
Jean-Hervé Bradol, Francisco Diaz, Marc Le Pape & Jérome Léglise

Medical doctor, specialized in tropical medicine, emergency medicine and epidemiology. In 1989 he went on mission with Médecins sans Frontières for the first time, and undertook long-term missions in Uganda, Somalia and Thailand. He returned to the Paris headquarters in 1994 as a programs director. Between 1996 and 1998, he served as the director of communications, and later as director of operations until May 2000 when he was elected president of the French section of Médecins sans Frontières. He was re-elected in May 2003 and in May 2006. From 2000 to 2008, he was a member of the International Council of MSF and a member of the Board of MSF USA. He is the co-editor of "Medical innovations in humanitarian situations" (MSF, 2009) and Humanitarian Aid, Genocide and Mass Killings: Médecins Sans Frontiéres, The Rwandan Experience, 1982–97 (Manchester University Press, 2017).

Marc Le Pape has been a researcher at the CNRS and then at the EHESS. He is currently a member of the scientific committee of the CRASH. Formerly with the CNRS, Marc Le Pape is currently a researcher at the l'Ehess (Centre d'études africaines). He has carried out research in Algeria, Côte d'Ivoire and Central Africa. His recent studies have focused on the Great Lakes region in Africa. He has co-directed several publications: Côte d'Ivoire, l'année terrible 1999-2000 (2003), Crises extrêmes (2006) et dans le cadre de MSF : Une guerre contre les civils. Réflexions sur les pratiques humanitaires au Congo-Brazzaville, 1998-2000 (2001) and Génocide et crimes de masse. L'expérience rwandaise de MSF 1982-1997 (2016).
Part 1 Symposium: Is humanitarian water safe to drink?
5th November 2010
INTRODUCTION
Francisco Diaz, Director, Logistics Department, MSF Paris
– My experience with water, hygiene and sanitation (also known as watsan) activities comes from two kinds of situations: emergencies (in Darfur, Niger, Uganda, Zambia, Eritrea, Ethiopia, Sri Lanka, and Pakistan) and access to water and sanitation for a slum population (in Guatemala City, 1987-1997).
The experience with Ethiopian Internally Displaced Persons (IDPs) camps in the 1980s was a critical one for MSF. Due to the lack of watsan expertise within the organization, we had to turn to OxfamOxfam is for Oxford Committee for Relief Famine, a charitable organization founded in Britain in 1942. and the ICRCInternational Committee of the Red Cross. to quickly acquire the know-how.
By the early 1990s, however, we were able to operate on our own in this domain. MSF’s regular involvement in assisting refugees revealed the importance of good quality water and sanitation in limiting morbidity and mortality in the camps. Watsan became MSF’s second biggest operational activity, after medical care (curative and preventive).
Physicochemical water contamination in refugee camps in Thailand and Bangladesh justified increased medical attention to the quality of the water produced and distributed in the context of humanitarian intervention. The simple fact that the prescribed procedures in our professional practice failed to take this type of contamination into consideration (Sphere,The Sphere Project was launched in 1997 with the aim of improving the quality of aid to stricken populations. Thousands of individuals from hundreds of organizations (national and international NGOs, the International Red Cross and Red Crescent Movement, United Nations institutions, donor agencies, host governments and representatives of stricken populations) representing over 80 countries have participated in various aspects of the Sphere Project (from developing and revising the Handbook through to piloting and training). 1997) led us to re-examine the origins and limits of these standards. The Logistics department wished to conduct this examination in collaboration with the CRASH team.
In my mind, the objective of this symposium is that we not resign ourselves to the recurring contamination (either fecal or physicochemical) of the water we produce and distribute, and its negative health impact, because our teams aren’t able to either prevent or treat it (for example, the hepatitis E virus).
Jean-Hervé Bradol, CRASH, MSF Paris
– The primary aim of this symposium is to better formulate the questions raised by the contamination that Francisco Diaz mentioned. That step is prerequisite to finding solutions. The day will be divided into three sessions.
In the first session, we’ll try to understand which field situations and difficulties this examination is based on. Epidemiologist Rebecca Freeman Grais, the director of Epicentre’s research department, will tell us about the summer 2004 hepatitis E outbreak at Mornay camp in Darfur. Public health engineer Étienne Gignoux, an experienced watsan manager in both the field and at headquarters, will present the main situations and difficulties that we face.
In the second session, we’ll try to get a better understanding of the current state of knowledge on the relationship between water and health, and the range of technical options for reducing waterborne health risks. Paul R. Hunter, professor of microbiology at the University of East Anglia (United Kingdom), will enlighten us about the relationship between water and health. Engineer Joël Mallevialle will give an overview of the technologies used by private and public companies, and indicate which might be compatible with the circumstances of humanitarian work.
In the third session, we’ll learn who the players are, and about the social, economic, and political issues regarding water access. We’ll also examine the nature of the discussions and conflicts at the international level. Thierry Ruf, research director at the Institut de Recherche pour le Développement (IRD), and Benoît Meribel, president of Action Contre la Faim (ACF), will present, in turn, the local and transnational issues involved in supplying water to populations. This symposium was a joint effort by people in the Logistics department (Francisco Diaz, Jérôme Leglise, Salma Lebcir, and Marianne Denolle) – where watsan activities are housed – and members of CRASH (Bérengère Cescau, Brooke Dalury, Jean-Hervé Bradol, and Marc Le Pape). I also want to thank the interpreting service (Agnès Debarge and Eve Dayre), coordinated by Caroline Lopez Serraf, and the Etat d’Urgence Production team (François Dumaine, Simon Rolin, and Jérome Etter), which videotaped the symposium.
SESSION ONE: HUMANITARIAN INTERVENTIONS WHERE THE WATER SUPPLY IS SUBJECT TO PROBLEMS
THE LESSONS LEARNED FROM HEPATITIS E EPIDEMICS
REBECCA FREEMAN GRAIS, ÉPICENTRE EPIDEMIOLOGIST & RESEARCH DIRECTOR
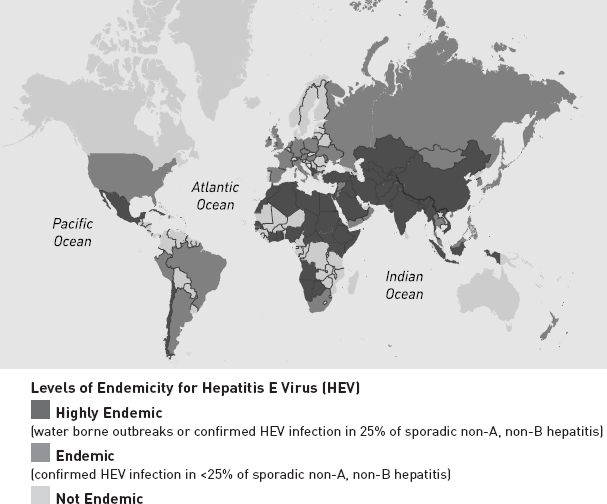
– I’m replacing our epidemiologist Kate Alberti who usually handles this topic as she is in Haiti working on the cholera outbreak. My presentation will look at the lessons we have learned from our response to hepatitis E epidemics. I’ll start with a brief description of hepatitis E and then I’ll talk about the exampleBoccia Delia, Klovstad Hilde, and Guthman Jean-Paul. Outbreak of hepatitis E Mornay Camp Western Darfur Sudan. Final report. Épicentre Dec. 2004, Paris. of Mornay camp, in west Darfur, Sudan: what we learned from that experience, what we’ve learned since, and what we still need to learn. Hepatitis E was recognized as a distinct disease only in 1980, which is relatively recent. Before then it was referred to as non-A, non-B hepatitis. A single-stranded RNA virus, the hepatitis E virus has been detected in primates and other animal species. Humans are a natural host. The primary mode of transmission is faecal and faeces contaminate drinking water. There is also person-to-person transmission and food-borne transmission (ingestion of undercooked or uncooked shellfish, for example). There is, of course, the possibility of zoonotic spread. If we look at the epidemiology of hepatitis E worldwide, all the estimates point to a fairly high level of seroprevalence. One third of the world’s population have antibodies to hepatitis E - a huge amount. A highly endemic country is one with outbreaks with a rate of infection or estimates of seroprevalence of over 25%, an endemic country has a rate of under 25%, and then in white there are the non-endemic countries. So, as you can see, HEV is everywhere.
“THE TWO FACES OF HEPATITIS E VIRUS”, JAMES M. HUGHES, MARY E. WILSON, EYASU H. TESHALE, DALE J. HU, SCOTT D. HOLMBERG, IN THE TWO FACES OF HEPATITIS E VIRUS, OXFORD UNIVERSITY PRESS, OXFORD, ROYAUME-UNI (1999) (REVUE), 2010, VOL. 51, N°3, PP. 328-334
In terms of the virus itself, there are four genotypes and one serotype. Two points of particular note, the virus is prevalent throughout the world and the genotypes are grouped geographically, with continental differences.
I will now give you an example that I know well: the outbreak that occurred in 2004 in a camp with 78,000 displaced persons in Mornay, West Darfur, Sudan. The inhabitants drew their water either from the wadi (the river), or from the pipe systems. MSF also set up a chlorinated pipe system using surface water. People were able, of course, to get their water from other sources within the camp (ground water from previously existing boreholes or untreated surface water).
So what happened? At the end of June 2004, 6 cases of acute jaundice were reported in west Darfur. The following week, 18 new cases were reported. There were 4 in Mornay, including two pregnant women who subsequently died. Cases increased in the following weeks. The Naval Medical Research Group in Cairo confirmed the diagnosis of hepatitis E. By the first week of August, there were already 1,000 cases in the whole of Darfur, with 600 in west Darfur alone, of which 200 were in Mornay. An epidemiological investigation was launched at the end of August 2004 to document the epidemic and analyse the risk factors.
We started by first examining the registers and hospitalised patients’ records and then conducted what is called a case cohort study. We looked at individuals aged 2 and over who were living in Mornay and who had had an onset of jaundice since July 1st (defined as yellow sclera) and at least one of the following symptoms: weakness, abdominal pain, fever, or vomiting. The controls, people not showing any of these symptoms, were randomly selected from among the inhabitants. Then we looked at the information we collected from these individuals (cases and controls), particularly their clinical symptoms. We performed serologic investigations for humans (IgG and IgM) and donkeys (PCR on stools and serum). We also looked at potential risk factors in the dwellings: water, sanitation, and animals in the household.
July-Dec 2004: 2621 cases
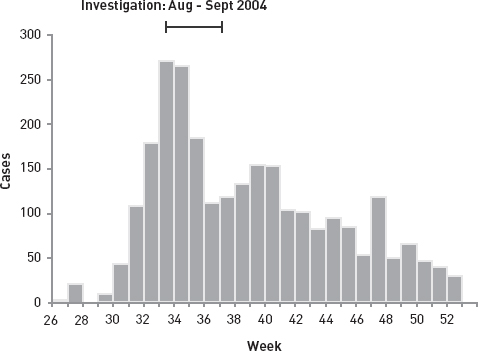
Source: Boccia Delia, Klovstad Hilde, Guthman Jean-Paul
Outbreak of hepatite E Mornay Camp Western Darfur Sudan. Final report. Épicentre, Paris, décembre 2004.
So this is what the epidemic looked like. The investigation was conducted in August. You can see that the epidemic reached a very high peak, and then fell off. This is consistent with what is called an outbreak, the origin of which is a common source, in this case, waterborne. Among the individuals we investigated, 50% of the cases were adults (aged 15 to 45), and half were female. The attack rate was around 3%. The case fatality ratio was, by and large, quite low at almost 2%, but it was significantly higher among the pregnant women (19 out of the 45 deaths).
The risk in comparison with the reference group (0 to 14 years) was approximately double for people aged between 15 and 45. We observed the commonly described risk factors but we also ascertained that drinking chlorinated surface water was also a potential risk factor. Among the 75 cases of jaundice that we tested for biological signs of hepatitis E, 97% had acute hepatitis E, and a small proportion, 3%, had prior immunity. Even more interesting, we saw that 35% of the case controls had acute hepatitis E but had no clinical symptoms. A quarter of them had an indicator of hepatitis E immunity.
Out of the 12 un-chlorinated water samples we took, 5 tested positive for coliforms. We also checked that there was correct chlorination at the taps and that the residual chlorine was in the required range. 2 out of the 5 donkeys we tested returned a positive result for hepatitis E. We only tested sick donkeys, which was probably a mistake as such a sample is clearly not representative of the donkey population.
What we learned from this investigation was, to some degree, consistent with what we already knew. The adult male population (aged 15 to 45) was at higher risk. Of course, we also saw that the pregnant women had a higher fatality rate than the other groups.
What was more surprising was that, while the analyses didn’t actually provide evidence (the confidence intervals were a little too wide), they suggested that the inhabitants who drank chlorinated surface water were at higher risk. In retrospect, these individuals may also have taken water from other sources, rather than only from the chlorinated system, or maybe it was due to another factor that we didn’t look at or that we were not able to identify. Inactivating Hepatitis E in chlorinated water requires unusually high concentrations of chlorine. But inactivating the virus may be more difficult than simply ensuring adequate chlorination. The turbidity of the water plays a role as does the pH, and it’s a difficult technique to master even under the most favourable of conditions and with a great deal of resources. The other snag is that chlorine works best at low pH and, the more chlorine added, the more it increases the pH of the water, which makes it harder to inactivate the virus. It’s a tricky undertaking, and just simply increasing chlorine is no guarantee that the hepatitis E virus will be inactivated. It is also possible that there was person-to-person transmission in the epidemic, although we didn’t look into this possibility. We only looked at the donkeys, so we have a biased sample in relation to other possible sources of contamination.
We concluded that the water distribution system did of course increase the availability and quantity of the water. But, the water treatment process that was implemented did not guarantee inactivation of the hepatitis E virus and we must adapt our water treatment processes in order to prevent future epidemics. But the essential conclusion is that it is all-important to provide water in sufficient quantities, even if it is of a quality that does not guarantee the absence of HEV.
Another issue is that the hepatitis E incubation period is extremely long - an average of 40 days. So by the time we see an increase in the number of cases, the process is very far advanced and it is too late to take action and implement changes. Our window of opportunity for intervention is very short. It should have been done when the water distribution system was first set up. So it’s a difficult disease to control once the first cases appear in a population.
Since then, we have seen another epidemic in displaced persons camps in the north of Uganda (2007-2009). Some 10,000 cases of acute jaundice were reported, and 160 deaths. Interestingly, there was a resemblance to the hepatitis genotype that we observed in Sudan and which was also present in the border regions of Chad during the same period. Our colleagues noted in Uganda that the children in the population under investigation had a higher risk of dying from hepatitis E, despite the fact that they were generally asymptomatic. These deaths were attributed to hepatitis E in verbal autopsies, which makes confirmation rather awkward. Previous studies suggest that this phenomenon had previously occurred during an epidemic in the former Soviet Union.
The main conclusion reached by the investigators and the authors when they looked at this study was that transmission within households did actually play an extremely important role. The reasons for this are unclear. There may be a sociological or demographic explanation - people who live together have a tendency to use the same water and use it in the same way because they share similar hygiene practices. They found that cases were clustered among households rather than distributed evenly across the population. What we can surmise from this is that we may have to envisage methods targeting multiple intervention locations, i.e. not merely treating the water, but targeting the users and the ways that water is used within a household.
So, what’s left to learn and what do we still need to work on? Well, when we look at the literature, we realise we don’t know that much about hepatitis E. As I saw yesterday while I was reading through the literature on the subject, almost all the authors repeat the same thing over and over again and, ironically, when you go to the WHO website for information on hepatitis E, you’ll see that the link you need to click for more information on hepatitis E does not work.
There’s nothing that really explains the differences in terms of gender or age: the impression that people aged 15 to 45 have a higher risk than others. We also don’t know much about a differential susceptibility to a fatal outcome. Why children? Why pregnant women? Both the period of communicability and the global epidemiological burden of hepatitis E have still yet to be clearly identified. Published papers provide little scientific proof and we have only patchy data from the different places around the world where there has been an increase in laboratory-confirmed cases.
We also don’t know what the role of a vaccine could be. There are several candidate vaccines being developed. Nepalese soldiers have been the targets of one vaccination campaign, and another, conducted by the Chinese government, was recently reported in The Lancet. Of course, they found 100% effectiveness among the population that they studied in a phase three trial. What’s interesting here is that more consideration should be given to vaccination and its potential use. This is a three-dose vaccine - not the easiest vaccination schedule to immunise a population. Naturally, it hasn’t been tested on pregnant women or children. We would be curious to know how well the vaccine works on the most vulnerable populations. Another aspect to investigate is the role of animal reservoirs. We know of cases in developed countries where transmission occurs from pigs, wild boar, rats, deer. A case of hepatitis E transmission from a sloth was reported recently; a low risk but this tells us once again that we don’t really understand who or what carries hepatitis E or the potential role of animal reservoirs.
I would conclude that, first of all, we need to continue to explore innovative, preventative and adaptive systems in the area of supplying water, not just with regards to hepatitis E, but in terms of public health in general. And particularly if we don’t have a completely closed system. It is important to put our minds to the measures we can put in place: verifying the quality of the water at the source, in the distribution system and of course at the point of consumption. Generally speaking, we have a relatively poor understanding of the role that water plays not only in the transmission of hepatitis E but also in the transmission of diseases in general. I sincerely hope that we will continue to investigate this further.
QUESTIONS AND COMMENTS FOLLOWING REBECCA FREEMAN GRAIS’ PRESENTATION
Fabrice Weissman, CRASH, MSF Paris
– I’d like to hear more details on the conclusions you draw from the outbreak that occurred in northern Uganda, regarding transmission modes. I didn’t really understand what you said about transmission between members of the same family.
Rebecca Freeman Grais
– They attributed the source of this epidemic, or the principal cause, to feces in the water source. But they also looked at secondary attack rates: what happened within families. Some families were essentially unaffected despite the fact that they had the same water source, versus other families where most of the family members were affected. That would lead one to believe two things: one, that there was potentially person to person transmission within the household, or there is some other factor in terms of how that water is used within the family that would have led to this clustering effect of cases, which is interesting in terms of a control measure. Meaning that it is insufficient to ignore how the water is used in a household, which is obvious.
