation of all children. In 2007, MSF and the Campaign for Access to Essential MedicinesMédecins Sans Frontières set up the Access Campaign in 1999 to improve access to medical tools and treatments suitable for pathologies the MSF teams encounter in the field.
set out to increase access to RUTF by promoting, in Niger for example, the development of initiatives for local production of the milk paste and also actively encouraging research and development. The opportunities for mass treatment offered by RUTF prompted MSF to become involved in regions where malnutrition was endemic and to strive to bring about reforms to national and international nutrition policies.
India, with around 40% of the world’s severely malnourished children,“Maternal and child undernutrition: global and regional exposures and health consequences”, The Lancet, volume 371, issue 9608, pp. 243–260, 19 Jan. 2008.
gives MSF the opportunity to put its political and operational ambitions into practice, especially as malnutrition is not a taboo subject in the subcontinent.

During his speech marking the 60th anniversary of Indian independence in 2007, the Prime Minister Manmohan Singh stated that: “The problem of malnutrition is a national shame. I appeal to the nation to do the utmost to eradicate malnutrition within five years”.“‘Shame’ of India in its 60th year”, Daily Mail, Aug. 2007.
The rate of malnutrition in India remains constant, or may even be increasing, an embarrassment to the government on two levels. First, because it highlights the failure of national initiatives, such as the Integrated Child Development Services programme set up in 1975 and designed to provide children under six with ready-made meals at community health centres known as Anganwadis. Second, it is proof that India’s economic growth has failed to reduce malnutrition, as a number of national and international observers have pointed out. The Indian Association of Paediatricians commented that, “despite improvements in economy, health sector, literacy, and health and nutritional indicators, the prevalence of severe acute malnutrition [as defined by WHO norms] is still unacceptably rife, particularly among children under three years old”.Indian Paediatrics, Vol. 43, 17 Feb. 2006.
The most recent national surveys, conducted in 2005–6,National Family Health Survey (NFHS)—3, 2005 to 2006. show that “infant malnutrition is increasing despite the economic boom” in India, as highlighted by an Indian journalist who specialises in development issues.Patralekha Chatterjee. “Child malnutrition rises in India despite economic boom”, The Lancet, 369, no. 9571, pp. 1417–18.
For example, in Haryana, one of the subcontinent’s most prosperous states, the rate of chronic child malnutrition among under three-year-olds rose from 34.4% in 1998–99 to 41.9% in 2005–06, with acute cases rising from 5.3% to 16.7% during the same period. The international press pushed the point home: “The results [of the 2006 national survey] provide a shocking illustration of how India’s recent economic boom, while enriching the social elite and the middle classes, has failed to benefit almost half of its 1.1 billion people”,Jeremy Page, “Indian children suffer more malnutrition than in Ethiopia”, The Times, 22 Feb. 2007. wrote a Times journalist in 2006 in an article with the provocative heading “Indian children suffer more malnutrition than in Ethiopia”.
For those called on by the prime minister to tackle malnutrition, Right to Food campaign in IndiaThe Right to Food campaign will be referred to as Right to Food in this chapter. More information at http://www.righttofoodindia.org/. occupies a special place. An initiative driven by campaigners, trade unions, people’s movements, NGOs, experts and human rights organisations, it was established in 2001 after the Indian Supreme Court was petitioned to require the government to use its food stocks to combat the food shortages threatening the population. Since then, the Supreme Court, acting on information provided by Indian civil society, issues interim court orders which carry the force of law, enjoining the government to protect the right to food, primarily through guaranteeing access to national programmes such as school canteens, food distributions and work for food programmes.
According to Right to Food, malnutrition has to be examined from all angles: the deepening agrarian crisis, public policies that ignore children, gender inequality, the dismantlement of the public distribution system, the caste system, as well as the growing influence of commercial forces in the manufacture of products for infants, genetically modified seeds and experiments in biotechnology. Its members organise demonstrations, publish scientific analyses and draft proposals for legislation to alter the legal framework and content of national social and food programmes. As some members hold official positions, their opinions are more likely to influence the process of changing India’s policies and laws. For instance, Biraj Patnaik, one of the key persons of Right to Food, is principal adviser to the Commissioners of the Supreme Court on the right to food.
Right to Food calls on a whole range of strategies to exert pressure, including legal activism, raising awareness and protest. It also consults and works with the state, which it sees as having a specific role to play in as much as it is responsible for ensuring the food and nutritional security of the Indian people through improving the quality of its services. Therefore, neither the Indian state nor Right to Food will allow the issue of malnutrition to be addressed by foreign aid organisations, accused of defending their own interests to the detriment of the common interest. In 2003, India banned food aid donations from US NGOs because it considered the enriched flour distributed liable to be contaminated by genetic modification, and thus unfit for human consumption.“India bars entry of NGOs’ modified Corn-Soya Blend”, Indian Express, Express news service, 6 Mar. 2003.
Indian civil society organisations took this as proof that this type of overseas aid “was nothing but a prelude to opening the doors for commercial dumping of [genetically modified] foods by the US multinationals that are unable to find markets in Europe”.K.S. Jayaraman, “U.S. food aid to India still under GM cloud”, Crop-Choice news, in Nature Biotechnology, Vol. 21, no. 4, Apr. 2003.
Differing Ideas About Malnutrition
MSF and Right to Food would appear to have a common enemy in malnutrition; however, each organisation perceives different realities and different solutions, as was immediately apparent when they first met in 2008. For MSF, tackling a public health issue of this kind demands first and foremost providing an answer to the medical emergency, in this case acute malnutrition, where the body starts to consume its own tissue in order to find the energy and nutrients it needs to survive. However, this is not a concept favoured in India, where malnutrition is seen as a problem that slows down children’s development and reveals that their food needs are not being met. Put another way, where MSF sees malnutrition as a potentially fatal condition that has to be combated through the use of appropriate treatment, Right to Food perceives it primarily as a signifier of social injustice that entitles its victims to receive assistance from the state. These diverging concepts underscore the differences in the way to finding priority solutions to malnutrition.