Dominique Maison, public health engineer, WHO
– I’m a public health engineer and I deal with emergency situations at the WHO. I have one question. You quite rightly said in your presentation that water could not explain everything. I think that we very quickly get to questions of behaviors and hygiene, which are a very important aspect in this type of intervention and in the longer term. I want to know whether you conducted any KPC surveys (knowledge, practice and coverage study on water and sanitation) that might also help explain what you presented.
Rebecca Freeman Grais
– No, we haven’t although, we probably should have. I should have been more specific about that. This was actually the first big experience that we had with an outbreak of this size. I think we probably did the best we could do. Were I to do this investigation again, I would have looked at subsequent other factors as well, and that of course being one of them.
François Mansotte, public health engineer, Agence Régionale de Santé Aquitaine
– I have also worked in Guyana – the last French département (territorial division) to have a cholera outbreak (1991) and which periodically experiences localized endemic typhoid foci. I think that you stressed the fact that you were surprised to see chlorinated – correctly chlorinated – water carrying infectious agents. I’d like to say that in every country in the world, and particularly in France, chlorine inactivates neither viruses nor parasites. As a result, you really have to pay attention to the quality of the water you’re going to use, and use ground water whenever possible. This principle dates back to the 19th century, and will still hold true for centuries to come.
SUPPLYING WATER THE CONTEXTS OF MSF
PRESENTATION BY ÉTIENNE GIGNOUX, PUBLIC HEALTH ENGINEER, MSF FIELD PROJECTS
– I have experience as a watsan specialist for MSF, and since I’m the only speaker from MSF, before talking about the problems, I’ll try to tell you what we actually do in the field.
The doctors might contradict me, but a priori no one in our projects dies of thirst. But, the upheavals that lead to our interventions mean people have access to a water supply that is altered in quantity and quality. So what we to try to do is get water of sufficient quality and quantity for everyone to use.
Where does our professional culture for water come from? Usually, the people in charge of this activity at MSF are logisticians supervised by specialists who have been trained, or have acquired expertise, in water treatment and management. This expertise was acquired in a very different context – in France, for example – where the water systems have evolved layer by layer over the years. They evolved as a function of demographic growth and of scientific and technological advances. And most importantly, water in France belongs to the state, to the community. Humanitarian “super-plumbers” don’t have this kind of overall control of water in the environments they work in. Moreover, they have to act very quickly.
From a water supply standpoint, experience has taught me to divide the different contexts into four categories. Sites for refugees or those displaced by conflict are more intervention contexts of the 1990s. We were doing fewer interventions of this type by the mid-90s, although we still had a big population displacement-related emergency every year where water distribution had a major role. The latest one was in the Congo, for people displaced by conflict. They may be sporadic, but when they do occur, they require major human resources and equipment, and affect a huge amount of people. So they should not be overlooked.
The second context I want to talk about is sites for those displaced by, or victims of, a natural disaster. Why distinguish these people from those displaced by war? Mainly for technical reasons. Generally speaking, natural disasters lead to the creation of a multitude of small sites. With conflict-related population displacements, the camps are sometimes enormous – for example, the Kalma camp in Darfur has 100,000 to 120,000 people and the Mornay camp in the same region, 80,000 people. With a natural disaster, you’re going to have a few big camps, but mainly a multitude of small ones requiring a different operational approach. In addition, natural disasters often damage the water system.
The third context, after population displacements and natural disasters, consists of “stable situations” where you want to see the water supply evolve quickly – to respond to an epidemic, for example. A common example is an urban cholera epidemic. The absence of war or natural disaster is what qualifies these situations as “stable.” However, what they have in common with the response to a natural disaster is that they require interventions in multiple locations spread out over a large area.
The fourth and last context, which can’t be forgotten because it is ever present and a MSF priority, is water management in health care facilities.
As time is short, in the rest of this talk I’ll be leaving out water management in health care facilities and focus on supplying water to populations. Also due to lack of time, I won’t go into the areas of hygiene and sanitation, though these are fundamental to managing water-related health risks in care facilities.
The quality imperative is obvious for water at a clinic or a hospital. More than in other situations, the system must be reliable so that there is no interruption in supply. But roughly speaking, when it comes to supplying water, the imperatives are not very different from other contexts. In terms of sanitation and waste management, however, there are many more requirements. The quantities increase in relation to the facility’s size and activity. Cholera camps and large hospitals use a lot of water. The surgical field hospital set up in tents after the January 2010 earthquake in Haiti, used 60m3, or 60,000 liters, of water per day. Clinics, on the other hand, use a lot less – a few cubic meters a day.
To introduce our working environment to those of you who don’t know and with whom we want to share this discussion, I’ve put together a standard model of our interventions. Picture a village with an existing water resource – a well, for example. Surface water can also be collected, thanks to a river in which small holes can be dug for collecting water when the river is dry.
DRAWNING BY ÉTIENNE GIGNOUX

Two things happen when displaced people arrive. The first is reduced access to water, as there will be more people around the well; the second is pollution of both the surface and well water. This is due to the increased population and to fecal contamination. The intermixing of the resident and displaced peoples will also lead to an exchange of pathogens.
For MSF watsan technicians who intervene in response to the health crisis caused by the influx of IDPs, the priority is supplying water to health care facilities. They have several possible sources available to them. The well is already heavily used since the arrival of the IDPs. It isn’t always possible to use another source at another site – a nearby town, for example – and transport the water by tanker truck. It’s likely that as a first line, they’ll use what they have in front of them...that is, surface water.
The first goal in treating surface water is to make it clear - probably the most complicated step. But we now have sufficient experience to lay out how it should be done. Water is obtained by very quickly sinking shallow wells (surface water) in and around the river bed. We perform flocculation – sedimentation assisted by the addition of a chemical – in large tanks to get clear water.
Before the water is distributed via pipes to users, it is disinfected with chlorine. Until now, we considered chlorine sufficient. As we saw earlier, we’ve learned from experience that in some cases, chlorine doesn’t cover every epidemic risk. As a result, for some interventions we have added ultraviolet (UV) radiation treatment to the system, which is fairly easy to implement at our projects. How effective it is, however, is one of the subjects for today’s discussion.
Is surface water treatment adequate? Once the initial needs are taken care of, we can look for ground water. To better protect the resource and sometimes because of the depth required, bore wells are preferable to open wells. Why a bore well? Because it yields better bacteriological quality. We assume that the quality of ground water is better than that of surface water. Another problem with surface water is that quantities vary significantly according to the season. The volume of ground water, on the other hand, is more stable over the course of the year. But drilling a well is relatively complicated. It requires special skills and a fair amount of equipment. And there’s always a risk of not hitting water. It is, however, feasible. In most cases, the bacteriological quality of the water is better. You have to keep in mind that there are exceptions to the rule, but they are rare. In terms of physicochemical contamination, there can be nasty surprises that are hard to anticipate, a striking example is the arsenic in the ground water in Bangladesh.
So there we have, in a nutshell, the issues of supplying water in the event of a population influx. This was the first context in which MSF sought to acquire and mobilize watsan expertise. But does that expertise apply to other contexts? After Cyclone Nargis hit Burma’s Irrawaddy Delta in 2008, we were faced with a large number of sites where the water systems and reservoirs had been impacted by the disaster. So the method applied to IDP camps I mentioned earlier wasn’t feasible. Rainwater is an alternative to surface and ground water and was used at the start of Nargis relief operations. The other option is to draw water at another site and transport it by tanker trucks. This is expensive, relatively complex in terms of transport, and is vulnerable to the inevitable tanker truck breakdowns.
Aside from correcting for excess iron, physicochemical treatment is too complicated for our working environment. There are more options for bacteriological treatment. But the quantities needed for population displacements restrict us to chemically-assisted sedimentation (flocculation), chlorination, and ultraviolet radiation. We can use the same techniques for hospitals and clinics, but the smaller volumes also allow us to use more effective techniques against fecal and physicochemical contaminants, such as microfiltration, ultrafiltration, and reverse osmosis.
There is one technical area that we have yet to explore to any degree – household water treatment, at the point of consumption. There is a greater range of treatments. Chlorination and chemically-assisted sedimentation are always an option. Solar energy can be used to power UV treatment, pasteurization, or even boiling, which has been a longstanding practice among certain population groups. Microfiltration (ceramic filters) and, to a lesser extent, ultrafiltration (a jerry can fitted with an ultrafiltration membrane and a hand pump) are also among the techniques that can be used for household water treatment right at the point of consumption.
What are the current limitations of the treatments we use? One very obvious example is chlorine’s lack of effectiveness against the hepatitis E virus. We have responded by adding ultraviolet radiation to chlorination. But we have no proof that UV is effective against the hepatitis E virus, and already have reason to believe that it isn’t. The example of HEV escaping chlorination made us realize that we are not controlling the risks from a number of pathogens in the water we distribute.
During this symposium we will review the existing technologies and their possible uses in the area of humanitarian intervention. Then we need to ask ourselves, what is the right time and place for water treatment? At the source, before distributing water to the population, or at the home, before the members of the household consume it?
Access to water must be examined throughout the different stages of an emergency. Supplying water to a health care facility is often a matter of just a few hours. But providing a minimum supply of water to the population is going to take several days, or even weeks. Providing enough water for the entire population will take a few weeks, or even months. While these are systems that work, it takes several months of work to be truly effective in terms of quality and quantity. In natural disasters, and this includes epidemics – a cholera outbreak, for example – there are so many sites that all of our usual techniques reveal their limitations. This is partly due to the fact that we have trouble defining amongst a large number of possible intervention locations which sites take priority. In addition, the water supply systems that we’ve learned to set up in refugee or IDP camps require cumbersome and costly maintenance.
Such issues tip the balance in favor of household water treatment by families themselves. This might better meet the constraints posed by widely scattered sites during natural disasters and epidemics outside of camps (in “open settings”), as well as the time management issues in emergencies (distributing equipment to families can be faster than installing a collective water system). The comparative costs of the two methods – household vs. community-level treatment – may be roughly the same. But MSF has neither the equipment or the strategies for household treatment. Exploring this avenue is one of today’s objectives.
The hepatitis E experience at Mornay camp showed the limitations of our usual quality indicators: clarity, taste compatible with consumption, absence of fecal coliforms, and adequate levels of free chlorine. These are appropriate for bacterial contamination, but not for viral or parasitic contamination. The problem is the same in Europe but, as some studies have shown, the relative concentrations of virus and bacteria in the water are not the same as in the tropics.
We have tools to control the physicochemical parameters that are easy enough to use. But we still need to be informed in advance about the type of risks prevalent in the region in question. MSF teams don’t collect preliminary local and regional epidemiological data on water often enough. What’s the best approach? Should we be trying desperately to demonstrate water quality using multiple control measures? Wouldn’t it be better to get the right information regarding the available epidemiological data on the physical, chemical and infectious risks in the region?
But the connection between water and health is far from clear, and perhaps this is where I should have started my presentation. As a result, how do we know which strategy should be given preference? Should we prioritize household treatment? A collective system? Sanitation and hygiene measures? Scientists disagree. Some, like Thomas Clasen from the London School of Hygiene & Tropical Medicine, stress water’s fundamental role in health, and recommend household treatment. Others – for example, Sandy Cairncross, from the same institution – think that health depends more on hygiene and sanitation measures than on the quantity and quality of water. We’ll be coming back to this controversy over the course of the day.
QUESTIONS ON ÉTIENNE GIGNOUX’S PRESENTATION AND DISCUSSION ON BOTH OF THE FOREGOING PRESENTATIONS
– Olivier Falhun, press officer, MSF Paris
Étienne, you didn’t talk about how we handle the standard in terms of quantity. There is a standard, and a fair amount of discussion about it. I think the standard is 20 liters of water per day per person, if I’m not mistaken. Is that a goal we aim for in every situation?
– Étienne Gignoux
It’s important to provide large quantities of high quality water. So we set as our objective 20 liters of potable water per person per day. In practice, it’s always a source of discussion. We’ll see today what “potable” means in our work environment.
– Francisco Diaz
I’m in favor of running water. Water should flow from a tap whenever it’s turned on. That’s the best way to settle the quantity issue. But the environment and the context don’t always allow that. Twenty liters per person per day is still the amount we find satisfactory, if it’s achieved fairly quickly. In reality, we try to improve water production in stages, hoping to reach that threshold in a reasonable amount of time, which depends on the conditions in the refugee or IDP camp. In a hospital surgery unit, the standard is different: several hundred liters per day per patient, which has to be achieved right from the start of the intervention.
Claire Magone, CRASH, MSF Paris
– This hasn’t been well-documented, but I get the impression that MSF is doing less and less well drilling. I even have the feeling we’re not doing it at all anymore. By comparison, having seen the same intervention contexts, as in Action Contre la Faim practices, I have the feeling that MSF is less in favor of drilling than other NGOs faced with the same situations. You were talking earlier about opening a Pandora’s Box of viruses and used the example of hepatitis E. Wouldn’t that tip the balance in favor of bore wells?
Étienne Gignoux
– That’s a very good point. Ground water is indeed better in terms of bacteriological quality. It potentially solves the problem of viral contamination, if that’s a concern. This point still needs clarification, but in my opinion, it’s something we should be concerned about. Drilling wells is an alternative that helps solve the problem because we’ve seen that chlorine treatment doesn’t destroy all of the viruses in surface water. However, drilling during the initial phase, in the first week of an emergency, is really difficult. I haven’t come across many aid organizations capable of successfully drilling within such a short time frame. The conditions –geological, in particular – needed for success don’t always exist. That’s why there’s still a strong temptation to use surface water.
Jérôme Leglise, watsan advisor, MSF Paris
– After a decision by the Operations management team, it’s true that we’re not drilling wells right now. But if we found ourselves in a context where it was necessary, we would start up again. Well drilling is possible in IDP camps and in «open settings,» but only later, in the post-emergency phase. We have had a few drilling campaigns, in Thailand, in the Democratic Republic of Congo (DRC), and in Chad (2007). Since then, the activity has been put on hold. But that could change.
Gilles Roche, physician, member of the Académie de l’Eau (Water Academy)
– Speaking of standards, has MSF set out precise specifications below which you won’t distribute water?
Francisco Diaz
– Our credo is that there’s always a process for improving water quality. Take surface water, for example by definition it’s usually contaminated. Simple decanting, sedimentation with chemical additives, and exposure to sunlight should improve its quality. We usually use chlorine and chemicals to enhance the effect of sedimentation. Then, the goal is to get clear water, with low turbidity (below 5 Nephelometric Turbidity Units, or NTU), and a free residual chlorine content between 0.3 and 0.6 grams/liter. This is the objective we try to meet everywhere. But when it’s not possible, we have no choice but to distribute the water anyway.
Damien Mouly, Institut National de Veille Sanitaire (Sanitary Surveillance Institute -INVS)
– I work at the INVS, notably on water and health. In comparison with your water treatment systems, there are lots of places in France where the systems aren’t as sophisticated. Particularly with regard to pretreatment, the water is often only disinfected. So there are some methods that can be compared.
Ensuring safe water isn’t just a matter of measuring bacteriological or chemical quality, but also monitoring warning signs. Warning signs can be environmental – pluviometry, for example. Water treatment incidents are often good indicators. Many epidemics occur as a result of contamination of the resource and simultaneous failure of the treatment system. Aside from water quality monitoring, do you have a comprehensive approach that allows you to detect risks early and prevent things from getting worse?
Étienne Gignoux
– In France, ensuring water quality means making the resource secure. Establishing security perimeters, narrow or wide, to protect the source from which the water is being drawn is difficult in the settings where we work.
On the other hand, as far as water treatment incidents are concerned, they are recorded in writing and monitored, sometimes several times a day. But as you pointed out, this is a quality indicator and not an indicator that allows us to detect increased risk. Collectivized water production and distribution may make consumers less vigilant, because it’s tempting to leave responsibility to the system. Going from a collective system to family-based systems means that responsibility for water quality is transferred to the family. With household water treatment there’s a huge risk that people won’t do the necessary maintenance on their systems which means these need to be able to detect problems and interrupt production when quality is no longer assured.
To answer the question, I have a hard time imagining in the humanitarian context placing sensors all over the place to anticipate problems. But, we know that in a karsticKarst topography is a geomorphological structure resulting from the hydrochemical and hydraulic erosion of limestone formations. About one fifth of the continental area of the earth is karst terrain. Most karst is rugged terrain with a primarily subterranean water network and a substratum marked by numerous cavities; tower-like reliefs, disappearing and reappearing streams, caves and chasms. http://fr.wikipedia.org/wiki/Karst area rain is going to have an impact on water turbidity. The solution is to have a treatment system based not on one single process, but on several – for example, chlorination and UV. This could be a safeguard. When one of the two processes breaks down, the other one still ensures disinfection.
Peggy Pascal, technical advisor coordinator at Solidarités International headquarters
– I would like to go back to the question of water standards (20 liters of water per day per person), and more broadly to the Sphere project. I think that the drive for standardization was at the time aimed at pushing NGOs to homogenize their practices by defining a framework, in order to try and raise quality. But that can also be a real danger. It can lead to forgetting about the particularities of some contexts. In the case of Chad, the danger of wanting to comply with the Sphere standards is to draw too much water from fossil sources (ground water collected at a time when the region’s climate was different, and therefore not renewable). So we mustn’t forget the importance of understanding where the water comes from, because otherwise we end up with a water shortage in the camps. This is the problem we’re now facing in some camps in Chad, with horrendous long-term consequences for the local people. That’s why it’s important to spend time on the initial evaluation of available resources. Aside from its technical aspects, a bore well is also a permanent water collection point. Installing a bore well in the Sahel could lead to serious conflict over water and land ownership as there are extremely complex water and land rights. It would take NGOs years to identify and begin to be able to understand them. In northern Mali, dozens of people have died because wells were drilled in places where the importance of taking water and soil rights into account was not understood.
Francisco Diaz
– These issues are the daily reality of people in the field. What choices to make? Should we regulate the amount of water as a function of its origin, of how long the reserve will last, or should we satisfy the needs being expressed to the detriment of more long-term management of the resource? That’s why it’s important that these subjects be discussed with the beneficiaries themselves, the authorities, government representatives and aid organizations. The decisions have to be made together, so that everyone buys into them, because there won’t be a “right” choice if people act under duress. That’s more or less my perspective. We’ll talk about local social, economic and political challenges in greater detail during Thierry Ruf’s presentation this afternoon.
Paul R. Hunter, professor of microbiology, University of East Anglia, United Kingdom
– First of all, to go to the Hepatitis E issue, you said that the chart of mortality was quite high. Is that case specific mortality that was high, or was that a population based mortality?
Rebecca Freeman Grais
– In northern Uganda, one of their conclusions of their investigations was quite remarkable and possibly different than other documentations for Hepatitis E. But the problem of course, is that they assessed the mortality by verbal autopsy. So it’s a retrospective attribution of the child’s death to Hepatitis E in asymptomatic children. So I think there are potential methodological issues about attributing child’s deaths to Hepatitis E. Especially in a context where child mortality is already high. So, it would be more interesting to look at the differential between a normal expected number of deaths and an excess of deaths. In this case there were attributed to child death. But the only other point that was interesting was a precedent of high child mortality in asymptomatic children in the former Soviet Union, so there actually was another example of that.
I spoke with the people who did that study last night. They seem to have the same reaction as I did, into some degree with the Mornay example. We don’t have enough degree of understanding that we should, and so those investigations are done by the people like myself. This isn’t my expertise. So we don’t necessarily even know what to look for. And we need to work on epidemiologic methods that are more adapted to investigating water born outbreaks.
Paul R. Hunter
– Yeah, because one of the things about Hepatitis E that always strikes me, is that in many ways, with the one exception of increased mortality particularly in pregnant women, it is very like Hepatitis A; which also is very resistant to chlorine, resistant to high temperature. And causes essentially asymptomatic infection in children, and it’s only one to twenty, something that you start getting really bad illness, and that’s the group they get the sort of the full hepatic failure, which is often thing that kills with the Hepatitis A. And it’s probably due to children with not very brilliant immune systems and when your immune system is weak then it kills you.
The other issue is that we’ve been talking about water supplying in terms of is quality or quantity better? And, can we meet a normal standard? Although that debate is very interesting, I think it misses one really important thing. Whatever we do, we shouldn’t let the fact that we might not be able to achieve a predefined global standard stops us doing it. It is no way we gonna get zero pollution. We can’t achieve it and there is increasing evidence that actually, if you do start making improvements, then you can have real impacts; long before you achieve any predefined standard, which probably may or may not be true or useful in an African setting. This is something that, when I’ve been working with WHO, we’ve been very keen to trying get international guidelines policy about not waiting until you can achieve European’s standards, but actually, improving access, improving quality.
The other point is that if you are going to do anything, it has got to be sustainable. And, whatever you do, you cannot do something that has got to last 6 months, and then break down. And the problem is that many NGOs dig wells that work very well for 6 months, and then fail or fail in the dry season, when actually you need wells. In that context, you can actually make things worse, you can increase disease burden. If you want to provide easy access to water, then more and more people will perhaps choose to build their homes in an area close to water and then that fails, and suddenly you have more severe waterborne problems in an area than you had before. I think that’s something that a lot of NGOs really don’t want to know about.
Francisco Diaz
– Before turning the floor over to the other speakers, perhaps we can expand a little on the need for a water system to be stable over time in order to avoid negative impacts.
Jérôme Leglise
– I think that’s exactly one of the main purposes of today’s conference. But precisely, we operate in different situations that aren’t “long-lasting”, “normal”, “stable”, or “settled”, where we nevertheless have to find – at least in the medium term – an ideal balance between stability and durability, and quickly improving the state of affairs. Because in the initial phase of an operation, saving lives is what matters. Will the well last 6 months, a year, or even longer? For a lot of practitioners, asking themselves these types of question during an emergency makes them feel like they’re getting lost in conjecture. I completely agree on the durability issues – again, that’s the ideal.
Jean-Hervé Bradol
– In reality, in the Mornay example, the first interventions began there in 2003. The outbreak of the epidemic, if you remember Rebecca’s presentation, occurred almost a year later in late July-early August 2004. I’m raising this to question the categories with which we operate: emergency signifying short-term.
Remember too, that before the population displacement, the site had been a large market town. Wells had been drilled by Oxfam and UNICEF, as part of a development project, which told us that the water that wasn’t coming from those wells was transmitting hepatitis E – the surface water chlorinated and distributed by MSF. Remember also that we had found a Sudanese drilling company that had agreed to work in that dangerous area.
And one final factor to flesh out the context a bit – the operations teams quickly started wondering about the future of the IDP camps. Were they in the process of becoming permanent fixtures? The violence had altered the layout of the country, but that didn’t mean that this new territorial layout would disappear once the civil war ended.
Marc Laimé, journalist, Le Monde Diplomatique
– Have you thought about documenting after the fact the impact of the improvements you make? What happens afterwards, in the post-crisis situation? How long does the equipment that has been set up last? Can you evaluate the impact of emergency relief operations on the period that follows?
Second point, for today’s conference, have you been contacted or approached by the government or the French Development Agency about the 6th World Water Forum to be held in Marseille in 2012? Just taking the case of Africa, we are seeing hundreds of watsan actors there. How do you see your specific problems fitting into what was just being talked about, into the “global circus” of access to water and sanitation? Come 2012, France is going to be lecturing the whole world. For the past few months it’s been claimed that the UN adopted a universal right of access to water, which is a huge joke.
Francisco Diaz
– To answer Marc Laimé’s question, we can’t always monitor the evolution of situations in the long-term quite simply because, as emergency actors, we’ve already left by the time the durability of our installations becomes an issue. Marc’s second question was about the 6th World Water Forum in Marseille in 2012. I’d like to say that we’re outside the “global circus.” To the extent, regrettably, of not grasping the issues. To understand them better, we’ve scheduled that topic for the third session. It will be introduced by Benoît Miribel.
François Mansotte
– Étienne, I really liked that at the end of your presentation you talked about a certain type of controversy. I’m not sure there really is a controversy. There is one, provided you have different cultures. But as soon as it’s understood that the danger is contaminating the clean with the dirty, the controversy disappears. Contamination of the resource can occur in different situations. If you draw from a river that’s polluted upstream by excrement, if you work in a karstic zone or if the well isn’t protected, then of course you’ll have a sword of Damocles hanging over your head.
Then, treatment can be more or less well managed, as can transport and household water storage, which is a major issue. The last point is people’s general hygiene. Ideally, they wash their hands before eating and after defecating. There’s a kind of triangle: potable water, sanitation, and general hygiene. The triangle can be more or less in equilibrium.
You may have thought, from my earlier comments, that I have a negative opinion of MSF. On the contrary, I think that you do good work in a difficult context. Based on quality indicators on untreated water, treatment quality, storage quality, and on hygiene quality, it’s possible to characterize the situation as being relatively secure or very badly out of balance. I think that’s the fundamental question: is the system for supplying water for drinking, sanitation, and hygiene robust? Just because you intervene in the short- and medium-term, if the system is really unstable, don’t assume you’ll be spared an epidemic.
Étienne Gignoux
– I agree with you absolutely about the importance of the water-hygiene-sanitation triangle. It is indeed a whole. But let’s look again at the Mornay example, where we concluded that the outbreak was spread by the water system. In this example, we worked together with our partners on all three aspects – hygiene (Concern) and sanitation (UNICEF). Yet an epidemic spread anyway. The system was found to be at fault. It would take a huge investment to avoid that. That’s where the controversy lies. Should we focus our efforts on making a small improvement in quality, at the cost of enormous investment? In the Mornay example, drilling was the only other alternative. Drilling under those conditions is fairly complicated. Hence the controversy: is it worth it? I don’t know the answer.
Agnès Alexandre-Bird, public heath engineer, Agence Régionale de Santé (ARS) de Rhône-Alpes
– In 2004, I had to intervene at the tail end of a hepatitis E epidemic in a refugee camp in Chad. I can’t say that I ever found the causes of the epidemic. When I arrived, there were open wells that were well-managed but incorrectly chlorinated. My question concerns the effect of chlorine on viruses; you asked the question, but I hope that there will be some answers this afternoon. The documentation tells us more chlorine, higher concentration, longer contact time. I imagine this is based on scientific research. If that’s not enough, is there any information that would explain why it’s not effective?
– Joël Mallevialle, public health engineer
It always bothers me a bit when someone says, “this thing doesn’t work,” and “this other thing works.” In fact, it’s somewhere between the two, and depends on the quality of the water and the hydraulics. As for contact time, there’s something that is sometimes forgotten in French treatment plants too: the contact time isn’t calculated by dividing the volume by the flow rate. To estimate the contact time, you have to know the hydraulics in the reactor where the chlorination is being done. Otherwise, when you think you have 10 minutes of contact time, it may really be only one minute, once the hydraulics is taken into account. It’s often because of this kind of error – looking only at residual chlorine, without taking the other parameters correctly into account – that chlorination is wrongly considered to have failed. Besides, chlorine is not a cure-all. I’ll go into all this in detail in my presentation this afternoon.
Gilles Isard, MSF Head of Mission in China
– There’s one aspect we haven’t talked about, and that’s cost. Yet I have the impression that that’s a real limitation, particularly at MSF. It’s commonly assumed that supplying water should cost almost nothing. The feeling is that water-related expenses shouldn’t have a decisive influence on the operations budget. I’d like to know the cost of the technical solutions to the problem of viruses that aren’t destroyed by the usual chlorine levels – reverse osmosis, for example. How much does it cost to treat one cubic meter of water by reverse osmosis? Would increasing the budget allocated to emergency water treatment allow us to provide water in sufficient quantities and of much better quality than we do now?
We’re able to spend significant sums on medical treatment for one patient – sometimes several hundred euros a year – but you get the impression that it shouldn’t cost more than a few cents to supply a person with water. I don’t know the exact numbers. But I think that if we divide the cost of setting up and maintaining our systems by the number of people and the number of days, we’d see that the expense is tiny. I’d like your opinion on this point: isn’t the limitation more financial than technical?
Francisco Diaz
– The financial aspect may be one obstacle, but it’s not the only one. If we mobilize more financial resources, will we get better results in terms of the problems we’re looking at today? That’s an important question. But more than the financial limitations, the primarily medical nature of MSF makes water treatment a secondary objective. The fact that our colleagues from the Operations and Medical departments aren’t here today is an illustration of the problem. Gilles, what was your other question?
Gilles Isard
– If we want to treat viruses, bacteria and parasites all at the same time, reverse osmosis should be one of the possible technical solutions. How much does it cost now to treat water with reverse osmosis with the existing processes? Would it be possible to get the quantities we need? Is this approach feasible, or is it completely beyond our price range?
Francisco Diaz
– We’ll be returning to that subject this afternoon, but just to tide you over: we did a study at the time of the 2003 Liberia conflict, during a cholera outbreak in the city of Monrovia. Back then, a rather small treatment unit – with an output of 1 cubic meter per hour – cost 20,000 dollars. The unit itself – 2 to 3 cubic meters – fits on a pickup truck. Higher outputs, around of 20 cubic meters per hour, require a device nearly the size of an articulated truck. That would cost around several hundred thousand Euros.
Peter Maes, watsan, MSF Bruxelles
– The cost needs to be consistent with the scope of responsibilities. I remember problems that we had with water supply for the populations in Sudan during the nutrition crisis of 1999. I would have been very unhappy if we hadn’t managed to preposition a drilling machine even if this is costly. But something else struck me as well: the complete absence of regulation to a certain extent. For example, this Pur®, kind of wonder sachet sold by a private company. If you have turbid water, you put it inside, and normally it’s the golden bullet, at the end you have appropriate free residual chlorine. We’ve been testing that all over the world, and sometimes it works, but very often, it doesn’t work. And you find these sachets sent to all spots in the world, by containers subsidised by UNICEF and others. This is sold by Procter & Gamble®. So, there is room for some advocacy in that field and MSF is a good machine for advocacy.
Gilles Roche
– The slide animation on MSF’s strategy for water access is really good. It’s simple, clear, functional, and there’s a strategy. It’s a bit of a shame that you didn’t do a similar presentation for sanitation or even for hygiene training. As François Mansotte said, these different aspects are totally interrelated, especially in a pre-epidemic or epidemic situation. Could you say a few words about it?
Étienne Gignoux
– We are definitely in agreement on the triangle (water, hygiene, and sanitation). We’ll be talking about it a bit this afternoon, but as we had decided to focus the symposium on water, that’s what I limited my presentation to.
Dominique Maison
– To go back to the question of cost, I think it’s actually more complex, because there are a lot of externalities. You can actually spend a lot on equipment that isn’t necessarily effective on the ground. I completely agree with Peter Maes on this issue. As I see it, there is still uncertainty about what is effective and what isn’t, and about the conditions for use and implementation of these processes in humanitarian fields of intervention. For example, does the distribution of chlorine for use by families lead to people becoming dependent on it? Will the supply be regular? For how long will the process be used? How much does it cost? Take Haiti as an example. The local authorities were very clear in the first two months of the intervention that their objective regarding the sale and distribution of water in Port-au-Prince was to return to the situation of before the earthquake, even though it barely managed to meet requirements, despite the NGOs’ hard work. I think that’s an essential point for advocacy: the intervention cannot be limited to simply allocating resources on the ground and programming disengagement in a few months. We’ll have a direct impact on the situation for a few months during the emergency. But if we lower our guard, if we don’t anticipate alternative solutions and don’t plan for long-term involvement, the original problems will re-emerge. A study of the costs should include not just the initial expense, but also the potential costs – in terms of the consequences on health– of a failure, and the costs of repeated interventions due to the lack of durability of the initial system. This is an important argument when we advocate for improved water systems.
Fabrice Weissman
– I’d like to go back to the question of standards and bore wells. Echoing the comment of our colleague from Solidarités, I totally agree with the idea that standards shouldn’t be applied automatically. For example, water consumption habits in the Sahel are very different from those we see in Sri Lanka. Twenty liters of water per person per day is a lot to a nomad from Darfur. A Sri Lankan farmer, on the other hand, lives in a society sometimes characterized as a hydraulic civilization. He distinguishes between cooking water, washing water – of which he uses a great deal – and drinking water. As a result, the design of our supply system has to take these differences into account. I think we do try to pay attention, but we have to persevere to get a better understanding of the social and cultural particularities of water use. Of course, the political issues involved in creating permanent water points raise fundamental questions. Bore wells seem, a priori, one of the most accessible options for responding to the multiple problems encountered in treating surface water. I’d like to know what conclusions we can draw from the wells drilled by MSF. I’m thinking about the ones done with equipment that can be moved around on a pick-up truck, which is used a lot by Action Contre la Faim. I also have the feeling, from your description, that for a more effective well-drilling policy, it would be more appropriate to approach local companies who are already familiar with the terrain. The availability of equipment increases the speed and chances of success. What’s been the outcome of the well-drilling campaigns that MSF has done using that compact, very mobile equipment?
Étienne Gignoux
– If I gave an opinion on the outcome of our drilling campaigns, I would be both judge and jury. Ultimately, it’s better to work with local companies. The only problem is that in an emergency – particularly in our operational contexts – they don’t come. Chad is a very good example. In Dogdoré in 2007, no one wanted to come; we asked them all, but they’re not crazy. They stay at home in cases like that. And the other NGOs didn’t want to come either. The only option was to do it ourselves.
Francisco Diaz
– Access isn’t the only problem in the places where we operate. The expertise doesn’t always exist in the region in question. In the far reaches of Katanga, it’s not always that easy that to find an available and competent company to do the drilling. You always have to have several options, so that you can feel comfortable both outsourcing the activity and developing the expertise in-house.
The fundamental problem is that our operations aren’t regular enough to sustain our expertise. To maintain know-how and aggressively build on it, there needs to be a critical mass of activity, which constitutes the source of the knowledge. Plus, we have to have skilled human resources and state-of-the-art equipment – that is, suited to our specific needs. The random nature of our operations makes it very hard to guarantee that we’ll be able to respond when a new intervention is requested. And then we’re expected to be first-rate, super fast, and innovative (the trendy term), and that’s not possible without regular activity in the domain. This is our operational reality. Over the past few years our operations have become more medical. We’re working more in hospitals and in response to epidemics. Our activities in those contexts are different from supplying water to a refugee camp. So, there are the elements of our organisational problem with developing and maintaining our know-how. Now we have to find solutions.
Jean-Hervé Bradol
– I’d like to go back to the issue of standards, which seem to me to be a problem on one hand because they’re static, and on the other, because of their weaknesses. The experts tell us that dynamic risk management is the best approach. However, in our working environment the handbooks – for example, the Sphere Handbook – ask us to attain a given quantity and quality. A public health technician needs certainty. Have I done my job or not? When the quantity and quality standards are met, the public health technician and his or her supervisor often have the mistaken impression that all risk has been eliminated. This is the result of using a quality indicator, and it highlights the value of doing a risk analysis. The current standards don’t allow you to protect yourself from every possible danger. Parasites, viruses, bacteria, and toxins slip through the net. The same for chemical risks, which aren’t covered by the standards in use. The example of ground water arsenic pollution in Bangladesh is a reminder that danger remains even when the standard has been met. I share Gilles Isard’s opinion regarding a relationship between such weak standards and serious economic constraints.
Dominique Maison
– One small terminology question – the words “reference”, “values”, and “standard” are not interchangeable. Sphere sets reference values so we’re in an attitude of progress, homogeneity and improvement that corresponds to the situations we know. As for standards, they are defined by regulations in most countries. They have a prescriptive, regulatory meaning. The constraints of an emergency or ignorance of the national regulations – a poor excuse – sometimes lead to a failure to respect these standards. Organizations should at least know them, even if they aren’t able to comply with them. In theory, public authorities are capable of monitoring them and imposing sanctions. I won’t dwell on the difficulties some countries run into in this area.