The development of an outpatient nutrition rehabilitation system had been under debate at MSF ever since the first experiments in Niger in 2002, as it required a shift in the organisation’s practices and assumptions.Isabelle Defourny, “Operational innovation in practice: MSF’s programme against malnutrition in Maradi (2001–2007)”, in A Not-So Natural Disaster: Niger 05, Xavier Crombé & Jean-Hervé Jézéquel (eds), London: Hurst and Company, 2009.
Handing over most of the responsibility for administering nutritional treatment to the children’s mothers meant giving up close monitoring of a child’s medical condition, as under previous protocols and during the hospitalisation they necessitated. Paradoxically, the medicalisation of malnutrition entailed a degree of demedicalisation in the way that MSF worked, rendered acceptable in terms of medical effectiveness by the introduction of RUTF. Switching to the use of ready-to-eat pastes meant no more careful preparation of water- and milk-based therapeutic rations under conditions of strict hygiene, and that nursing care was no longer as necessary in treating children. In fact, no matter how severe the malnutrition, providing that the child wants to eat, s/he can be given individual milk paste sachets and allowed to go home. Treatment dosages are very simple to follow and a weekly check-up on the weight curve is quite sufficient.
However, whereas MSF saw RUTF as a chance to simplify the distribution, administration and use of nutritional treatments, essential if medical responsibility was to be delegated to the families of malnourished children, Right to Food perceived a risk of exacerbating poverty and social demobilisation. Its members felt that the response to the issue of malnutrition had to include increasing points of contact between marginalised groups—women, lower castes—and the rest of society. Over four million Indian womenLeena Menghaney, “Winners and losers in India, a major crisis in a booming economy”, MSF website, Mar. 2008. are employed preparing meals for children, a task that offers great scope for social interaction.
Plumpy’nut, the therapeutic food used by MSF in most of its programmes, is a commercial product made overseas and patented in a number of countries. Plumpy’nut is protected by several patents owned by Nutriset until 2021 in twenty-nine countries, not including India.
Some members of Right to Food viewed it as a Trojan horse for the very international food industry that the campaign is committed to fighting against.“Not Biscuits, Cooked Food in Mid-Day Meal Scheme: Minister”, Thaindian News, 17 Mar. 2008.
In April 2008, its members staged a protest during a meeting organised in India by GAIN (Global Alliance for Improved Nutrition), an international foundation linked to private business whose stated aim is to combat malnutrition by making sure that suitable products are available on the market. During the meeting, Right to Food members demanded that GAIN “spare India from its strategy that seeks to build promising markets for multinationals and the food industry [such as] Unilever, Cargill, Danone and Wockhardt” and congratulated the government for not “succumbing to the biscuit manufacturers’ lobbies and resisting their attempts to replace distributed hot meals [as part of the government nutritional programmes]”.“Media Brief. People call Upon GAIN to Leave India and Government of India to Regulate PPPs”, CNN report, 16 Apr. 2008.
The most vocal and radical wing of Right to Food against the commercialisation of food and the industry’s conflict of interest is the BPNI (Breastfeeding Promotion Network in India), which grew from the movement to fight the sales strategies used by Nestlé in Africa during the 1970s to promote its baby formula products. The coordinator of the world’s largest network for the promotion of breastfeeding, Dr Gupta, accused MSF of the “legitimisation of commercial products for feeding young children […] by creating a simplistic solution for child malnutrition”. Arun Gupta, “Commercialising young child feeding in the globalised world: Time to call for an end!!”, 2009, www.rtfn-watch.org.
Dr Gupta was all the more suspicious because of MSF’s stated aim of using RUTF derivatives to prevent malnutrition, as expressed in its public documents and at international scientific conferences. He declared that: “The story of one success in an emergency situation [in Niger] is quickly being translated into a mainstream intervention for preventing and treating severe child malnutrition. […]. Once we start using RUFs [ready to use foods] as a preventive strategy, as is being voiced by these international agencies, child nutrition turns into a big market”.Gupta, “Commercialising young child...”, 2009.
It is against this background that three different approaches were set in motion by three different organisations, all apparently inspired by the same goal of treating severe acute malnutrition in India. These were direct and discreet action, led by MSF-Spain; the alliance with Right to Food, incarnated by the Access Campaign; and the strategy of the widespread fait accompli, as adopted by UNICEF from 2008.
Take Action and Prescribe
In August of 2007, Bihar State was hit by flooding and MSF-Spain set up a two-month mobile consultation service in Dharbanga district. During this period, the MSF teams identified a large number of malnourished children and treated around 1,000 of them with Plumpy’nut. MSF closed its programme once the floods abated, but decided to carry out a nutritional survey in the area. Their suspicions were confirmed: 20% of children were suffering from acute malnutrition, and almost 5% were severely malnourished, Retrospective mortality, nutrition and measles vaccination coverage survey, Dharbanga district, Bihar state, India. June 2008, MSF-Spain, Epicentre. sufficient according to established international standards to constitute an emergency situation. A food security survey conducted by MSF found that malnutrition “is not episodic and related to the 2007 floods, but is an endemic, long-term problem”. Livelihoods and risk of malnutrition in Dharbanga, Bihar. MSF report, Apr. 2008.
So MSF decided to set up a programme in Dharbanga district. In geographical terms, the choice stemmed from the gravity of the nutritional and health situation seen to affect the population and to which no local responses were forthcoming. Being directly confronted with this state of affairs led MSF-Spain to decide to take action on the question of malnutrition, and in 2008 it began talks at the local level. In the words of the programme manager: “This project was not driven by a political agenda set by the organisation’s head offices. It started in the field […]. We still don’t know where it will lead, but we have to accept an element of trial-and-error and uncertainty. The main thing today is to be able to save these children’s lives”.Jean-Hervé Bradol, Jean-Hervé Jézéquel, “Child undernutrition: advantages and limits of a humanitarian medical approach”, part of the Cahiers du CRASH collection, p. 18.