In our work environment, we talk about reference values. These reference values refer to a level of risk. That’s the purpose of the consensus meetings that Professor Paul HunterSee next session. participates in, agreeing on the correct reference value, the correct indicator. Regarding Sphere reference values, comments can be addressed to Oxfam, which is currently updating the part of the handbook that interests us – water, hygiene, and sanitation. All contributions are welcome. Here’s an illustration of these regulatory problems: in Guyana, as François Mansotte mentioned, we had to deal with an emergency. An organization came in and installed a known model of clarifier,A large tank where suspended organic matter settles out. The role of the clarifier is primarily to separate the bacterial floc from the water by gravity, with the sludge settling to the bottom and the clarified water draining out peripherally. generally used by Veolia®, and began to deliver water that didn’t comply with French regulations. In emergency situations we use systems, expertise, and staff who are accustomed to making the best of the circumstances and to doing things as well as possible. But countries are more than entitled to be a lot more careful, a lot more demanding about water quality. We work independently of national standards. This is an area that merits scrutiny. Because there’s no good reason why organizations or staff from countries with high standards in the area should necessarily lower their standards on the pretext of an emergency. Regarding bacteriological quality, there are technical questions that must be raised, while keeping the cost factor in mind. As for physicochemical quality, we talked about arsenic, which represents a serious and immediate risk. But the same question applies for a whole set of other contaminants. If we can’t manage to treat them, we should at least have studied the possibility of doing so, taking cost into consideration. Some chemical risks can be left aside when the exposure time is short, around a few months. This is the case right now in Pakistan, where water resources are scarce. We have access to ground water that’s contaminated with arsenic, but poses a much lower bacteriological risk, especially cholera, than the other sources. This is tolerable, provided that exposure to the water – which doesn’t meet the WHO standard for arsenic content – is brief. This, once again, for a clearly-established health benefit for the population as a whole.
Pascal Simon
– Managing water isn’t easy for humanitarian medical organizations. To start with, it’s not our vocation. Our experience is primarily related to providing water in health care facilities. Technical solutions do exist. In the Bangladesh example, arsenic filters are available. Each country has context-appropriate technical solutions. The problem is always cost. In our budgets, there are rarely budget allocations for water in emergencies. Managing water in the medium-term is an important issue, because crises sometimes become long-term. Burmese refugees have been in camps in Thailand for thirty years. In Kalemie, on the shores of Lake Tanganyika in the Democratic Republic of Congo, there are recurring cholera outbreaks. We must ask ourselves about the future of the systems set up by aid organizations. What will happen when they leave? Will the bore wells be used? Or sold? The social and political aspect is important. For example, the Burmese refugees have better access to water than their Thai neighbors who often have to make do with five liters of water drawn from a polluted river. There can also be economic problems. In Darfur, for example, the distribution of free water to the inhabitants of Kalma camp by the aid organizations has put all the small water vendors out of work. In Haiti, supplying water is also a long-term humanitarian endeavor. Are we capable of thinking about medium- and long-term water management?
Damien Mouly
– To continue on the subject of physicochemical contaminants, I should point out that the WHO views chlorine by-products as the second most worrying problem. The more organic matter, the more there are. The more turbid the water, the more chlorine needs to be added, and the higher the levels of chlorine by-products. In short, the clearer the resource, the more effective chlorine is in controlling the risk of infection and the lower the cancer risk. The exposure time required to produce a significant cancer risk is on a different time scale than an emergency intervention.
I have one question. Epidemiology is a good tool for measuring the effectiveness of this integrated water/hygiene/sanitation approach. Epidemiological data can be collected with surveillance, surveys, and research protocols looking at more precise questions. MSF often does emergency intervention epidemiological studies. How does MSF use epidemiology to measure the health efficacy of upstream measures in the water domain?
Emmanuel Baron, Director of Epicentre
– Unfortunately, epidemiologists can’t do as much as you give them credit for. Epidemiology mainly tells us when there’s a failure. It doesn’t tell us the extent of the diseases or how they are transmitted. Rebecca Freeman Grais reviewed the survey done in Mornay in 2004 during the hepatitis E outbreak. It has serious limitations. In terms of surveillance, I don’t even know whether the teams continued to collect data for cases of febrile jaundice the following year, in 2005. Where is the information? With a little more resources and in a fairly targeted manner, we could look for the information. I’m looking forward to Professor Hunter’s presentation on the current state of knowledge regarding the relationship between water and health. There’s currently a huge vacuum in terms of information.
There’s one important number that Rebecca showed. According to the study results in our sample, a third of the general population of Mornay camp had antibodies against hepatitis E. That shows how little we know about the epidemiology of this recently discovered disease. Of course, nothing is impossible. We’re working on epidemiological surveillance, which can be supplemented with occasional surveys. We can also work on encouraging staff to recognize certain syndromes during clinical activities. But nothing can replace having the political will to take an interest in these issues, as our colleagues from the Logistics department are asking us to do. Indeed, for over 20 years now the MSF movement has had an institution called Epicentre that does epidemiology. But I’d still like to remind everyone that studies on the impact of measures implemented within large populations have limitations. If we decide to tackle these issues, we’ll look for new avenues. I’m not overly pessimistic – just cautious.
Gilles Roche
– With regard to analyzing water that’s going to be distributed, you know there are multiparametre test kits out there, and in development, that will measure heavy metals, and all kinds of toxins, bacteria, etc. They rely on the detection of a unique signal, generally photochemical. These kits or systems are simple, lightweight, and portable. My question: is MSF following this research? Are you involved in a way that lets you add your two cents, so that the systems being developed will meet your needs when they come out? I’m thinking particularly of what’s being done at the Ecole des Mines d‘Alès and at other similar institutions.
Jérôme Leglise
– We do have a kit, a spectrophotometricThe optical density of the solution is determined by a spectrophotometer calibrated to the absorption wavelength of the chemical species to be detected. measurement tool. In contrast to bacteriological quality, physicochemical quality is not monitored systematically, but rather in response to suspicions about a particular contaminant. Hence the importance of the relationship with the medical teams who tell us, according to their clinical observations, which types of poisoning they suspect – heavy metal poisoning, for example. In those cases, we send an analysis kit with a given reagent. It’s not always possible to offer a concrete solution in terms of water treatment, because as soon as physicochemical contamination is involved, it becomes extremely complex. But that would at least push us to look for an alternate resource or to draw from the least contaminated resource. MSF Logistique in Bordeaux does routine technology scouting. But we’re always open to learning about new products that other people tell us about.
Gil Dwen, watsan, MSF field projects
– I’d like to go back to the question of bore wells. Is drilling a sustainable solution, or not? Because often we install a bore well, bring a few spare parts, leave, and then come back to the field some time later to find the wells installed but not working. Similarly, when we explore new field sites we see a lot of bore wells in the same condition. They were set up, and then neither the population nor the government was able or willing to spend the money required to repair them. Has this issue been looked at? Are there answers to the problem of maintaining the wells after we leave?
Étienne Gignoux
– Are bore wells sustainable? Do you know of a water source that’s sustainable without any maintenance? Even natural sources ultimately run out when they’re used by a large number of people without being maintained. Is there any way to get water sustainably?
Gil Dwen
– We often say that bore wells are installed to provide water in the long term. I think it’s a shame to install or invest in a system like that, and not have it maintained afterward. It’s a pity that it can’t serve the population for a lot longer than the systems we usually install do at our field sites.
Francisco Diaz
– We look for ground water because a priori – and I said a priori – the quality is better. That’s what prompts us to drill – not the quest for durability. With drilling, we get better quality water so that we don’t have to treat it, because treatment is complex and not always effective. Afterward, if it’s not used and maintained, the bore well – like any building or system – deteriorates and disappears. This takes us to issues (e.g., appropriation of equipment by the people, local development) other than supplying water in an emergency.
François Mansotte
– It’s possible to exchange technical information with other institutions. I think there are at least two types of institutions. There are the ones with money – like the Veolia® and Suez®Environnement Foundations. They are experienced in taking sophisticated systems abroad. They don’t offer any guarantees in terms of sustainability, but at least they know how to install equipment quickly in a foreign country, and how to monitor water quality. Other partners are gaining in importance. For example, the French Army, which is part of NATO. Operating frequently in other countries, it has developed a structured approach. While it does take costs into account, like the other institutions, their approach relies heavily on a diagnosis of the resource. This is fundamental. I don’t think they drill wells. They treat surface water. They know the Sphere reference values. But they use something intermediate between Sphere and the WHO recommendations. What they are able to do in the field is interesting. I think sharing a professional culture would help to avoid making the same mistakes. Of course, not all organisations have the same resources, but we all have the same aim – supplying people in the short or medium term with water that is, a priori, better quality than what’s usually available. The military has an additional factor to deal with: the risk of acts of malice and attack. That risk doesn’t exist, a priori, for humanitarian organizations.
Olivier Falhun
– Just one question, out of curiosity; it might be off the subject, so I apologize in advance. We hear a lot about the impact of climate change. There are somewhat alarmist predictions about the conflicts that might be caused by the scarcity of water. Are we specifically studying these issues?
Francisco Diaz
– We’re trying to examine these issues, which aren’t as off the subject as they might seem at first glance. The Logistics department is interested in all environment-related issues. We have to set out a timetable for handling them.
Jérôme Leglise
– To add just a bit to Francisco’s answer, it’s true that we have different priorities. To use an image, we’re not among the signatories of the Grenelle Environnement [France’s Environment Round Table]. We do, however, wonder about the impact environmental changes will have on our programmes. We pay particular attention to the handling of our medical waste and other specific types of waste. We start by examining things from the bottom up, that’s the first step – to consider the impact of our activities on the environment. To continue along the thread of Étienne Gignoux’s presentation, we do know, a priori, that there are going to be more natural disasters, especially global warming-related floods. We might see a lot more of what Étienne described as the second type of intervention context: a natural disaster in an open setting over a large geographic area. These situations get us away from supplying water to IDP or refugee camps. In my opinion, that’s what we need to start preparing for, right now. That’s why the provision of potable water should play a bigger part in our future operations.
Dominique Maison
– That said, there’s good reason now to ask ourselves about the impact of relief operations on the environment. That should be done ahead of time. For example, by looking at the biodegradability of some of the products we use in our interventions. The second avenue, fairly closely linked to water, is the question of energy – its use and its sustainability, the impact of lead batteries on the environment, the possibility of using solar energy, etc. A host of topics related to this theme are open; it’s a trendy subject. While I don’t really like the term, it may offer an opportunity to get budgets, and more importantly, allow us to take advantage of the fact that the issue is at center stage right now to start a discussion. The issue is very relevant. It was mentioned earlier in connection with water supply standards. It doesn’t make sense to care about these things at home, in western countries where the resources exist, but not care once we’ve crossed the border.
Gilles Isard
– I’d like to continue discussing the water scarcity issue. Right now, we’re working in some locations where the water has to be shared at a drainage basin. Sometimes we give priority to recently arrived IDPs. Yet they are adding to an existing population, farmers, people who need those water resources and who are already having problems – seasonal, in particular – getting enough water. Sometimes, aid organizations just take over and monopolize the resource. They decide to give the water to the IDPs first, since they think they need it more than the residents. That can lead to conflicts with the local population, sometimes exacerbated by other social factors – particularly ethnic ones. I don’t know if we always take the water needs of the various users into consideration. Do we pay enough attention to that aspect? Do we reach any water sharing agreements with the local population in our programmes?
Étienne Gignoux
– I agree with the fact that we don’t always consider the local context when allocating the water. Let’s not miss the point here, though. Water is not scarce. Drinking water, domestic water, is a minute part of a population’s water requirements. Probably the smallest part, compared to the water used for irrigation or livestock. I don’t know of a situation where there wasn’t an alternative so that everyone, IDPs and residents, could get water. I don’t think global warming will affect that meager amount of domestic water. We can find solutions for that. I’m going to go back a little to the Chad example (2007). I disagree slightly. I think the amount of ground water is indeed limited. It’s true that the arrival of a displaced or refugee population can place excessive demands on the resource. However, there are ways to avoid it. The east of Chad gets as much rain as Brest in France.
Gil Dwen
– To use a concrete example, I worked in a refugee camp in Thailand. There were 8,000 refugees at the drainage basin. Water wasn’t scarce, but poorly allocated. Of course there’s water in the world, but there’s a shortage in lots of places. If everyone uses the river irrigating a valley for agriculture, the arrival of 8,000 IDPs at a small drainage basin may, if alternatives aren’t found, lead to conflict.
Francisco Diaz
– In that case, the alternative is to say that the camp isn’t in the right place. One of the essential factors to assess when setting up a camp is access to water. If it’s a problem, it means it isn’t in the right location.
Thank you all for your lively participation this morning
SESSION TWO: WATER AND HEALTH: THE CURRENT STATE OF SCIENTIFIC KNOWLEDGE AND AVAILABLE TECHNOLOGIES
WATERBORNE DISEASES AND WATER SAFETY
PRESENTATION BY PAUL R. HUNTER, PROFESSOR OF MICROBIOLOGY,
UNIVERSITY OF EAST ANGLIA, UNITED KINGDOM
First of all, thank you very much for asking me to talk today; Médecins Sans Frontières and Oxfam are my two most favourite charities in the world and so it is a great honour for me to be invited to come and talk to you today.
Just a little bit about me. I was introduced as a microbiologist, which I am, but I’m also an epidemiologist. I trained in medicine and then specialized in medical microbiology and infectious diseases. I spend most of my time now doing epidemiological research, and more particularly on diarrheal diseases. You’ve all been told about the number of deaths of children each year from diarrheal disease, but there are between 4 to 8 billion cases around the world each year and if you got all of that diarrhoea together in one place, it would be the equivalent of about 15 minutes of flow over the Niagara Falls… this comparison always goes well down with American audiences because you see all the women who were planning their honeymoons to Niagara Falls rapidly looking around for other honeymoon destinations.
And of all the diseases associated with drinking water cholera is surely the most feared, but it is childhood diarrhoeas caused by contaminated water that is almost certainly the most fatal.
So, how do we know if drinking water is safe, and if it isn’t, how do we make it safe? Well, life used to be really easy because, up until the mid-90s when I became chair of the UK advisory committee on water, all they ever talked about was how to do the best E. coli test. So in the past, if coliforms (then faecal coliforms, then thermotolerant coliforms, then E. coli, now E. coli or enterococci) were absent in 100 ml, then the water was safe and if present, the water was not. But, there are lots of problems. The first is that you do see outbreaks of disease, even in the absence of faecal indicators, notably cryptosporidium and viruses, including hepatitis E. There have been several studies and systematic reviews that actually cast doubt on the relationship between faecal indicators and disease. The other thing is that the presence of both pathogen and faecal indicators in many water systems can be intermittent, so if you’re conducting a weekly test, it isn’t really a good indication that indicators would be the same the other six days of the week. The other problem is that in many settings, particularly those where Médecins Sans Frontières works, a zero faecal indicator is in reality unachievable. There’s also a problem with E. coli in the tropics. So, in my view, no drinking water is ever safe. The drinking water in Paris is not safe. The drinking water in London is not safe. The drinking water in Darfur is certainly not safe, but, it may be safe enough. And if it isn’t, can you make it safer?
So, this is a study carried out by my colleague, Steve Gundry from Bristol University. He examined many papers on the relationship between diarrheal disease and indicator presence. And although there was a clear link with cholera, he could find no real relationship between indicators and diarrheal disease risk in the studies he looked at. So, why are we bothering? If it doesn’t matter, why don’t we try and think of doing something else? Well, I think that would be misleading, and the big issue that is often talked about and was mentioned this morning, is summed up in the paper by Tom Clasen, a lecturer at the London School of Hygiene and Tropical Medicine. He concluded that household point-of-use water treatment reduces diarrheal disease considerably, by some 30% to 40%. So a good thing, but then in 2009, his boss wrote a paper stating that his systematic examination was based on inadequate studies and that if you only looked at the double-blinded studies, the effect was not proven:Household Water poor populations: is there enough evidence for scaling up now? Schmidt, W. and Cairncross, S. (2009). Environmental science & technology; vol. 43, no. 4; pp. 986–992. “There is evidence that the estimates may be strongly biased. Current evidence does not exclude that the observed diarrhoea reductions are largely or entirely due to bias. We conclude that widespread promotion of household water treatment is premature given the available evidence.” A little aside here, you can imagine the interpersonal issues here. You’re working in a university and your boss then publishes a paper, without you knowing, that basically says the paper you published two or three years ago is rubbish… you can just imagine the difficulties.
The finishing blow was delivered by Waddington:Water, Sanitation and Hygiene Interventions to Combat Childhood Diarrhea in Developing Countries by Hugh Waddington, Lorna Fewtrell, Birte Snilstveit, and Howard White, The International Initiative for Impact Evaluation (3ie). Aug. 2009. New Delhi, India. “The results challenge the notion that water quality treatment in the household (at point-of-use) … are necessarily the most efficacious and sustainable interventions for promoting reduction of diarrhoea.”
It was not just Sandy Cairncross and Hugh Waddington who produced these kinds of reports, which were generally speaking pretty good. They concluded that the results challenged “the notion that water quality treatment at household point-of-use are necessarily the most efficacious and sustainable interventions for promoting reductions of diarrhoea.” Now, if household water treatment doesn’t work, and household water treatment works primarily, almost exclusively, by improving water quality, then the assumption must be that water quality doesn’t matter. They also looked at community-level quality interventions and found pretty much nothing there either, which was fairly disappointing. So where do we go from here?
The first thing to say… and at this point, I want to draw your attention to water safety plans. If water safety plans are a structured way of helping people to think about the water they deliver, anticipating possible problems, looking for how the system might be prone to hazards and then developing ways for going about creating systems preventing those hazards, then these are a very powerful tool.
The problem is that I have only got half an hour here, and if you are really interested in water safety plans, and I think you should be, you need to spend a whole day looking at them.
So, the issue still remains. Is water quality measurable (for example, through faecal indicators or something else) and is it important? And a lot of what I have been doing over the past few years has been trying to answer this one simple question.
This is a paper that we published in 2009.Household Water Treatment in Developing Countries: Comparing Different Intervention Types Using Meta-Regression. Hunter PR (2009), Environmental Science Technology 43: 8991–8997. We looked at the same data that Sandy Cairncross and Tom Clasen had been arguing over but we did something different. What we did was to say, ok, maybe all household water treatments are not the same because everybody else until that point had examined them together, whether it was chlorine disinfection, solar disinfection, ceramic filters, biosand water filters, or whatever.
And here is what we found: the black line is the average level you’d expect if there was no effect whatsoever, but it was subject to recall bias. So basically, if it’s above the black line, it’s not effective, and if it’s below the black line, it is effective.
ESTIMATED MEAN RISK OF ILLNESS BY INTERVENTION AND STUDY DURATION
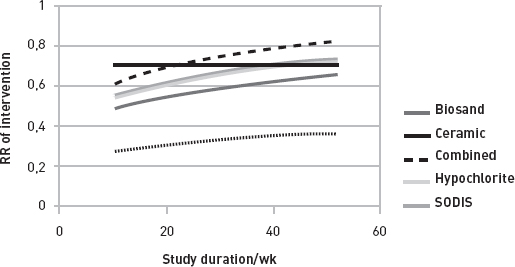
And you can see that, after the first twenty weeks or so, none of the disinfection had any value. That includes domestic chlorination, solar disinfection, a combination of chlorination and flocculation, or water filters such as PUR®. After the first twenty weeks, none of these interventions had any value.
The biosand water filter was a little bit better but not so you would really notice. But ceramic filters were substantially better than the others. And that’s consistent with Sandy Cairncross’s comments that all the blinded studies were only looking at chlorination. When they were blinded and properly conducted, there was no effect. So I would agree with Sandy that the studies cast serious doubt on household water treatment. But I would point out that the one category of intervention that does seem to work is ceramic filters. And since this paper, there have been more studies that show that ceramic filters work. There are all sorts of other publications that suggest that household chlorination doesn’t work.
So why doesn’t solar water disinfection (SODIS) work? Professor of epidemiology Dr. Jack Colford and his group at the Berkeley School of Public Health at the University of California conducted a major study in Bolivia. Two or three years later they returned to the location of a solar disinfection intervention and found that almost nobody was using it. Those who were used it only intermittently and not properly, and there was no difference in diarrheal disease. The popularity of solar disinfection is based on very mediocre studies financed by an aggressive lobby.
“What Do These Findings Mean?
These findings indicate that, despite an intensive campaign to promote SODIS, less than a third of households in the trial routinely treated their water in the recommended manner. Moreover, these findings fail to provide strong evidence of a marked reduction of the incidence of diarrhoea among children following implementation of SODIS although some aspects of the study design may have resulted in the efficacy of SODIS being underestimated. Thus, until additional studies of the effectiveness of SODIS in various real world settings have been completed, it may be unwise to extend the global promotion of SODIS for general use any further.”
Mäusezahl D, Christen A, Pacheco GD, Tellez FA, Iriarte M, et al. (2009) Solar Drinking Water Disinfection (SODIS) to Reduce Childhood Diarrhoea in Rural Bolivia: A Cluster-Randomized, Controlled Trial. PLoS Med 6(8): e1000125. doi: 10.1371/journal.pmed.1000125
Interventions on hygiene don’t work either. And that’s not to say that hygiene isn’t important; what we are saying is that if we don’t give people water, and even if we do, we’re not going to have much of an effect with hygiene measures. I’m a hospital consultant, and a large part of my career has been spent trying to persuade nurses and doctors to wash their hands properly. And if I have to fight with them, how am I going to manage to persuade farmers in Sudan to wash their hands properly… it just isn’t going to happen. There is this absolute blindness amongst the hygiene lobby to this fact… some of you people in this audience are nodding and some of you look horrified.
Sanitation works as well, and I am totally convinced of the importance of good domestic sanitation. Ceramic filters work too. Now, to get back to interventions in camps and villages, one of the reasons why some of these other disinfection techniques may not work is the impact of “bad” days.
COMPARISON OF HWT WITH OTHER INTERVENTIONS
WADDINGTON DATA
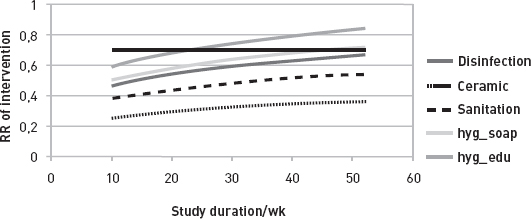
Here is a study we published several years ago where we looked at the risk in Uganda. We took the basic data from a Ugandan study. If you drank from the properly treated municipal water supply, then you had about a one in 10,000 chance of getting enterotoxogenic E. coli per year. If you drank from untreated water, then you were guaranteed a case of infection per year. You can’t get more than one because you become immune, so this was the maximum. If you drank untreated water one day in every two weeks, then you were pretty much guaranteed to become infected by the end of every year. I’ll show you some data to support this.
Impact of “bad” days
• Risk from ETEC from drinking adequately treated water
< 10-5/year
• Risk from drinking raw water
1,0/year
• Risk from drinking raw water 1 day every two weeks
0,97/year
• Risk from drinking raw water 1 day every month
0,81/year
This is the paper that was published with France’s Philippe Hartman and Denis Zmirou-Navier. You can see here, for enterotoxigenic E. coli (ETEC), one day of drinking untreated water was still 1,000 times riskier than drinking treated water for a whole 6 months.
Table 3
Probability of infection by drinking water by age when drinking treated drinking water and when drinking raw during supply failure
| Probability of infection over the whole six month period assuming fully functional water treatment | Probability of infection/d reverting to raw water consumption in each age group assuming no previous failures | |||||
| Months | ETEC | Cryptosporidium | Rotavirus | ETEC | Cryptosporidium | Rotavirus |
| 6 to 12 | 0.0003 | 0.3768 | 0.6432 | 0.1278 | 0.3706 | 0.5371 |
| 13 to 18 | 0.0003 | 0.2348 | 0.2295 | 0.1278 | 0.2309 | 0.1916 |
| 19 to 24 | 0.0003 | 0.1463 | 0.0819 | 0.1277 | 0.1439 | 0.0684 |
| 25 to 30 | 0.0003 | 0.0912 | 0.0292 | 0.1277 | 0.0897 | 0.0244 |
| 31 to 36 | 0.0003 | 0.0568 | 0.0104 | 0.1276 | 0.0559 | 0.0087 |
Probabilities for treated water over six months and for raw water over one day.
For rotavirus and cryptosporidium, it was about the same. If the treatment system fails and you have to go back to drinking raw water, the risk is pretty much the same as with the 6-month one. This is why I raised the issue of sustainability. The system has to last for more than 6 months for it to be worthwhile. This constraint also applies in an emergency situation. If you are only able to provide clean water 13 days out of 14, then all of the public health benefits of having clean water might end up in the pit latrines. I can’t stress this enough…There are so many NGOs in the field, and all they want to do is tell their donors that they have dug wells. They’re not interested in whether or not they will continue to function after they’ve gone and I think that’s extraordinarily damaging and deceitful.
The other thing we’ve been asking ourselves: maybe people haven’t been asking the right questions? Here is another study that we’ve just published in the American Journal of Tropical Hygiene. We looked at studies on the link between the distances that people go to collect water and the diarrheal disease risk. You can see here that, the further away you live, the further you have to walk to collect water, the more likely your children are to suffer from diarrhoea. This is probably an availability issue rather than a quality issue or it could be both. I think this is an area that has not really been addressed properly.
IMPACT OF DISTANCE TO STANDPIPE ON DIARRHOEA RISK
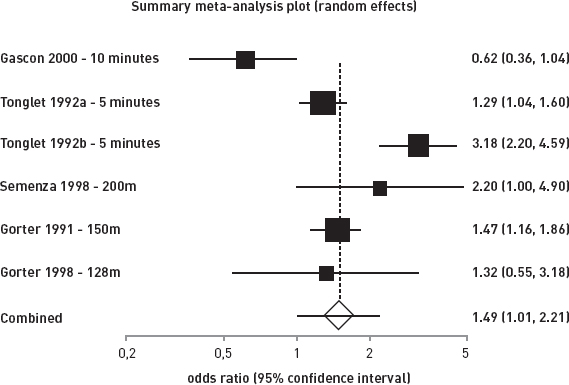
I just wanted to tell you about some studies that we’ve conducted in the ‘real’ world. The first concerns England, a well-known “developing country”, and we looked at rural communities with small water systems. You can see here that pretty much half of the sample, half of the networks, had coliforms, and about a quarter had E. coli and enterococci. Before you sit back and feel smug, oh, we’re French, we’ve got it sorted, we also looked at French networks, and you’re just as bad as we are. So, no grounds for complacency.
% Presence of indicators
| 1st sample | 2nd sample | Any sample | |
| Coliform | 36.3 | 38.1 | 47.0 |
| E. coli | 16.7 | 15.3 | 23.5 |
| Enterococci | 18.5 | 19.8 | 28.0 |
This is very disappointing: no effect. It doesn’t matter if there’s shit in your water or not. There’s no impact on diarrheal disease, alas, and in fact the impact on E. coli might even be slightly the other way around. But if you use another variable, an interaction term for age, then suddenly the results suddenly appear statistically significant. This is really important. This is your risk for diarrheal disease from drinking contaminated water. And most noteworthy is that in England all the excess disease is in children under 10. If you survive to your 10th birthday, then you’re going to be fine, and in fact you might even be slightly protected from having drunk contaminated water. It’s interesting to observe that in the over 60s group, there is a sub-group with an increased risk. These are people who retired to the country after their 60th birthday and went from drinking city water to drinking faecal polluted rural water and therefore were more at risk.
AGE SUB-GROUP ANALYSIS
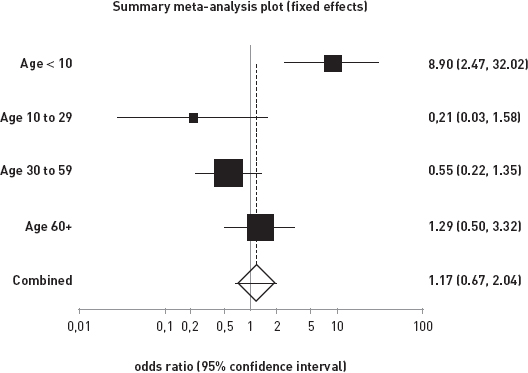
Incidence in Childreb < 10
• Enterococcus –NEGATIve
1.14 (0.46 – 2.35) episodes/person year
• Enterococcus –POSITIF
5.15 (2.57 – 9.22) episodes/person year
This is in a developed country. Moreover, if you drink this faecal polluted water in England, then you have roughly the same annualized risk of diarrheal disease as many refugee camp inhabitants. Children in many African refugee camps have diarrhoea about five times a year. And the other thing to note in this last model is the importance of good sewerage. If you have on-site sewerage, i.e. a septic tank discharging into a local stream, or some other system of disposing of it, then you are three times more likely to get diarrhoea in this model.
Now this is a study we conducted in the Mekong Delta. We found the same results. Here is the impact of improved drinking water. So if you’re under 5 and you drink improved water, then you have a quarter of the diarrheal risk compared to if you drink contaminated, unimproved water. Once you’re 5, it changes, although statistically-speaking not significantly, and then, after 5, it doesn’t matter whether you drink contaminated water or not. If we compare the diarrheal rates in Vietnam and England, you can see here, once you get to 2, the illness rates are about the same in the two countries and all the disease burden is in children aged under 2… the excess disease burden in Vietnam seems to be in children under 2.
RR in people drinking improved drinking water in Vietnam
| Age group | RR | LCI | UCI | P |
| < 5 | 0.25 | 0.07 | 0.87 | 0.03 |
| 5 to 15 | 1.75 | 0.20 | 15.1 | 0.61 |
| 16 + | 0.77 | 0.23 | 2.59 | 0.68 |
RISK OF DIARRHOEA IN TWO DEVELOPING COUNTRIES BY AGE GROUP
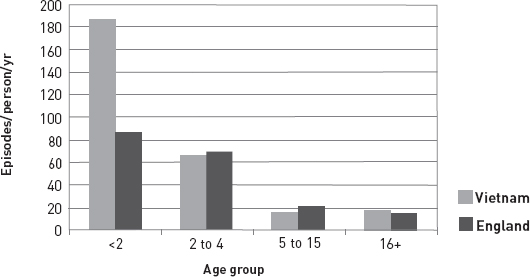
This is Puerto Rico where we’ve been doing some other intervention studies, and again, you can see that the impact of the intervention was greater on children under 5 - about twice as effective.
Puerto Rico Intervention study
| Age group | Relative risk | Lower 95% CI | Upper 05 % CI |
| < 5 years | 0.382 | 0.077 | 1.895 |
| 5 to 15 years | 0.657 | 0.228 | 1.891 |
| > 15 years | 0.687 | 0.317 | 1.483 |
This is Limpopo province in South Africa. It not as obvious in this study, but we certainly found that the value of intervention was greatest in the under 5 age group. But the interesting fact from this study, - and we think it’s accepted, it’s going to be published in the International Journal of Hygiene – brings us back to what I was saying about reliability of systems; all these results are based on the 6-month period after the intervention, but you can see here that the less reliable systems provide some improvement over the control communities, but not much, and it wasn’t statistically significant. The more reliable intervention had much more effect, so once again we have evidence. It would be better to improve the quality of the evidence. It actually does matter if you can implement a system that you are sure functions every day of every week during your stay; otherwise your efforts might be in vain.
Limpopo: new water system
| Age group | Relative risk | Lower 95% CI | Upper 05% CI |
| < 5 years | 0.361 | 0.147 | 0.889 |
| >= 5 years | 0.460 | 0.219 | 0.967 |
Impact of system reliability on illness
| Communities | Incidence/p/y |
| Control Community | 0.62 (0.48 – 0.80) |
| More reliable intervention | 0.17 (0.11 – 0.24) |
| Less reliable intervention | 0.41 (0.30 – 0.54) |
For us in this room, if we get diarrhoea (unless it’s cholera or if you’re pregnant), or hepatitis E, it’s probably no big deal. We get over it. All the deaths are in children under 5 and they’re the ones who get diarrhoea the most. Moreover, diarrhoea and malnutrition go hand in hand. And there’s quite a bit of debate in the literature about whether it’s diarrhoea that’s more important because it causes malnutrition or whether malnutrition causes diarrhoea. Whatever. All I know is that the two work together to make things worse. Particularly when HIV and malaria make their impact. You end up with more than just child deaths. To a certain extent, it’s always a tragedy for a child to die, especially for the family. But for society as a whole, maybe it’s not such a big deal because the longer-term economic fallout might not be so dramatic. I don’t actually believe what I just said there, but this is an argument that has been put forward. This has a longer-term impact on the ability of society to develop. Inability to thrive, cognitive impairment, educational underachievement, all of this is going to lead to the child failing to reach its potential as it grows up and therefore to contribute much to society by getting itself out of poverty.
The Child Death Multiplier
• Children < 5 have more diarrhoea
• A higher proportion of this diarrhoea is due to contaminated drinking water
• Children are much more likely to die from an episode of diarrhoeal disease
Now, I just want to talk to you about another aspect of water that people don’t really think about: water carrying. For those of us who have worked in Africa, one of the biding memories is that of people carrying heavy loads. I should say mainly women carry heavy loads on their heads, particularly water. We’ve just published a paper looking at water-carrying in Limpopo province as we’re particularly interested in muscular skeletal disorders. I haven’t got time to present all of the study but, basically, we found extremely high levels of self-reported back pain. Actually, this was not: “Have you got back pain?” but this was: “Tell me about water carrying, how does it impact your life?” and a frequent answer was: “ … oh God I’ve got terrible back pain, neck pain”. We’ve been measuring the loads supported by children and women’s cervical vertebrae. These are unbelievable loads that growing kids have to put up with for sometimes hours a day as they carry water backwards and forwards. So it’s not at all surprising that they get serious back pain. And we were able, even in this small pilot study, to document cases where this kind of pain subsequently leads to all sorts of other difficulties in life.
Prevalence of neck/head, back and spinal pain (n: 29)
| Frequency ratio (report of pain: pain not reported) |
Point prevalence | |
| Neck or head pain | 12:17 | 41.4% |
| Back pain | 11:18 | 37.9% |
| Spinal pain | 20:9 | 69.0% |
Dr. Santaniello-Newton used to work for MSF. I think she ran an MSF clinic in Sudan in the early 1990s. She came to work with me and we went through all the data she had from a meningitis outbreak. We were primarily interested in the effectiveness of the meningococcal vaccine as a way of controlling epidemics in refugee camps. This was the basic focus of the paper. The other interesting result we found was that the epidemic appeared to spread through the camp along the routes that people walked to collect water. There seems to be very good evidence that the people congregating around water collection points were the hub for the spread of meningococcal meningitis in this camp… in your camp.
So in conclusion, microbiological effectiveness of interventions does not necessarily correlate with public health benefits and it’s usually because the systems aren’t reliable. Believe me. For anything to work it must be reliable and taken up by the population. You’ll probably say, anybody could have come up with that, come on, tell us something exciting. But this seems to be a completely novel concept to many NGOs working in the field who seem to be not at all interested in this.
Drinking water is certainly an essential public health intervention. And I don’t care whether we’re talking about quantity or quality. Ideally we’d have both. If there’s anything you can do to improve quantity, availability, or quality, then it’s worth doing.
Reliance on E. coli testing alone is not a sufficient marker of quality and you need to be doing other things like these water safety plans. Enterococci are almost certainly a better indicator in tropical water settings than E. coli. They’re likely to be a better indicator in Europe. To be honest, they’ve always been a little bit more difficult, a little bit more expensive to do than E. coli tests. European legislation now says we have to do both.