A remote area with very few social and medical facilities, it is regularly affected by widespread flooding during the monsoon season, causing people to flee their homes and making access extremely difficult. Although such precarious conditions were sufficient to justify action, they also represented obstacles, potentially undermining MSF in achieving its goal of substantiating the programme’s results, which required ongoing monitoring of patients, including in their own homes, in order to be able to establish the “scientific proof” that would help to convince Indian public opinion.
MSF-Spain was not primarily seeking to prove the effectiveness of its strategy, or to transform the way that nutritionally fragile children were cared for at the national level; it sought simply to act immediately and locally. The modesty of its aims was motivated by the desire to avoid repeating its recent experiences with the treatment of visceral leishmaniasis, another pathology endemic to India with 80–90% of known sufferers in Bihar State. Aiming to bring about a change in the national treatment protocol, MSF had worked very closely with the Health Ministry and an Indian research institute, as well as conducting lengthy and elaborate negotiations with local and national authorities before finally arriving at the first phase: authorisation to use the treatment of its own choosing in its programmes. MSF felt, as it said publicly, that all this had taken too much time: “After a drawn-out year-long bureaucratic process, MSF-Spain has started to receive and treat patients suffering from visceral leishmaniasis”.“India: MSF comienza a tratar pacientes de kala azar”, [India: MSF begins treating patients with kala azar], MSF press release, Aug. 2007.
So the Spanish section set out to treat malnutrition immediately and swiftly, avoiding or ignoring as far as possible the procedural straitjacket that it had encountered when attempting to alter nationwide practices in the treatment of leishmaniasis. Initially seeking a low profile for its activities, the organisation hoped that in due course its programme results would speak for themselves and enable it to lobby in favour of changes to malnutrition treatment in India.
On the other hand, the Access Campaign which supported MSFFrance’s objective of starting a nutrition project in India as of 2007, was determined right from the start to play a part in reshaping national practices and policies: “The idea was to set up a pilot programme to show that this was a do-able and effective way of treating severe acute malnutrition and […] to play a part in spreading the word about this type of treatment across the country, inciting civil society, intellectual and political leaders to take up the cause”.Bradol & Jézéquel, “Child undernutrition: advantages and limits...”, pp. 39–40.
The MSF section decided to turn to the Access Campaign’s Indian office, set up in 2005 to lobby for a legal and judicial framework in favour of domestic production of low-cost generic drugs and working hand-in-hand with other civil society organisations across India. One key person of the Access Campaign India, and with close ties to Right to Food, forecast the failure of a project parachuted in from outside, and advised that the section should work closely with Indian civil society and the government to seek an Indian solution to malnutrition. Yet, this person accepted to be part of an MSF evaluation team with two ardent proponents of the widespread use of RUTF, which visited a district in Orissa State during July 2008. A rapid examination of children based on an evaluation of their brachial perimeters revealed that one in ten was suffering from severe acute malnutrition,MSF internal visit report, MSF, Aug. 2008. a reality that the representative of the Access Campaign India had never previously encountered. Striving to find treatment solutions, the team discovered that the local government programme canteens had no food to offer. It also found that local stores only stocked what one team-member dubbed “compassion treatments” for malnutrition, meaning foods whose composition failed to meet the specific needs of malnourished children. By the end of their evaluation, the three members of the team were in agreement: government and market were both unable to offer solutions to the problem of severe acute malnutrition, but there was a network of local community organisations that a potential treatment mechanism could work with.
In August of 2008, a few weeks after the evaluation team’s visit, floods once again struck India. The prime minister declared a national disaster and appealed for international assistance. MSF-France stepped in to provide primary healthcare to people living in one of the coastal areas of Orissa, and began the lengthy process of negotiating with local authorities to set up a nutrition programme.
At the same time, the dialogue between MSF and Right to Food campaigners was progressing with every meeting, facilitated by the members of the Access Campaign India as go-between, and regular visits from the Paris-based Access Campaign representative. Despite their initial differences of opinion, the people involved had confidence in MSF. They knew about its battles with the pharmaceutical industry on ensuring access to generics, and they were also increasingly sensitive to the need to develop a curative approach in the face of the eight million Indian children suffering from severe acute malnutrition. This awareness echoed the plea issued by the Indian Association of Paediatricians for the adoption of an outpatient care model: “India only has 900,000 hospital beds. It is therefore impossible from an operational point of view to admit all these [malnourished] children, which makes home-based treatment strategies an inevitable alternative”.Indian Paediatrics, Volume 43, 17 Feb. 2006.
In December 2008, Right to Food representatives met with MSF to debate the issue of care in India for cases of acute malnutrition. Participants were Right to Food members most closely involved in nutrition issues, and a doctor from the National Institute of Nutrition was invited to offer a counterweight to MSF’s scientific expertise and discuss the possibility of drawing up joint documents on relevant experiences. Once again, the talks foundered on the question of treatment: for Right to Food, there could be no question of accepting imports of RUTF. MSF thought that it was moving in the right direction when it announced that local production would soon come on stream, working with companies located in India, such as CIPLA and Compact,CIPLA is an Indian pharmaceutical laboratory specialising in the production of generic medicines and Compact a Norwegian company specialising in the production of high-energy biscuits and nutritional supplements. and with whom it was already in negotiation. But the campaigners were adamant that commercial interests had no place in the production of a common good: they wished to support an economic model with a community-based, cooperative or public structure, preferably on a small scale. The product would have to bend to this imperative, not the other way around. The MSF position was that centralised, industrial production of RUTF would offer the best quality guarantees—product standardisation and packaging and controlled hygiene conditions—but the campaigners maintained that, because of the size of the subcontinent, it was better to risk recurrent localised quality problems than an industrial incident affecting the only production line.
MSF undertook to encourage production initiatives of the type supported by Right to Food. However, it also stated that it would use imported products in the treatment of malnutrition, because “the priority is to treat the children and if their treatment is not to be delayed we have to use whatever therapeutic products are available; it will take a long time to agree on a new local formula”.MSF visit report, Dec. 2008.
Approval was granted at the end of the meeting. Mindful of the imperative to do something in the face of a lamentably persistent problem, the campaigners agreed that MSF could start nutritional campaigns using imported RUTF, so long as it had no implications for the state-run programme, and they called on the organisation to come forward with scientific proof that its recommended strategies could be adapted to the context of Indian malnutrition.
Yet, even while MSF-France and MSF-Spain were in negotiations on opening their respective projects in Bihar and Orissa, the whole situation changed as a consequence of a more aggressive strategy adopted by UNICEF.
A Medical Coup d’État
UNICEF had been running a programme to combat severe malnutrition in Madhya Pradesh since 2006. It was a hybrid programme combining WHO-designed norms for detection and treatment of severe acute malnutrition and Indian practices, which differed primarily in terms of the criteria used to identify malnutrition. The programme ran Nutrition Rehabilitation Centres which offered fifteen-day in-patient care to children who were malnourished by Indian standards, i.e. chronically malnourished, and below the norm for their weight/height, as well as children who were severely emaciated. The Madhya Pradesh health authorities were amenable to UNICEF’s innovation, which was to medicalise malnutrition treatment, and they helped to expand the programme; by the end of 2008, there were 182 Nutrition Rehabilitation Centres in Madhya Pradesh State.
However, for new UNICEF chief nutritional advisor Victor Aguayo, nutrition advisor to the UN in Niger in 2005 and who arrived in India in 2008, the model was overly restrictive: it required hospitalising a large number of children who could be treated as out-patients; it failed to offer a suitable solution to children suffering from chronic malnutrition; and the production of the foods was not standardised and was based on foodstuffs purchased locally and therefore not fortified with the vitamins and minerals essential to the children’s recovery. His observations were backed by two international nutrition experts invited by UNICEF to report on its programme. UNICEF then decided to modify its programme protocols by introducing imported products whose quality it could vouch for. Its representatives decided to override the objections to the use of imported industrial RUTF raised by Right to Food. As became apparent during different discussions between MSF and UNICEF managers in 2008, UNICEF, having witnessed Right to Food’s outspoken intervention at the meeting held by the Global Alliance for Improved Nutrition (GAIN), considered the civil society alliance to be a radical movement whose influence was restricted by their ideological heterogeneity. UNICEF therefore decided to restrict itself to dealing with state representatives alone, using an imperious argument as a justification for its reforms. The UNICEF representative in Madhya Pradesh declared: “RUTF has been a real revolution. India simply cannot say no to its use”.“India tries new way to reach its underfed children”, Reuters, 18 Mar. 2008.
Ironically, it was Right to Food that provided UNICEF with the opportunity to implement its reform. As campaigning got underway for the Madhya Pradesh legislative elections, to be held at the end of 2008, Right to Food’s local section tried to push malnutrition onto the agenda. The state was known to be the most affected by severe malnutrition, with an estimated 1.26 million children afflicted each year,NFHS-3. 2005–6. and that year it was also suffering from drought. The campaigners blamed the “Madhya Pradesh government [which] seems deaf to all news about the scourge of hunger across its state [and] refuses constantly to recognise what’s going on, saying that malnutrition is not the real reason for these children’s deaths”.Right to Food Campaign Madhya Pradesh support group, “Moribund ICDS”, pp. 22–23.
The media took up the story, backed by hard-hitting pictures taken in the UNICEF-supported government nutrition centres.
UNICEF grasped this opportunity to suggest a face-saving solution to the government, embarrassed by Right to Food’s statements: authorise treatment strategies using Plumpy’nut, which promised fast and
effective results. Faced with a health and electoral emergency, the Madhya Pradesh government approved the initiative without, however, making it official. In August 2008, use of Plumpy’nut was introduced at nutrition centres in two districts where the media had reported a great many deaths of children. Soon afterwards, flooding in Bihar gave UNICEF further grounds for taking action and it introduced Plumpy’nut there as well.
However, in October 2008, Right to Food members in Madhya Pradesh found out that UNICEF was handing out sachets of the imported food, Plumpy’nut, to children without federal government authorisation or prior consultation, and in breach of the Supreme Court’s 2004 ban on the use of centrally procured commercial foods in national food programmes.
An emergency meeting attended by UNICEF and Right to Food was called in Madhya Pradesh. The principal adviser on the right to food to the Supreme Court, Biraj Patnaik, who had helped MSF nationally and internationally in highlighting malnutrition issues, tried to intercede in favour of expanding malnutrition treatments to embrace new approaches, while requiring them to be adapted to suit the Indian context. But the campaigners were highly suspicious of UNICEF: the organisation was accused of having violated the principles of national sovereignty by importing Plumpy’nut and setting up a protocol new to India without consulting the national authorities. Its ties with GAIN encouraged the idea that it was seeking primarily to open up a market for food multinationals. As provided for under the Indian constitution, Right to Food initiated a procedure requesting information from the government and demanding an investigation into how RUTF was introduced and the Indian state’s responsibility in the process.
In February 2009, the ministry responsible for approving UNICEF’s activity plan asked it to withdraw RUTF from its budget since the government did not allow them. The UN agency’s programmes were cut off from their supplies. At the same time, apparently alerted by the more radical elements of the BPNI, a member of the national parliament put a question to the minister of health: “Is the Minister aware that UNICEF and MSF have imported industrial nutrition foods without government approval?” C.K. Chandrappan, starred question, 25 Feb. 2009.
Challenged in public to make a show of force, the Indian government ordered UNICEF to explain itself. The UN agency offered as defence the acute necessity for emergency action after the floods in Bihar and the drought in Madhya Pradesh. In a letter sent in May 2009, the minister of health reminded the agency that it was bound to obey national laws and that, in particular, it had to respect national sovereignty on nutrition and emergency response. The government further demanded not only that use of RUTF cease, but that remaining stocks be shipped out of the country and a programme of equal value be made as payment.
This dramatic turn of events had immediate consequences for MSF-France. Negotiations with the Orissa State government, which had been dragging on for several months, collapsed. The local authorities had no intention of stepping out of line with the federal government and suggested that MSF try and sort the problem out in Delhi. After a full year of talks, which had already lasted far too long in the minds of most head office desk managers, MSF decided to pull its team out and to abandon its project.