I think the primary focus of the delivery of safe water should be families. If you can’t provide safe water to everybody, focus on families with children under 5 because this is where you will get the deaths and also where you will have the most impact on reducing longer-term health problems. Maybe when there is hepatitis E, typhoid and cholera around, then you’ve got to rethink, but even in cholera epidemics, it’s often still the under 5s that succumb most quickly.
And be careful, I’m not saying that disinfection is pointless; community-level disinfection of water systems is a good thing. I want to encourage it, although we’ve already heard about the difficulties posed by hepatitis E and cryptosporidium, probably less resistant, less sensitive to chlorine. But for people who use chlorine or PUR® sachets, or put bottles up on the roof, it probably is absolutely pointless. But not everybody will acknowledge it; there will still be those who will swear I’m Satan for even suggesting it.
I have no doubt that point-of-use ceramic filters are a sustainable and very valuable public intervention where you don’t have access to good quality water. And I would almost certainly use ceramic filters for my own water if I didn’t have access to an improved supply. And almost certainly the difference between these systems is that people use ceramic filters regularly because it actually improves the taste… it’s no longer brown, it doesn’t have grit in it and the taste is better than with chlorination or solar disinfection. With solar disinfection, water is still gritty, dirty-coloured and tastes vile. If you chlorinate it, it’s still gritty, dirty, tastes vile - especially vile because then it tastes of chlorine. I think this is a big issue, one of the main issues. There are all sorts of other problems with solar disinfection like, what do you do when the sky is cloudy? You don’t have a water treatment system then. Disinfection: what do you do when you run out of chlorine? So guys, we can’t get any chlorine until tomorrow. Never mind.
I apologize in advance to any engineers here, because I think you’re all really lovely people. But I think one of the big problems with water supply delivery in developing countries is that it has become too much of an engineering-based service, which is entirely appropriate when you’re talking about medium to large sized systems.
I think when you’re talking about small systems, one or two households, the equivalent of a well serving a few households. I think engineers still have a role. But the people that are really important here are the midwives, the nurses, the medical staff. The people who look after women who are pregnant or have recently given birth. Those of you who’ve got children, when were you or your wife most receptive to other people’s advice? Was it when she was pregnant? And most women, particularly if it’s their first delivery, are more receptive to people telling them what to do than at any other time in their lives. The problem for them is that they have the midwife, the doctor and the health visitor all saying different things.
Conclusions
– Microbiological effectiveness of interventions does not necessarily correlate with public health benefits.
– Interventions have to be reliable and taken up by the target population.
– Drinking water is certainly an essential public health intervention
– both quantity and quality.
– Reliance on E. coli testing alone is not a sufficient marker of quality.
– But it is still necessary although Enterococci may be better in the tropics.
– Primary target for delivery of safe water should be families with children <5 years old.
– However, where risk of cholera, typhoid and hepatitis E , then cannot afford to focus only on the young.
– For acute emergencies, point-of-use water treatment by whatever method probably valuable.
– After the first few weeks PoU disinfection exclusively almost certainly worthless (NB cholera).
– PoU ceramic filters definitely of value.
QUESTIONS FOR PAUL HUNTER
François Mansotte
– You brought up something very important that wasn’t mentioned at all this morning: the fact that people associate water that tastes like chlorine with the arrival of an NGO. All of a sudden, Big Brother shows up and decides for the people that the best water is water that tastes like chlorine. They’ve never drunk chlorinated water, so the chemical taste is awful. They might trust one type of water more because they’re used to drinking it, or because they can see where it’s come from, because it’s surface water and not ground water.
I was posted to the French Guyana where we distributed chlorinated water, despite the fact that people didn’t drink it. That’s an example of a technical approach we like to think we can use everywhere and make acceptable to everyone but which the local people don’t accept.
Paul R. Hunter
– I couldn’t agree more. This is certainly a big problem and it’s surprising… if you look who’s pushing which treatments around the world. Basically it’s the Americans who are pushing chlorine. If you go to New York, as soon as you turn the tap on you almost have to go and open the window and stick your head out because the chlorine smell is so strong. And Americans have grown up thinking that, and I apologize to our American colleagues here, if you can’t smell and taste chlorine, the water’s not safe because that’s what they’re used to. And all of us prefer the water we drank when we were children. If it doesn’t taste like the water you drank growing up, it doesn’t work. Largely for the reasons you mentioned, but also because it doesn’t always work anyway… it doesn’t work with hepatitis E, it doesn’t work with cryptosporidium, and it doesn’t work with some other viruses and contaminants. And that’s why I think filters may well be preferable because they improve the water. Even if you’ve grown up drinking water with dirt in it, you would actually prefer not to. It’s good to be able to close your mouth after you’ve had a glass of water without biting on grit, isn’t it? Good point.
Étienne Gignoux
– I agree that there are very interesting problems posed by household treatment and filtration. However, one of our problems is hepatitis E – a virus that concerns us directly because, in the Mornay example, the epidemiological survey showed that being a user of MSF’s chlorinated water system increased the probability of contracting the disease. Ceramic filters aren’t an answer to this problem, because the virus passes through them. This is why we researched household ultrafiltration. I know Thomas Clasen has already done a study. What do you think of this option?
Paul R. Hunter
– Yes, you’re absolutely right, ceramic filters will not remove all viruses. But they are better than many people give them credit for because the viruses don’t float around. They often stick to faecal material. When examining human diarrheal samples with an electron microscope, the viruses, and particularly the rota ones, clump with stuff. So ceramic filters reduce some of these viruses but not all of them. They cannot be relied on to remove hepatitis E. Where there is a real risk of hepatitis E, ultra-filters or reverse osmosis will certainly do the job. That’s the water I myself would drink. The problem is that they are too expensive in humanitarian settings and they also use a lot of energy. If you can afford them, then the problem will be what will happen when you move out. Suddenly you’re not there to provide further reverse osmosis or ultra-filters. And I think in the acute phase of an outbreak of hepatitis E, they are mostly definitely invaluable. But you cannot launch this type of intervention during an outbreak and then as soon as it’s over say: it’s all sorted, we’re going to pack our bags and leave. You risk making the situation worse because if you’ve been in the place for a few years, you will have prevented building immunity. If some time in the future you were to go back to the previous situation, you would find a very vulnerable population. So you need to plan for this and work out how to manage it. But yes, if you can afford it, those filters you are talking about will do the trick. Look at the army, they use these kinds of filters for their water and for a very good reason. They want their troops to be fit.
Peggy Pascal
– One comment on the subject of today’s conference, “Is humanitarian water safe to drink?” I think that depends on at what point you look at the water. When the people actually go to get it? At the tap or the water collection point? Or when they drink it? Did your study look at the issue of storage? Household storage capacity is connected with the distribution of what are called non-food items (NFI), cans in particular. My second question: what do you think about hygiene education programmes and their impact? I didn’t really understand your presentation in this regard.
Paul R. Hunter
– Ok, so the first question was essentially about household water storage. What matters is the quality of the water as it goes into the house. So in principle, as long as water is treated before it’s consumed, that’s good enough. The difficulty is that the closer you are to where the water is treated, the greater the uncertainty. If I’m the city engineer, I can control what happens to the city water network, but I will never be able to control what you do in your home. I think a lot of the failures we see in household water treatment stems from what people do in the home.
And, yes, education is indeed important. There is some evidence from South America that hasn’t yet been published that shows that if you use ceramic filters, people have to be trained on how to use them. If they aren’t, they won’t work because people do not know how to clean them and they will become contaminated. I think hygiene is very important. Thorough hand washing is absolutely essential to protect yourself and your family from disease. The problem is that we don’t yet know how to promote it other than by providing sufficient water, and soap if it’s available, so that people wash their hands. My opinion is that people who are going to wash their hands will wash them if they have access to water and soap. And if they don’t, they won’t, no matter how often you tell them it is important. And you’ve only got to take a look around here. It’s been done in the States. I’ve done it unofficially in this country, but only in gents’ toilets, not ladies’ toilets. Next time you go to a public toilet, take your time washing your hands and count the number of people who go out without washing their hands. It is depressingly high. In this country… in North America, and I have no reason to doubt it is going to be any different anywhere else in Europe. Over half of men, 60%, go into a toilet and do not wash their hands afterwards. And it’s about the same for women; I think 40% do not wash their hands. Everybody in Europe and North America knows the importance of washing their hands after they go to the toilet so why is it that so many don’t? And then people say we can reduce diarrheal disease by 40% just by telling people in the Sudan how important it is to wash our hands. It’s not going to work is it?
And when you look at the unblinded studies that have shown an effect, they cover a very short period. We have demonstrated that, whatever the method used, there are very good effects during the first few weeks. What really matters is what happens six or twelve months on. In so many of the papers on hygiene, follow-up is only for a few weeks. Go to a village this week and tell the people that it is really important that they wash their hands, here’s some soap, go back the following week and see how it went; this is not a scientific approach. In any other branch of medicine, this kind of research would be scoffed at. It wouldn’t even get published, but hygiene, household water treatment, they’ll get published. Try and explain this to the hygiene and household water treatment lobbies and they’ll draw a cross on your door and put severed horses’ heads in your bed at night!
Emmanuel Baron
– Paul, aren’t you telling us essentially that we should be paying more attention to the emergence of mass clinical phenomena, observable through the basic medical activity we practice in the field, rather than putting too much faith in monitoring biological indicators of whatever sort? In essence, isn’t it the clinician’s role that you’re emphasizing? Today’s audience is indeed telling in this respect. There’s a big imbalance between medical and nonmedical professionals – with a lot fewer of the former.
Paul R. Hunter
– Before I became a professor, I devoted most of my time managing infectious disease, at both clinical and community level, and outbreaks of epidemics. You are right. The most important thing we medics can do is, if we find as you say emerging clinical phenomena, if we are working in medicine and suddenly start seeing cases of diarrhoea in more children over 5 than we would expect, is to report it. If you’re not responsible for public health, than go and see the person who is because if you don’t keep your eye on the ball in infectious disease epidemiology, the situation can get out of hand. A classic example of this was in America. I do apologize for going on about the Americans. They’re really nice and honest people, but during the Reagan years they reduced tuberculosis prevention funding hugely with the result that, ten years later, they were suddenly having to invest huge amounts of money in tuberculosis prevention. Although I’m sure there were many other reasons, one of them HIV, there’s still the feeling that if they hadn’t taken their eye off the ball, there wouldn’t be such a problem with tuberculosis. Dengue fever is a very interesting disease and the Puerto Rican government had one of the best dengue prevention and monitoring surveillance programs in the Caribbean until about fifteen years ago. Then a surgeon was elected Governor of Puerto Rico and he decided to cut back on all public health prevention programs. So no more dengue surveillance, and last September saw an outbreak of dengue in Puerto Rico. There have been 35 deaths so far and it’s not over yet. If only they had continued with proper public health surveillance and monitoring they might not be where they are today. As medics, it’s so easy to ignore the public health implications of what we see in our clinics. But if we monitor, report and actually think about what we see and respond at an early stage, we can contain many of the problems. One of the difficulties with hepatitis E is the incubation period as, by the time you see the first case, the contamination has long gone because of the four, six, eight-week incubation period.
Peter Maes, Watsan, MSF Brussels
– I was wondering what you wanted to say with the last image in your presentation, the lady and the child in a medical setting. In a stable context, for instance in a malaria endemic zone, MSF provides a bed net to women patients coming for a prenatal consultation, and we give not one, but two bed nets to make sure that the vulnerable members of the family will sleep under one. Does this slide suggest that, in a stable setting where you have a huge burden of child mortality caused by diarrhoea, it would be relevant for MSF to provide some kind of household water treatment?
Paul R. Hunter
– Yes, if you can’t provide safe water to the whole community that is exactly what I’m suggesting. Let’s go back to the England study. We have big problems, as you do in France, with small, rural water supplies. You go to people and say: “you’ve got faeces in your water” and they say “oh I’ve been drinking it all my life, no problem, go away, Big-Brother state, forget it”. They don’t believe you. Whereas, if you say: “you’ve got faeces in your water and I know you’re used to it and you’re fine, but you could kill your grandchildren if they drink this water”, this is a much more powerful and accurate message. Messages targeting the whole population that actually only apply to children under 5 means that nobody is going to believe you. Because they know that they have been drinking the water for the past 60 years and they can’t remember the last time it made them ill. Nobody gets to 60 without ever having had diarrhoea but they are totally convinced that they haven’t. They simply won’t believe you when you tell them their water is not fit to drink. But if you make it clear that it’s not them that we’re worried about, but their children and grandchildren, they’ll listen. In situations where you can’t provide safe water for the whole community, say: “As well as giving you bed nets, we’re going to help you make water safer, here’s a ceramic filter which is easy to use. You might want to use it when you give water to your children.” Maybe pregnant women or when mothers start to dilute breast-milk with water as this is when they should start using the filter. Let’s suppose weaning occurs at six months. If you are able to get them to use one for six months from weaning until the child’s first birthday, it would be highly effective in reducing child mortality. And, given that water that has been filtered tastes better, the chances are that all the family may decide that they want to carry on filtering it because the quality of the water is so much better. That’s fine; it’s a question of quality. But it’s very young children who are the health issue.
Peter Maes
– May I anticipate the resistance that there will be to this kind of proposal? For quite a long time now people who oppose bed nets have been saying they may produce a negative mortality effect if children are protected from a very young age. But of course, even if they are protected with a bed net, they will be bitten once in a while so they will still develop immunity. Studies haven’t been able to identify this negative mortality effect in 5 to 15 or even 20 year-olds; do you think it would be same in the case of diarrhoea?
Paul R. Hunter
– It’s even more obvious in the case of diarrhoea. Aside from cholera, diarrhoea does not kill children over 5, except in extremely unusual circumstances. Anybody in this room who’s ever worked in clinical practice in developing countries will no doubt remember one or two cases of children of over 5 dying from diarrhoea. It is well documented that the probability of death falls substantially between the ages of one to five. Delaying a child from developing diarrhoea for six months substantially increases his or her chances of reaching adulthood. Unlike diarrhoea, malaria kills adults more frequently, even if the majority of deaths also occur during infancy. Of course there are always exceptions to prove the rule. We’ve all seen them. Before I became a professor, one of my last patients in clinical practice died from diarrhoea he caught from eating a Spanish lettuce contaminated with salmonella.
Étienne Gignoux
– Just one comment to follow up on Peter Maes’ question. This symposium is a start, an introduction. We’ve started working towards providing household water treatment devices. It’s good to see that others are interested. We have to try to integrate household water treatment in situations where our goal is to reduce infant and child mortality. We should take advantage of the fact that we have enough field projects to carry through these trials.
Rony Brauman, CRASH, MSF Paris
– I have a question about cholera. Is it true that lowering stomach acidity favours vibrio passage into the intestine and thus occurrence of the disease? And if that’s the case, would preventing the spread of a cholera outbreak involve a better diet to raise stomach acidity, in addition to the usual measures?
Paul R. Hunter
– You’re absolutely right. Stomach acidity matters. People suffering from a disease called achloridia, which means the stomach doesn’t produce acid, or taking antacid medications have a substantially increased risk of cholera. This is because stomach acid usually kills cholera. It’s not 100% effective because if it was, obviously ordinary people wouldn’t get the disease because the stomach acid would kill it. But it does reduce the effects substantially. I don’t know of any way of manipulating this through the food chain because cholera can be spread through food products. The recent cholera epidemic in Chile provides some evidence of this. Some street vended foods, for instance raw fish, were associated with an increased risk of cholera. On the other hand, if people drank the local coca-cola, which is acidic, they were less likely to get it than if they drank water. In fact, and nobody ever mentions this, if you drink coca- cola all the time, you won’t get cholera. I’m surprised; they’ve missed a sales argument there. Drink coca-cola and you won’t get cholera isn’t advertised on British television, but it’s absolutely true. Drinking beer probably doesn’t have the same effect but you do keep falling over!
DISINFECTION, CLARIFICATION, UV RADIATION AND ULTRAFILTRATION
PRESENTATION BY JOËL MALLEVIALLE, PUBLIC HEALTH ENGINEER
Jérôme Leglise asked me to talk about membranes and UV radiation, which are not new technologies. Their application has been growing in recent years. While I was reluctant to talk about chlorination, which is a fairly old technology, the comments I heard in this morning’s discussions justify me including it in this presentation.
Disinfection
I’d like to review a few important parameters, which people know but have a tendency to forget, both when initially sizing systems and during their operation. The most important parameters to consider are the chemical kinetics and the hydraulics of the contact reactors; the latter is frequently neglected.
Most microorganisms react according to the Chick-Watson Law, which says that microbial inactivation is directly proportional to the product of the disinfectant concentration C (in mg/l) and the contact time T (in minutes). There are, of course, exceptions. The problem is that T, the contact time, is not equal to the volume (V) divided by the flow rate (D), or V/D. To understand why, imagine that we’re in a chlorination reactorDevice in which reactions – for example, those between a disinfectant, like chlorine, and microorganisms – are contained and run. In humanitarian settings, this is often just a tank. for which T, the theoretical contact time (=V/D), is ten minutes. The water to be treated enters by one opening and leaves by another; the contact time will vary as a function of the characteristics of the path between the entrance and exit. The actual contact time, or “hydraulic retention time,” is often much shorter than that obtained from the theoretical calculation (T = V/D). It might be very far from the theoretical contact time – for example, ten minutes – and be well below one minute. The solution is to create chicanes in the disinfection reactors to get what’s called a piston effect. This happens automatically in a pipe. You have to remember that if you don’t take hydraulics into account when calculating the contact time, you don’t get the anticipated result.