However, MSF-Spain did manage to sign an agreement with the Dharbanga district health authorities to start a project in early 2009. Admittedly, its initial scope was limited to treating severe acute malnutrition with RUTF, with no provisions for conducting research. The Spanish section had resolved to focus on setting up a local agreement so that it could start providing treatment as quickly as possible. Shielded by the discreet nature of its activities, the modesty of its stated aims, the remote area where its work was restricted to, as well as an unvoiced “live and let live” agreement with Right to Food, the Spanish section’s programme went ahead unaffected by the turmoil surrounding UNICEF.
Operational Failure, Public Health Success
The Plumpy’nut controversy might have led to a halt to UNICEF’s nutrition programmes, but it also triggered a national debate and considerable domestic media coverage on the question of how to “Indianise” treatment for severe malnutrition. MSF continued to play a part in the debate, alongside the All India Institute of Medical Sciences, the Indian Association of Paediatricians, Right to Food and various government representatives. In order to cut short arguments about the danger of the links between the product and the food industry, RUTF were renamed Medical Nutrition Therapies (MNT). During a consensus-building meeting held in November 2009, the Madhya Pradesh health commissioner, one of the people driving treatment for severe malnutrition in the state, presented the results of the programme set up with UNICEF. The results showed that over 33,000 children had been treated during the period 2006 to 2008, and that the use of fortified milk pastes was effective. Ironically, therefore, the very first discussion on experiences in India concerned a programme whose clandestine nature had been denounced by Right to Food and was now defended by the very people who had worked to stymie UNICEF—the Madhya Pradesh section of Right to Food.
The report on the meeting, published in the Indian PaediatricsIndian Paediatrics, Vol. 47, 17 Aug. 2010. journal, recommended that consideration be given to treating malnutrition with “medical nutrition therapies”, provided that said treatments were produced in India and the protocols examined by national experts. The editorial to the journal declares that: “Philosophical differences are evident regarding the choice of interventions to be adopted in the community. One view favours the sole adoption of the preventive and promotive aspects (ensuring basic nutrition and health care for all infants and children, especially promotion of breast feeding and appropriate complementary feeding) with no special emphasis on active detection and nutritional therapy of SAM children. […]. We firmly believe that public health interventions for SAM must simultaneously focus on preventive and promotive aspects, and therapeutic interventions in the community”. Indian Paediatrics, 2010.
So “Indianisation” of treatment for malnutrition is underway, its pace dictated by the speed that consensus can be reached between activists, government representatives, scientists and invited experts, a group that includes MSF. There is now unanimity about the necessity of providing treatment for severe acute malnutrition in India, but a lot of ground still needs to be covered before malnutrition ceases to be a “national shame” and becomes a controlled public health issue. First, national nutrition stakeholders insist that anthropometric criteria for the identification of malnutrition have to be adapted to the Indian context. They want to ensure that thin children are not required to submit to international corpulence standards, and that the result will genuinely focus on reducing mortality and the consequences associated with the pathology. Working in collaboration with Indian research bodies, the health and family welfare ministries have launched initiatives to test and compare community-based treatment models that could be incorporated within the national system, i.e. those that do not require radical upheaval or additional human resources, which they do not want to commit. MSF can be a catalyst in this public health debate, providing that it can provide answers to questions that remain unresolved by using the results of the programme in Bihar, which had already treated over 6,500 children between March 2009 and February 2011.
But the question of the treatment itself is still up for debate and continues to be divisive, even within Right to Food. Progress on this front may well come as a result of an alliance of very different stakeholders. In early 2011, the health authorities and Right to Food members in Madhya Pradesh held talks with the international experts behind the RUTF concept on the possibility of creating a local Indian formula. This alliance has made contact with various local institutions, national food companies and India’s food and agriculture cooperatives, one of which, a cooperative with 2.9 million members who are all small-scale producers, boasts the unequivocal slogan: “The Taste of India”.
Translated from French by Philippa Bowe-Smith
***
South Africa. MSF, an African NGO?
Michaël Neuman
On the eve of the new millennium, Médecins Sans Frontières launched programmes providing access to antiretroviral (ARV) treatment for HIV-infected people. Although national and international initiatives for promoting access to treatment were evolving rapidly at the time, there were still major barriers in the poorest countries, particularly in Africa. The priority was prevention, mainly because of the high price of medicines (between 10,000 and 15,000 dollars per treatment and per year for triple therapies in 2000), but also because existing medical infrastructures and education levels were considered not to be of the necessary standard.For a more detailed analysis, see Jean-Hervé Bradol, Élizabeth Szumilin, “AIDS: A new pandemic leading to new medical and political practise”, in Jean-Hervé Bradol & Claudine Vidal (eds), Medical innovations in humanitarian situation. The work of Médecins Sans Frontières, Médecins Sans Frontières, 2011.
Some argued that Africans wouldn’t be able to take medication at the right time because “…many people in Africa have never seen a clock or a watch in their entire lives”.John Donnelly, “Prevention Urged in AIDS Fight; Natsios Says Fund Should Spend Less on HIV Treatment”, Boston Globe, 7 June 2001.
However, MSF saw South Africa and its sound medical infrastructure as the appropriate setting in which to prove that treating the sick was possible. More than five million people in the country were infected with HIV and had no access to treatment other than that provided at a handful of private facilities.
In 1999, Dr Eric Goemaere, former executive director of the Belgian section of MSF, arrived in South Africa to investigate the opportunity of opening a project for preventing mother-to-child transmission of the HIV virus (PMTCT). After first being stonewalled by the national authorities, he met Zackie Achmat, one of the founders of the Treatment Action Campaign (TAC), a movement formed the previous year by a small group of activists from the anti-apartheid movement to advocate for access to treatment for people with AIDS.

Zackie Achmat pointed Eric Goemaere in the direction of Khayelitsha, a township on the outskirts of Cape Town, where the Western Cape Province medical authorities had set up a pilot PMTCT project without the knowledge of the South African Ministry of Health. Khayelitsha had more than 500,000 inhabitants and the HIV prevalence rate among pregnant women was 15%, twice that of the province as a whole.Khayelitsha annual activity report 2008–2009, Médecins Sans Frontières/ University of Cape Town.
MSF was also interested in the Western Cape because of its unique political context. The province was in the hands of the opposition and MSF felt that this might afford them some room for manoeuvre. Indeed, the new provincial authorities saw in the lack of access to the new treatment options a means of shoring up their criticisms of the ANC (African National Congress).
In February 2000, MSF and TAC joined forces to set up a programme to treat opportunistic diseases, a programme linked to an AIDS education and information project, which involved the patients themselves. In order to pressure the South African authorities into extending the provision of HIV/AIDS care, MSF and TAC considered it crucial for the programme to be owned by poor and black patients, judged by both organisations to be the legitimate voice of contestation in the domain. In this respect, and inspired by contacts with organisations such as Act Up, the movement was continuing in the wake of the European and American activists of the 1980s who had wanted to “challenge the asymmetric relationship between doctor and patient, occupying the domain of the former to make the latter actors in their own treatment”.Jean-Pierre Dozon, “De l’intolérable et du tolérable dans l’épidémie de sida. Un parallèle entre l’Occident et l’Afrique”, in Didier Fassin & Patrice Bourdelais (eds), Les constructions de l’intolérable. Études d’anthropologie et d’histoire sur les frontières de l’espace moral, Paris: La Découverte, 2005, pp. 195–224.
The movement escalated, resonating with a South African society whose capacity for mobilisation and politicisation was a legacy of the anti-apartheid struggle.
When the Cause Justifies the Alliance
In 2001, the outcome of the Pretoria Trial put an end to the South African government using the high cost of medicines as a reason for the lack of access to treatment: the pharmaceutical companies that had accused it of not complying with international rules on the protection of intellectual property dropped their lawsuit, opening the way for the use of generic medicines.
From then on it became clear that the absence of treatment in public healthcare facilities was in fact due to opposition on the part of the South African authorities themselves. President Thabo Mbeki and his health minister Dr Manto Tshabalala-Msimang, increasingly open in their support for arguments refuting the link between AIDS and HIV, had begun promoting “natural” remedies.
This policy of “denialism”A term derived from the negationism of the extermination of Jews during the Second World War. found favour among some members of South Africa’s ruling classes, seduced by the pipe dream of developing their own drug and a racial interpretation of AIDS, seeing it as a means for whites to perpetuate their domination.See Kerry Cullinan & Anso Thom (eds), The Virus, Vitamins and Vegetables: The South African Aids Mystery, South Africa: Jacana, 2009.
These were the beliefs that TAC was fighting, a battle to which MSF contributed its medical legitimacy drawn from the fast-developing project in Khayelitsha, along with its international visibility and financial support. The project introduced antiretrovirals (ARVs) in May 2001 and so, for the first time in South Africa, ARVs were accessible to AIDS patients in public health-care facilities.
Operating as an alliance was essential to the success of the fight and crucial for increasing the number of patients receiving treatment, not only for Fareed Abdullah, provincial director of the AIDS programmes in Cape Province, but also for MSF and TAC. The University of Cape Town’s School of Public Health provided the necessary scientific endorsement and became co-owner of the data produced by the project. At the time, Western Cape was the only province controlled by the political opposition to the ruling ANC, an opposition mainly constituted of white liberals from the anti-apartheid movement. There was, therefore, a real risk of the project being hijacked for political ends. Yet neither MSF nor TAC was opposed to the ANC; Fareed Abdullah was a former ANC executive and in this capacity launched the pilot project when the province was still under ANC control. So MSF played the multipartite card, allowing different political representatives to claim part of the credit. Nelson Mandela himself was of great help as, not only did he support TAC’s demands, but in 2002, while the controversy was at its height, he travelled to Khayelitsha where he visited the MSF project, openly defying the government’s policy. In 2003, MSF and the Nelson Mandela Foundation opened a joint HIV project in the rural ANC-controlled town of Lusikisiki in Eastern Cape Province.
TAC and, in particular, Zackie Achmat, using their long-standing allegiance to the ANC as an argument for opposing the government, succeeded in creating a broad social movement in support of their combat and organised numerous demonstrations, gatherings and civil disobedience campaigns—including the occupation of public buildings. Drawing on the highly progressive South African Constitution of 1996, the organisation won a number of battles, including setting up a national PMTCT programme (2001 to 2002) and a national AIDS response programme (2004). Given that the Constitution provided for a legally enforceable right to healthcare, the activists were able to use the courts as a political arena. Publically at least, MSF kept its distance from most of these battles, an attitude which its partners found difficult to understand. But TAC’s own agenda, as well as its close relations with highly politicised organisations such as the powerful trade union federation close to the ANC, COSATU, was sufficient justification for this in the eyes of the organisation. As it was, MSF was already dealing with numerous accusations of political interference. In 2002, for example, a government spokesperson described the organisation’s importing of generic antiretrovirals from Brazil as “a form of bacteriological warfare”. “ANC fears ‘bio warfare’ in Aids drug imports”, The Star, 31 Jan. 2002.
It was also accused of using the funding of TAC’s activities in Khayelitsha and Lusikisiki as a means of manipulating the movement.Interview with Eric Goemaere, Jan. 2011.
For MSF, a broad range of alliances—a classic tactic of the antiapartheid struggle—was a condition for success. At a time when the country had just rid itself of white power, MSF could hardly draw legitimacy from its identity as an organisation from the “North”. Thus, the alliances built by MSF were a means of gaining the space it needed to develop its activity and advocate for access to treatment. These alliances also became a political shield, essential for warding off attempts by the South African government to destabilise the Khayelitsha programme. Indeed, it was a patient support group that wrote to Thabo Mbeki in response to the attacks by his spokesperson,“In response to SA government’s reluctance towards Brazilian ARV drugs”, 6 Feb. 2002. publishing its letter in the press.