The product CT – the chlorine concentration multiplied by the “hydraulic” contact time – that yields over 99% (2 log unit) microbial inactivation is an important parameter that varies widely from one microorganism to another and from one reactor to another. The CT needed to inactivate the polio virus is 300 times that needed to destroy E. coli. And the CT required to inactivate the giardiasis parasite is 9,000 times that needed to destroy E. coli. Another parasite, cryptosporidium, cannot be eliminated with chlorine, because the necessary CT is far too high. The calculation of the CT needed for a 2-log reduction in the number of microorganisms takes into account their resistance to chlorine, the chlorine concentration, and the “hydraulic” contact time. It can be used to compare the performances of different disinfection reactors, because it takes into account the contact time as a function of the specific hydraulics of the reactor, and not the theoretical contact time (V/D).
The second important parameter is the pH,The pH is one of the primary characteristics of a fluid: acid, neutral, or base. The pH ranges between 0 and 14. which gives an indication of the “degree of acidity of the water.” When dissolved in water, chlorine has two forms: ClO- and HClO. HClO is 10 to 100 times more effective than ClO-. The higher the pH, the less effective the disinfection. At pH = 8, 20% to 30% of the dissolved chlorine is in the form of HClO, while at a pH = 7, about 70% is in the form of HClO. There are places where the pH of the water is high – for example, the Tarn department in France.
Another important parameter is the ammonia content. One milligram of ammonia neutralizes 7 to 10 mg of chlorine. It varies dramatically as a function of breakdown, for example, of organic matter. If not removed, the sludge that collects in the bottom of a reactor can produce an ammonia peak during which time the water isn’t disinfected, despite the fact that the chlorine content and contact time haven’t changed.
The last important parameter is the water turbidity, i.e., the presence of organic particles. Algae that enter the chlorination reactor can shield a virus from the disinfectant, both in the reactor itself and within the distribution system.
Ozone – another, more powerful, disinfectant – isn’t used in your contexts because it doesn’t yield enough residual concentration to treat contamination that occurs subsequent to reactor disinfection, during distribution and storage. The principles are the same, however: the pH shouldn’t be too high, otherwise the ozone isn’t effective.
For reference, I should also mention silver salts, which are used in private swimming pools. I don’t have experience with silver salts, and the literature does not recommend their use in humanitarian contexts. There is, however, a consensus on the use of silver salts for preserving water in small- and large-volume bottles.
Clarification
Another water treatment process is “conventional” clarification, which I consider a disinfection process. Turbidity refers to the content of matter that makes a liquid cloudy. The WHO recommendation for water turbidity, which is measured by nephelometry using a turbidimeter, is 5 NTUs (Nephelometric Turbidimetry Units) in your work contexts.
While microbial elimination by this process is limited, it is often the first step in a series of actions (the multibarrier concept) aimed at improving water quality. Clarification helps remove a portion of the microorganisms connected to organic particles. By reducing water turbidity, clarification favors subsequent disinfectant treatment by preventing – in the case of chlorination, for example – a reduction in the concentration of free chlorine by reaction with organic matter. The figures I’m giving are for a turbidity of 0.5 NTU, which is the French standard. In your sector, the recommendation is 5 NTU. That’s understandable, because it would be hard to get 0.5 NTU everywhere. I have, however worked on small plant projects set up by NGOs where it was possible to get 0.5 NTU. It may not be possible to get it continuously, and in all circumstances, but operators should be encouraged to go below 5 NTU. The “multibarrier” concept is pertinent, and clarification is often the first of the barriers intended to remove microorganisms from water.
Radiation
Ultraviolet (UV) radiation has been in use for quite a while. UV-C is used because its wavelength corresponds to the peak absorption for proteins, DNA, RNA and all major biological substances. Radiation in the UV-A and UV-Visible portions of the spectrum is markedly less effective, though it does have some antimicrobial activity. Solar water disinfection (SODIS) relies on UV-A, because UV-B and UV-C require a quartz interface. Ordinary glass transmits very little UV-C. In other words, the SODIS process demands UV-A activity, which is much lower than that of UV-C. While UV-A does react with dissolved oxygen to form fairly reactive oxygen radicals, this happens on a small scale. Infrared radiation also heats the water, and if it reaches a temperature of 55°C, that’s not bad. But it takes six hours with 100% sun, and two days if insolation is between 50 and 100%. Solar disinfection can’t be used if it’s raining or if the water is turbid. The data in the literature aren’t very encouraging. While (SODIS) results may not be bad at first, there’s a risk that the bottles used for exposing the water to the sun, and then for storage, won’t be used properly over the long term, and that they’ll be put to other domestic uses.
Some microorganisms obey the Chick-Watson Law when exposed to UV-C radiation, but not all. The UV-C dose is generally defined in millijoules per square centimeter, which is the power of the lamp, in milliwatts per square centimeter, multiplied by the time, in seconds. Reactor hydraulics has to be taken into account when determining contact time. There are two types of lamps available. One is the low-pressure mercury-vapor lamp. In the other type, known as medium-pressure UV lamp, the mercury is either replaced or supplemented by a combination of metals. Nearly all of the energy emitted by low-pressure mercury vapor lamps is in the 250 nm, or UV-C, part of the spectrum. Low-pressure lamps have a power of 70 to 100 watts. With medium-pressure lamps, part of the emitted energy is in a different wavelength range, giving much less effective radiation. They also use a lot of energy – on the order of several kilowatts. The low-pressure lamps available on the market for water treatment have been adapted to reduce the number of lamps needed. Reactors for UV-C radiation treatment are tubular. The greater the distance from the lamp, the lower the intensity of the radiation. So you have to make sure that every part of the water receives enough radiation. The water that stays on the container surface doesn’t get much radiation. Devices that mix the water are used to remedy that.
Most microorganisms are inactivated at a dose of 40 millijoules per square centimeter. I don’t know about hepatitis E. Editor’s note: according to the recent literature, the hepatitis E virus is not destroyed at that dose. But data is scarce and not very conclusive.The spore and cyst forms of certain microorganisms are not inactivated by UV-C at that dose – Giardia and cryptosporidium, in particular.
In summary, in order for disinfectant or radiation to destroy a microorganism, it first has to cross a strip of water containing a number of elements, including both organic matter and metals such as iron. Ideally, when the UV radiation traversing the reactor vessel is too low due to an excess concentration of suspended particles, a sensor cuts off the pump. That way, distribution stops automatically when the water treatment is inadequate – for example, if there’s a spike in contamination during which water turbidity increases, causing a drop in the radiation exposure of microorganisms. According to the experts, unlike chlorination, UV radiation does not produce breakdown products. On principle, that’s hard to believe, because otherwise the radiation would have no effect on the biological matter it hits. In any case, it takes a long time for the toxic effects of disinfection byproducts to manifest themselves, while the priority of the humanitarian effort is to disinfect water right away.
UV radiation is increasingly being used in large-scale water purification plants, following sand filtration. In France, we add chlorine on discharge to obtain a concentration of 0.5 milligram per liter. Chlorine affects the taste of the water at concentrations of 0.2 milligram per liter and above.
At the household level, there are small devices with cartridge filters approaching microfiltration (5 and 25 microns), followed by a UV system, which are capable of treating 2.2 cubic meters per hour of relatively non-turbid water. The price on the internet is 520 euros with two spare cartridges and 380 euros for the radiation detector.
The same series of treatment processes (microfiltration and UV) can be used on the scale of a small village plant or neighborhood street fountain (sand filter plus UV radiation; 150-liter per hour flow rate; 70-watt solar panel; initial cost 3800 euro; estimated life span 10 years). Solar panels can supply the energy needed to produce the UV. If the water has high turbidity, low-tech clarification can be done first, for example, in a large tank that is shaken after adding coagulant, followed by rudimentary sand filtration. From what I’ve seen, as long as the device includes filtration prior to UV radiation, the results can be satisfactory. In that case, the problem of bad-tasting water from chlorine is solved.
Ultrafiltration
The initial hope with membranes was to be able to treat water without using chemical reagents. We’ll see if that’s just wishful thinking. Membranes are considered absolute filters, whose effectiveness depends on the pore size. It’s a very different philosophy or culture to sand filtration. A sand filter stops working when all the empty spaces are filled by particles; the water still flows, but there’s no more filtration. This explains why and how turbid water can come out of a sand filter. It isn’t possible with membranes, unless they break. With membrane filtration, the higher the turbidity, the lower the flow rate. Having worked with farmers, I have to say that getting them to accept the cultural change – that the flow stops when the membrane is clogged – isn’t easy.
IV – LES MEMBRANES
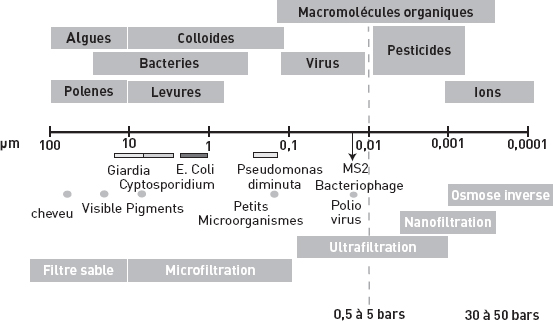
I wouldn’t think of using reverse osmosis for disinfection. An operating pressure of 30 and 50 bars is required, while ultrafiltration only needs 0.5 to 5 bars. In addition, with reverse osmosis and nanofiltration, you can’t treat the entire flow, and you remove all the mineral salts, which isn’t necessarily good for health. In the past, I’ve seen reverse osmosis units that gave worse results than microfiltration, but the technology has improved in recent years.
Now I’m going to talk to you about the fiber membranes used in ultrafiltration. There are two manufacturers in Europe: Aquasource® in France, and Norit X-Flow®, originally developed in Holland.
Water is sent through a fiber about a millimeter in diameter, for “inside-out” filtration. The pressure – 0.5 to 5 bar – allows water to diffuse through the pores. There are also membranes that operate in the opposite direction – “outside-in” – where negative pressure is needed to get the water through the pores. The advantage of these is that they are easier to clean. But the problem with “outside-in” membranes is that, because they are loose in the water, they have to be much more solid. They are more expensive to buy and have a lower flow rate.
Ultrafiltration fibers have to be stuck together, an important parameter, to form a tight seal. Modules of varying diameter can be created, depending on the desired filtration surface. For example, the filtration surface might range from 7 to 125 square meters per module. Flow rates are from 120 to 150 liters per square meter per hour. Obviously, the cleaner the water, the higher the flow rate. The membrane starts out clean, but then a cake forms and the flow rate drops. When the flow rate gets too low, the membrane has to be backwashed with clean water. After a certain number of weeks or months, chemical washing becomes necessary. Chemical washing will depend on the type of membrane. PVDF – which is a tough material, let’s say Teflon, but which fouls a lot – needs to be cleaned with acid and alkaline detergents. For cellulose triacetate, one dose of chlorine is sufficient.
The fact that high-capacity installations rely on this process is an indication that it is considered reliable.
AN 18,000- CUBIC METER PER DAY PLANT IN FRANCE.

There are simpler systems that consist of standard containers with different modules that can be installed. These systems can have 5 to 25 modules, with flow rates of 30 to 150 cubic meters per hour. One of the advantages of membranes is that they can be used to create modular systems sized for the desired flow rate.
The fibers can be made to work in two ways. Either the water is circulated – this works better, but uses energy – or you use a dead-end system, where you plug the end of the fiber and apply high pressure so that the water goes through the pores during a single pass through the ultrafiltration fiber. The results: according to the French manufacturer, ultrafiltration yields a 7-log (99.99999%) reduction in parasites and bacteria and a 6-log reduction in viruses.
In conclusion
None of the processes described in this presentation yields a perfect result, because there’s no such thing. Often, there’s no resource analysis done. In France, for example, one company installed a treatment plant downstream from a dam. It worked well. They wanted to duplicate the installation, this time with a plant upstream of the dam. During rainy periods, water turbidity created problems at the plant upstream of the dam, while obviously it wasn’t the case downstream. The upstream and downstream resources are different, and the process chosen for treating the downstream resource was overwhelmed when the rains made the upstream water more turbid.
Distribution and storage: chlorinated water is not sterile. A container of chlorinated water has 100,000, or 105, bacteria per square centimeter on the container wall. If the water is not chlorinated, there will be 100 times more, or 107, bacteria per square centimeter on the container wall.
The sustainability of the installation and the utilization procedures is a very important factor. Unfortunately, these vary so much from one installation to another that you can’t capitalize on experience, or pool equipment and personnel. I have had some experience with this with NGOs in Senegal, where the systems varied from one NGO to another. After two years, the quality was bad, due to the lack of a sustainable monitoring system.
QUESTIONS ON JOËL MALLEVIALE’S PRESENTATION
François Mansotte
– I found your presentation highly technical. Wouldn’t it be helpful to add an analysis of the types of systems available according to population size, i.e., household and collective systems? And then start discarding the treatment processes that aren’t workable, because they’re too expensive or too sophisticated, or require large amounts of energy or reagents? If we look at all the collective and individual treatment systems, which ones are left?
Joël Mallevialle
– I was asked for a relatively scientific presentation. I couldn’t look at all the prices; I don’t have them in my head. With these calculations, you have to take into account and compare the savings in work of each system. Then, depending on the output required, some may cost twice as much as others.
The small UV device I showed and gave you the price of is sold by a man who makes them in his garage. He buys parts here and there. Then he sells his device for point-of-consumption water treatment, because the water from those “water supply pigs” is bad. When I say “water supply pigs,” these refer to private outfits as well as public agencies. This size UV device works. Household ultrafiltration is growing. The problem with these devices is who does the maintenance?
François Mansotte
– I’ll make my question more precise, if you like. I’m asking about a situation that MSF often sees, a very rural setting where there may not be electricity and getting batteries poses a huge challenge.
Joël Mallevialle
– Several examples from my presentation answer the question. UV systems can be run by solar. For filtration membranes, humanitarian settings have to make do with dead-end filtration. The manufacturer says that its system uses a hundred watts per cubic meter, which isn’t a huge amount; it could be solar-powered. The hundred watts don’t include pumping to get water to the membrane or to feed the distribution network. These can also be solar-powered.
Jean-Hervé Bradol
– I believe that during the last emergency in Pakistan we tested the feasibility of using membranes at the household level - a jerrycan fitted with a hand pump that supplied enough pressure to push the water through the pores of the ultrafiltration membrane.
Étienne Gignoux
– There are new products and interesting new technologies available. We’ve already used UV in extremely resource-limited situations to bolster collective systems. We’re seeing jerrycans fitted with a membrane that can be operated by user pressure.
Jean-Hervé Bradol, CRASH, MSF Paris
– How do you clean the jerrycan membranes? Do you need ever need to use chemicals?
Étienne Gignoux
– We did the testing in our Bordeaux logistics centre and we just cleaned them with water. Backwashing was done manually in a washbasin and could be done in a streambed. But we haven’t made a final decision yet. There’s no equipment that gives as much hope of making an impact on water quality as what’s been obtained with the new ready to use products like Plumpy’Nut® in nutrition programs. Maybe we should also think about whether at MSF we have too great a tendency to want to solve every problem with a single object.
Joël Mallevialle
– In my experience, washing with water works for a while, but ultimately you need to do something else, or change the membrane. This is even truer in the case of dead-end ultrafiltration. Imagine cleaning a hollow fibre the size of thin spaghetti and with porous walls!
Étienne Gignoux
– Our equipment should last as long as the emergency, assuming that the people are going to go back to their previous situation and won’t need it. Besides, a lifespan of several years may have a health impact for small children beyond the emergency. A bit like distributing mosquito nets in an emergency or after a medical visit, we can hope for a health benefit for families who go back home with a water treatment system that lasts a year or two.
Marc Laimé
– Don’t you run the risk of yielding to – how should I say this – a fascination with high-tech? Of getting caught up in a kind of a “damn the torpedoes, full speed ahead” approach that will make it even harder when it’s time to leave the emergency area? Let’s say, – insofar as you’re able to drum up the financial and technical resources – you’re going to implement really cutting edge solutions, and when you leave, and the people have to go back to the pre-emergency situation, the gap will be even more violent, more brutal. How do you imagine you’ll deal with this kind of gap?
Joël Mallevialle
– My presentation and the modules I presented aren’t particularly intended for emergencies. I see them more as semi-permanent – that is, temporary that will last a few years. That’s not completely emergency. It’s true that ultrafiltration modules have been sent to emergencies in various places. I agree, once we leave, there’s nothing left. We can try to leave the maintenance kit, but it requires a technician capable of operating the system. The ideal is for several villages to pool their systems, which makes it a little more viable. Right now it’s considered high-tech because we’re not used to using these technologies. But the operation of both UV radiation and ultrafiltration membranes is relatively simple.
Jean-Hervé Bradol
– Marc Laimé, your question is one of the topics in the third session. In our experience, we’re often confronted with this problem. Should we or shouldn’t we achieve a certain quality threshold – for example, with medications for treating infections, and with new therapeutic pastes in nutrition? An improvement in water quality could potentially offer a measurable effect, and thus a social utility. With malaria drugs, for example, we had to go from spending a few dozen cents to several euro per treatment in order to achieve a certain efficacy threshold. And yet we were pleasantly surprised to see that failure wasn’t inevitable, since the use of the new treatments spread in a “sustainable” way, and their price dropped substantially, so that now it only costs half a euro to treat a child. Introducing a new technology always starts with an assessment of what you consider acceptable or not. How many deaths, and what kind of deaths, are acceptable in a given set of circumstances? Looked at from a different angle, how much effort and risk are involved in getting out of the situation. Any new practice always seems difficult to apply and stabilise across the board at the beginning. Initial proposals always meet with strong objections. For example, the high price – about 160 euro – of the jerrycans fitted with ultrafiltration membranes was immediately seen as an insurmountable obstacle by some of our colleagues. But by working on the price, we often manage to get it changed. For example, when we started wanting to prescribe antiretrovirals, they cost about $10,000 per patient per year. A few years later, the price was a hundredth of that. That’s the kind of impact you can get by taking a political approach to obstacles that are usually taken from just a technical perspective, without taking social and political aspects into account. We’re dealing with serious issues, for example, high mortality among young children. Governments set the objectives, in terms of mortality. We don’t come in from the outside and say what should be done. We study the country in question’s national public health plan. In addition, filtration and UV radiation are processes that already exist in the countries where we work.