When the Alliance Justifies the Cause
The benefits that MSF gained from its collaboration and from the relations it developed with South African civil society encouraged it to push the experience further and, in 2007, it was decided an office would be opened in Johannesburg. This move was part of a plan by MSF Belgium to internationalise MSF, as the movement’s many centres were mostly situated in the “North” (Europe, United States and Canada). Locally, the aim was to involve South African society and, more broadly, that of the southern African sub-region, in MSF’s activities and to “continue to draw from the reservoir of ideas generated by a society mobilised to respond to public health issues”. South Africa thus became a laboratory for the organisation which went on to test “just how activist it should be”.Interview with the director of operations, MSF-Belgium, Jan. 2011.
Brussels decided to appoint a South African woman, a former anti-apartheid activist with close ties to TAC and COSATU and highly committed to social and political causes, to head its new office. Although reporting to Brussels, the office in Johannesburg was firmly anchored in the civil society from whence it came. But it had no control over MSF’s operations in South Africa, which were still directed by MSF Belgium’s head office.
Until this point, MSF’s focus in South Africa was exclusively on the response to AIDS, but this was to change considerably with the emergence of the issue of Zimbabwean migrants, which fuelled one of the organisation’s recurrent controversies: how much activism can the organisation justify in the name of its medical and humanitarian expertise? In 2006, fleeing economic hardship, repression and political violence, 1.5 to three million Zimbabweans began arriving in South Africa. Tens of thousands of them were turned back at the border whilst others settled down to a precarious existence in the country. In December 2007, MSF opened projects on the Zimbabwean border and in Johannesburg, where it provided medical consultations to between 2,000 and 3,000 Zimbabweans who had found refuge in a Methodist church and in abandoned buildings in the surrounding area.
The discussions between MSF and its partners were quickly to move beyond the strict confines of access to healthcare. This had been a legal entitlement for foreigners since 2007, although it was still constrained by fear of arrest, staff shortages and the language barrier—sometimes used as a pretext for refusing them access to medical facilities. Between 2008 and 2010, within the framework of a partnership with a number of lawyers’ organisations (notably Lawyers for Human Rights and AIDS Law Project) and the church’s Methodist priest, MSF became actively involved in the issue of migrants’ rights, with the aim of making sure their voices were heard. A project was launched with “the express purpose of bringing about political change”.Evaluation report, 2007.
The partners shared the roles between them: MSF, the constitution of medical expertise; and the lawyers the capacity to run campaigns using the informa tion supplied to them. The network, established during previous combats—including the AIDS response—was fully mobilised. Once again, the South African constitution provided the ammunition necessary for taking political contestation before the courts.
On several occasions between 2008 and 2010, MSF worked alongside its allies to promote the rights of migrants. In 2009, in response to migrants gathered around the church, some of whom were queuing up for a medical consultation, the project coordinator agreed to sign a written testimony describing the medical conditions of people under arrest to enable human rights organisations to file a complaint against the city and the police. By drawing on the South African Constitution, the organisations succeeded in putting a stop to arrests for vagrancy. This action was at its height during the xenophobic violence of May 2008 when the foreigners living in displacement camps were threatened with expulsion. MSF was denied access to the camps where its mobile teams had been providing daily consultations. The organisation issued a press release denouncing the apathy of the UNHCR and the fact that its position was founded on international conventions,“No refuge, access denied: medical and humanitarian needs of Zimbabweans in South Africa”, MSF, June 2009. whereas MSF and its allies based themselves on the South African Constitution. On each of these occasions, controversy arose within the mission, as well as between the mission, the South African office and headquarters in Brussels, on the limits to the role and responsibilities of MSF.
Translated from French by Mandy Duret
***
France. Managing the “Undesirables”
Michaël Neuman
In France, the emergence of a “new poverty” See Father Joseph Wresinski’s report to the French Economic and Social Council, Feb. 1987. led Médecins Sans Frontières to turn its attention to the country’s medical and political arenas in 1987. Developing activities such as free healthcare, dentistry and prevention of lead poisoning, MSF, “in its capacity as French doctors and as a medical organisation operating in France”, MSF-France, Board of Directors, 16 Dec. 1994. sought to alert the authorities to the shortcomings in access to healthcare for the most vulnerable of French citizens and foreign nationals. The organisation, refusing to become a substitute for the state, chose to restrict its health-care centres to a number sufficient to enable it to play the role of alerting the authorities. Various different stands were taken by MSF over time: calling for state healthcare coverage to be extended to all categories of people in 1991, denouncing the refusal to hospitalise people without state healthcare coverage in 1993, and opposing the creation of respite beds Respite beds were for the homeless, not sufficiently ill to be admitted to hospital emergency services but too ill to be admitted to emergency accommodation shelters. in 1994, which was seen as a parallel healthcare system for the poor, whereas MSF was seeking to reintegrate them into the mainstream healthcare system.
A new project was launched in 1996 “to offer advice on social services and legal support to foreign nationals living in France”. This initiative endorsed MSF’s ambition to “break with the charity role” that had characterised it from its inception, even if it meant venturing into “non medical and uncharted” territory. MSF-France, Board of Directors, 4 Oct. 1996.
It became actively involved—through legislative reform—in providing legal support to people deprived of access to healthcare, by contributing to drawing up the law on the Couverture Maladie Universelle (universal healthcare coverage, or CMU), and taking legal action to ensure application of people’s entitlement to medical aid, which led to proceedings against the Nord and the Bouches-du-Rhône local councils.

The adoption of the CMU law in July 1999 Basic universal healthcare coverage (Couverture maladie universelle-CMU) provides access to state healthcare coverage to all those legally resident in France with proof of three months of uninterrupted residence, who have no other access to state healthcare coverage. was the culmination of a programme driven by people determined to challenge public policy. Nearly four million people benefit from the CMU, which resolves the majority of problems in access to healthcare. But no sooner had the public health issue lost its urgency, than surfaced the question of the mission’s new direction. In 2001, it was noted that, “access to rights will remain an important part of MSF’s programmes in France, but [that] this issue alone can no longer justify maintaining existing programmes or opening new centres”.MSF-France, Annual Report, 2000–2001 MSF launched new initiatives, particularly in the area of accommodation, and continued to monitor application of Aide Médicale d’État (state medical aid, or AME) State medical aid has been available since the late nineteenth century under the name of Free Medical Aid (Aide médicale gratuite-AMG). Initially intended to provide free healthcare to the destitute, since the adoption of the CMU, it is now exclusively for undocumented immigrants. and the repercussions of its successive reforms. In 2003, Mission France underwent a radical overhaul, justified in part by the will to reduce the cost of projects. This development coincided with MSF scaling down its objectives to run what were known as “access to healthcare and exclusion” programmes and refocusing on operational policies targeting “direct victims of violence”, considered a priority in the allocation of resources.
Thus the projects were gradually closed down, since there was no “health emergency”MSF-France, Annual Plan, 2006. that would have justified MSF setting up medical activities. The major public health issues of the mid-1980s had mostly been resolved. The CMU and the AME, in spite of some malfunctions and the adoption of restrictive measures, played the role they were supposed to; from 1998, some 400 Permanences d’accès aux soins (healthcare access centres, or PASS) were set up in public hospitals throughout France to provide the most disadvantaged with access to healthcare. However, while MSF could have considered putting an end to its mission, the tightening of asylum policies in France and Europe and the consequences for migrants’ health justified, on the contrary, new actions. In 2006, the association set up a walk-in clinic for refugees in Sangatte in northern France, and then closed it after a healthcare access centre that it had helped to establish opened at nearby Calais hospital. MSF went on to open a “support and healthcare centre” in Paris in 2007 to provide psychological care to asylum seekers (particularly non-French speakers) suffering from psychological problems. The centre also offers social and legal advice. The organisation undertook a number of evaluations that disclosed the inadequacies in the treatment of psychological trauma, arising as much from the asylum seekers’ personal stories as from their battles with red tape.
The avowed political dimension of the project drew on the 1951 Convention relating to the status of refugees and which defines the rights of asylum seekers, particularly in terms of non-refoulement (repatriation). Its advocates saw it as raising the profile of “this humanitarian issue […] by highlighting the interaction between medical status and access to refuge”. MSF-France, Board of Directors, 15 Dec. 2006. MSF’s president opposed the project, challenging the existence of an “asylum crisis”, questioning the feasibility of the medical objectives and denouncing inconsistencies in operational decisions: accepting today what had seemingly been refused yesterday, i.e., caring for a few at a high cost—one of the reasons behind closing projects in the past.MSF-France, Board of Directors, 2006.
Others challenged MSF’s legitimacy in taking a stand on the issue of the right to asylum and, by extension, on the government’s immigration policy, exposing major divisions within the organisation on the subject.
The exchanges of views preceding the launch of the project were a presage of the difficulties to come, as they revealed the differences of opinion on MSF’s legitimacy in shifting from the humanitarian sector to the social sector. In answer to some of its members’ concerns that the organisation was engaging in a political battle too far removed from its field of expertise, those behind the project made every effort not to appear involved in a movement to oppose the government’s immigration policy.Interview with the head of mission, Nov. 2010.
Limiting confrontation with the authorities, they stepped up the number of medical consultations in order to increase legitimacy and accumulate experience and information. Medico-psychological activities provided an answer to real problems, in this case, functional disorders—even if they only helped a small number of people (900 between March 2007 and December 2010). In addition, MSF’s objective to confront the authorities was restricted by the limited scope of the medical field the organisation could draw from. A number of opportunities for challenging the authorities were seized, but without finding a more general framework to work within. The health safety net provided by the authorities rendered the project’s position particularly complex, since there is little doubt that from the perspective of the French government there was never any question of leaving undocumented immigrants to die.
As Eric Besson, then minister for immigration, said in the spring of 2009: “Humanitarian action to help foreigners in distress, regardless of their residency status, is perfectly legal”.Eric Besson’s speech in Calais, 23 Apr. 2009. http://www.immigration.gouv.fr/spip.php?page=actus&id_rubrique=254&id_ar....
In a letter to NGOs, he specified that the state, “along with local authorities, [was providing] major technical and financial support—over 20 million euros a year— to organisations providing assistance to undocumented immigrants, and their humanitarian role is vital”. http://www.la-croix.com/Actualite/S-informer/Monde/Lettre-d-associations...
The government thus applied an increasingly clear distinction between “good” humanitarian organisations, providing assistance and compassionate treatment to “superfluous” people reduced to silence, and “bad” activist and political organisations seeking to “give a voice to the excluded poor”. Didier Fassin, “Une souffrance dévoilée” in Didier Fassin, La raison humanitaire, Paris: Hautes Etudes—Gallimard-Seuil, Paris, 2010, p. 61.
So, humanitarian action was legitimate, as long as it did not lead to any criticism of public policy.See also Aurélie Windels, Eric Fassin, “Eric Besson et le délit de solidarité: La loi et la jungle”, Politis, 20 Apr. 2009.
By treating individual sufferingThe word “suffering” occurs thirty-one times in the project’s Annual Report, “Support and Healthcare Centre-Paris, 2009 Activity Report”, MSF, 2009. and not questioning the political and social origins of such suffering too closely, is MSF not confining itself to the role expected of it by the authorities: in other words, playing into their hands by looking after people rejected by the system?
Avoiding the pitfall of shared management with the authorities of those deemed “undesirable” necessarily means making good use of MSF’s role as an expert in the conflicts it believes it should legitimately be involved in. However, the extent of the health safety net in France curbs the organisation’s potential for criticism, putting it at risk of compassionate treatment of individual suffering. In autumn 2010, parliamentary and governmental offensives against the AME and the right to residency of foreign nationals in ill health did, however, give MSF new reason to take a stand in an area where it feels legitimate. These stances were justified by the role the organisation had played in setting up some of the systems, as well as concerns as to possible consequences of the reforms on people’s health.
Translated from French by Philippa Bowe-Smith
Période
Newsletter
Subscribe to our newsletter to stay informed about our latest publications. Interested in a specific author or thematic? Subscribe to our email alerts.