Dominique Maison
– First, I’ll start by mentioning a short document by a Dutch foundation,Established jointly by the public and private sectors, the NWP Netherlands Water Partnership is an independent organization serves as a national coordination and information centre for water-related activities in the Netherlands and elsewhere. http://www.nwp.nl/afbeeldingen/WASH/Smart-DisinfectionsSolutions.pdf http://www.waterland.net/showdownload.cfm?objecttype=mark.hive.contentobjects.download.pdf&objectid=3D582856-AA1A-D55B-31D0B267A896B625 which looks at all of the most common processes. It includes not only the treatment of arsenic-contaminated water, which we talked about earlier with MDM if I remember correctly, but also information on water purification tablets. It answers François Mansotte’s question. The processes are classified according to their microbial efficacy (bacteria, viruses, and protozoa), their unit cost, and the relevant size of the population (household, village or whole region).
This little guide has one flaw, but unfortunately I haven’t seen anything better so far. It uses the manufacturers’ efficacy data. There we hit on something else that happened during the flood response operation in Pakistan in 2010. It’s a good illustration of the problem caused by the way some manufacturers behave. They turn up and sell to aid organizations in order to promote products for which there is no solid efficacy data.
In addition, I fully agree with Professor Hunter’s comment. It’s best when people take ownership of the means that will help improve their health. We have to take into account the cost of disseminating the information that’s needed in order for the population to take ownership of the new equipment. For example, in the case of the 160-euro jerrycan, don’t forget the 40 euro that may be needed for communicating with people and ensuring that they understand how the equipment works.
The way the local water supply circuit works must be taken into account to avoid prejudicing small distributors and manufacturers, like in Haiti, for example. In Port-au-Prince, water treated by reverse osmosis is being sold to the population, despite everything we just said about the technical efficacy and costs of reverse osmosis relative to its advantages.
I understand that MSF wants specifications drawn up for a specific duration and efficacy that we talked about today. But I think that that fragmenting, splitting up the discussions on the issue could result in mistakes in the field. We risk being counterproductive to the point of exposing ourselves to media criticism on contradictions between NGOs, ineffective interventions and questionable health impacts.
I too think that donors need to take responsibility for equipment used in the field, and not fund ineffective equipment that doesn’t have a health impact.
To finish, I’d like to stress the importance of the Water Safety Plan, which describes water management from resource to consumer. Obviously, the consumer has to contribute to this management.
Jérôme Leglise
– Going back to the last presentation, the problem with manufacturers’ data is indeed something we have to face. Their behaviour is sometimes unreliable. The people promoting the SODIS (solar disinfection) process claim a 100% success rate!
Sometimes there just isn’t any data, like in the case of hepatitis E. In Darfur and Chad, we set up UV systems without knowing, because there isn’t any data. Does 250-nm UV destroy the hepatitis E virus? It’s effective against the hepatitis A virus, but there’s still no answer for hepatitis E. I’d like to ask the WHO representative if it would be possible to get research laboratories working on hepatitis E, which is increasingly common especially in industrialized countries.
Alexandre Brailowsky, physician, Social Empowerment Director, Suez Environnement
– A colleague of Joël Mallevialle for a long time now, I’m a physician who has worked in industry. I’m going to ask my question, at the risk of provoking various reactions. Can all these new technologies be adapted to a humanitarian setting, to emergencies and development, which are two different scenarios? Within what moral framework might technology transfer be achieved in a field like humanitarianism?
Joël Mallevialle
– I don’t know whether I’m answering your question. I’d like to say a few things about what was said earlier. We’re pitting manufacturers against users. I’m sure that some of the results I presented were obtained by university researchers and not by manufacturers. Manufacturers aren’t concerned with doing something for humanitarianism. When a disaster strikes (the Tsunami, Haiti, etc.), manufacturers and private companies ask themselves how they can show that they’re contributing to the disaster response and so they send the equipment they have. If there were a more constructive attitude of dialogue and openness between the manufacturers and you, the users, you might even be able to cooperate on developing systems better suited to your needs. Research isn’t going to change. You might trust a university researcher who tests the modules and membranes. But equipment development and lower prices – these have to be done in consultation with one or maybe more manufacturers.
SESSION THREE: ACCESS TO WATER: SOCIOLOGICAL, ECONOMIC AND POLITICAL ASPECTS
Marc Le Pape, CRASH, MSF Paris
– Now we’re going to examine what the specialists call water governance. These governance issues will be examined on two levels – the local level, with Thierry Ruf, and the international level, with Benoît Miribel. This will be an opportunity to talk about the tensions that can arise between the different players, between experts and locally recognized authorities, between experts in the field and the international experts who set the standards, and between different categories of population.
WATER ACCESS: THE ACTORS
PRESENTATION BY THIERRY RUF, RESEARCH DIRECTOR, INSTITUT DE RECHERCHE POUR LE DÉVELOPPEMENT
Water access stakeholders: local issues
To examine water management from a social and institutional perspective, I am drawing upon my experience as an agronomist and geographer, an observer of rural agriculture and societies in the scientific tradition of comparative agriculture begun by René Dumont and carried on by Marcel Mazoyer and Marc Dufumier at the Institut National Agronomique de Paris-Grignon. This comparative approach goes beyond agricultural systems to include the sectors of potable water and humanitarian water.
I’ll begin by looking at the social management of water, and some examples that illustrate situations of conflict over resources; next I’ll relate a specific story where water can be seen as a social, economic and political issue; then I’ll discuss the possible types of relationship between stakeholders, then examples of injustice, and finally, strategies for action.
Social management of water
Generally speaking, in the rural development of countries and the small regions that comprise them, there is a stark contrast between different types of uses – in particular, between family farm management models and models using far more complicated technologies. Among the industrialized countries, the Spanish example typifies the tensions between these two models – family and corporate – and the conflicts related to resource exhaustion. There are also numerous examples among developing countries that show this. In Egypt, we observe a juxtaposition of many units all sharing the same water – the Nile – but operating according to very different sets of principles. This is seen in other examples, such as Saudi Arabia and most Near and Middle Eastern countries.
The central plains of the United States are considered the symbol of the development of what’s regarded as “water-efficient” technology. But the model is so heavily developed there that there’s talk of total exhaustion of the water table within 30 years, including drinking water resources – which is even faster than in many developing countries.
Let’s go back to the Egyptian example. Implementation of water-saving models requires major capital investment, so these technologies are for the most part beyond the reach of local communities. Poor communities find themselves having to compete for the water they have left and water becomes a source of discord. In such cases, we recommend responses that see water as a common good managed by associations. This is the thesis of winner of the 2009 Nobel Prize for Economics Elinor Ostrom, who has studied this type of society.
We also study these types of tensions, in countries like Morocco. We see situations where modernized water management ends up ignoring the ancestral rights of local and family communities and ultimately goes against their interests. The solution is to not treat the issue as simply a technical problem. Discussions must be held with the authorities, user associations and researchers. Using this method based on the sociology of collective action, we managed to prevent the tensions in a rural area of western Marrakesh from turning into a local water war.
Water as a social issue
I’m now going to relate the story of a small village in southern France, where each family had its own house and a well. One fine day, all the wells in the village dried up, because the village farmland (75% of the land) belonged to a sort of latifundista (this didn’t happen in Latin America, but it could have), who had decided to irrigate practically all his land. Of course, to irrigate he took water from the water table which lowered it, and dried up the wells of the people who, what’s more, worked for him. The villagers asked the government to help resolve the conflict.
The government took the families’ side, getting the landowner to stop using one of his wells for irrigation and reserve it for the production of drinking water. But the government asked the families to pay for the conversion; it was they who financed the entire operation. In the end, after a long struggle, they ended up with an institutional arrangement where the landowner who had over-exploited the water in the water table ultimately ended up as the private vendor of water to a community that had paid to install the infrastructure.
While the village went through all the stages of modernizing their water access network, they missed out on the cooperative stage. Rather than helping the people set up an association, the government gave the power over water back to the person who was the source of the problem.
This story is typical of what is happening in all developing countries: monopolization of agricultural water leading not only to losses for farmers (family small-holdings), but also to an extremely negative impact on drinking and domestic water, since the main visible consequences are contamination and scarcity. Then family-run agriculture is criticized for its backwardness and its organization, even though it’s not responsible for the processes that produced the effects.
In this story about a small French village coexist different definitions of water and conflict – is water a public good? Is it a common good? Is it a private good, or is it a toll good?
What matters to us, in terms of the social management of water, is to examine the notion of a common good. Elinor Ostrom set out eight principles for sustainable resource management, which can be applied to water management. First, the people have to have a reason for participating in a water treatment process and becoming involved in a water sharing process; that is, they must derive benefits from the participatory system in proportion to the costs they have to bear.
They also have to make collective choices, and I have the impression that this rule isn’t kept to as well as it should be in humanitarian interventions. There are negotiations over whether the water is going to be distributed continuously or discontinuously, in turns, etc. People have to be given some room for manoeuvre to be able to act.
Then, the principles for supervision and monitoring by the local stakeholders themselves – the water users – must be drawn up. Moreover, the concept of justice, of a water court, is a very important part of this approach. There are incidents, accidents, and theft, with penalties for those who fail to obey the rules.
But rules aren’t enough, they need to be applied, so there must be local authorities to ensure their application, who, in turn, must have government recognition – this is especially true for agriculture, but is also valid for domestic and drinking water as well.
What we find, at the local level, is that modern laws are never truly the absolute reference point; local water institutions are created from learning, from trial and error, and often a very rich history. This is a problem when NGOs intervene in an emergency situation, because they don’t know the history of where they are working. Perhaps NGOs should quickly call in an “operational sociologist” – I don’t know if that’s what he or she should be called – but someone to define the context and identify potential issues.
The tensions experienced by local institutions usually stem from several processes. On one hand, there’s the long history of political intrigue, territorial control, power struggles, and social transformations. But there are also contemporary divergences of interest among the local society, which is never homogeneous so there are very stark distinctions. Thus, often agreements that were once acceptable and appropriate may no longer be so at the time of the intervention.
We also have to acknowledge the difficulty of organizing a dialogue between all of the private, public and community stakeholders. Such is the case, for example, when the political power claims control of water and presents state water ownership as a necessity, while recognizing the principle of subsidiarity, by which water is managed locally. You can see right away that knowing which stakeholder has the most legitimacy in allocating water won’t be easy – is it the state, the community or the local water authority?
Balances are, however, struck between these different entities. These balances are established in a variety of ways; water resource management may be perceived as an area in which local communities, government agencies and private stakeholders will cooperate. This is not evident since, on the one hand, rural communities are not homogeneous, and on the other, the public interest is confronted with political patronage and corruption, while the private players are also highly heterogeneous, due to different and diverging viewpoints and stakes.
There are several arrangements possible. There is, for example, the École Française de l’Eau-type balance, where the state views itself as the owner of the resources, and appoints a private entity which signs a contract with a client. There is also the centralized state management, an approach once very common in many high- and low-income countries, though not the most in vogue today.
In reality, water management is always very complicated. I’m going to add one more complication, arising from the fact that there are always inconsistencies between administrative territories for water – inconsistencies between the authority exerted at a provincial or government level or at a drainage basin or actual water use zone; and inconsistencies between the authority over ground water, a basin, a usage zone. This is one of the major challenges. People talk about infrastructure, but they’re not talking about the same thing, or the same territory, or the same zones, or the same networks.
Possible types of stakeholder relationships
Let’s try to model the relationships between different stakeholders. Often, when dealing with resources, we talk about planning and privatization. We pit private and government sectors against each other, forgetting that the political equilibrium depends anyway on urban and rural communities. In general, people want neither total submission to the state, nor total dependence on privatization; as a result, a sort of balance is established. What we think less about is the relationship between democracy and populism, between the State and citizens. The balance between the central authority and the implementation of local control also has to be managed. Then the influence exerted by the various economic sectors needs to be taken into account; these want neither total dependence on the government, nor a market totally fragmented into local principalities or fiefdoms. There are also public agencies looking to strike a balance by applying a regulatory political model and a precautionary social model. In fact, the management of a resource like water should be a kind of complex social compromise, where all of these forces (populism, democracy, paternalism, privatization and planning) find a balance around the values of equity, regulation and efficiency. Yet we find that in agriculture (this may also apply to humanitarian water governance), the intervention models are generally very far from such a compromise; the models are either highly interventionist, or populist, or committed to privatization and the efficiency of the market as a producer of equilibrium (the case of the models advocated by the World Bank and the IMF). As for the populist model, it tends to overestimate local organizational capacities in its assumption that water can only be managed at the very local level, with no coordination, no public regulation, and no attempt at economic efficiency.
The approach we propose aims simply at getting the stakeholders to cooperate with each other and discuss the technical, social, and institutional issues, to find a balance where no one party is dominant – the state doesn’t dominate the local level, and the local level doesn’t dominate the state agent or the private sector. There needs to be some sort of forum for discussing and negotiating problems.
Let’s further complicate things. Obviously, this summary is simple compared to the reality everyone experiences when they work in developing or industrialized countries. At every level – local communities, the State, the private sector – there are disagreements among stakeholders, a lack of a common vision, and resistance to compromise. The world of water is a world that pits coalitions – each made up of elements from the rural community, the State, and the private sector – against each other.
Injustice
Here is another account, about a research and exchange program between academics, State representatives, and organized communities of farmers on water in Mediterranean countries. The conclusions of this Euro-Mediterranean program illustrate injustice and, at the same time, offer strategies for action.
In urban and rural situations alike, injustice stems mainly from the failure to take historical collection systems into account. Traditional and modern agricultural and drinking water collection systems are not seen to coexist and historical complexity is not integrated. This is the first injustice – ignorance of local knowledge and a lack of consideration for the ideas of people who are attached to their water rights and their ways of resolving certain conflicts. A second conclusion from the research program has to do with all untreated and potable water, and everything affecting the drainage and discharge of agricultural and urban water: there is generally no taking into account of the territorial geography or spatial organization; furthermore, citizens are not informed about the source of their water, either agricultural or urban. In the domain of humanitarian water, the issue cannot be limited to just installing and starting up a machine for water treatment and distribution. Where does the water come from: which network does it belong to? Which territories are connected to it? Is it ground water, is it from the mountains, and is it pure, impure, and so forth? Not informing people is a major failure in the three areas of water management – irrigation, drinking water, and humanitarian water.
The third injustice: people working at the local level don’t take into account social disparities (and these are many) and religious, political and social differences, etc. They must be considered. The issue of women has come up frequently in the international water debate. In fact, Principle No. 3 of the Dublin Statement from the 1992 International Conference on Water and the Environment recognizes their central role “in the provision, management and safeguarding of water.” As a result, the social issue, as such, is a bit of a caricature, focusing on only one aspect of exclusion.
Final injustice: intermediary institutions receive very little recognition from states. In the case of humanitarian water, I have the impression that that’s where the rub may be – at the moment of the intervention, when the need is for a structure, an institution to set rules. This is something that needs to happen when the system is first set up – not three weeks later, two months later, or three years later, when the technical system is failing.
Action strategies
What’s needed first is a pooling of expertise, based on real field experience. Second, it’s very important that governments clarify the boundaries of collective intervention. Otherwise there will be free riders, people who get themselves into the network but don’t participate in the collective process as they should. Third, there need to be internal rules, arrived at freely and in consultation, to produce original texts. This has to be a local process each and every time, since no model can ever fit every situation. Fourth element: it’s good to federate the technical structures, but also create a sort of water court to monitor conflict and establish a legitimate case law. Lastly (and for humanitarian water, this is clearly a huge dilemma), these things take a long time to put in place. It will obviously be impossible in some cases. However, I think we have to try really hard to establish viable local institutions.
Local action also has to be aggregated at other levels. At a minimum, it has to be aggregated at the provincial level, so that local experiences – rather than being isolated or forgotten –contribute to supporting citizens organized to regulate water management. I’d like to add that drinking water and agricultural water must not be pitted against each other, but combined, encouraging inter-institution practices, meetings, and the use of appropriate language.
Obviously, this is all very complex, and the fact that all of these problems are interconnected dictates even more reserve. The environment, nature, agriculture, climate, water, the market, society, and health issues are all interconnected. Given that they work with players in the field, scientists still have their work cut out to resolve all the issues related to the interactions between these eight elements.
Thank you.
Marc Le Pape, CRASH, MSF Paris
– Thank you so much for complicating the problem, and bringing up the usefulness of sociology. I was wondering, in relation to what you described, which water management model MSF uses the most. Maybe I’m wrong, but I think that it’s the interventionist model; we can no doubt discuss this. We’re going to go right to the second vantage point, as it would be useful for the discussion to address how the different areas of debate and operations fit together, at all levels.
ACCESS TO WATER: TRANSNATIONAL DEBATE
PRESENTATION BY BENOÎT MIRIBEL, PRESIDENT OF ACTION CONTRE LA FAIM
I’m very pleased to have been invited to speak here, to talk to you about an experience and an ongoing reflection within ACF concerning international debates on water and, more specifically, the right to water.
So why get involved in these debates? I’m going to talk about right-to-water issues, beyond the July 28, 2010 UN resolution on “the right to safe and clean drinking water,” and its adoption by the Human Rights Council in September 2010. The right to water and sanitation has become a human right. As with all rights, now we have to see how it will be applied.
I’d like to add that I’m not the only ACF person here today – there are some former ACF colleagues, of course. Current colleagues include Jean Lapègue, ACF’s water and sanitation coordinator, our vice president Jean-François Lamoureux and some other operations managers. How do we organize water management in our intervention contexts? How, for example, do we organize management of the water systems we set up, such as bore wells, etc., in the regions of Weh in Burma where we are assisting the Rohingya who were thrown out of Bangladesh? Things vary depending on the context, from one continent to another and one well to another. For example, in Burma, the head of the village insisted that the well be next to his house – no question of putting it anywhere else. We know from experience that the people need to take ownership to ensure proper maintenance and good practices. So before implementing the program, we held discussions in the village to determine where to put the water collection point, where to locate it so that it would best respond to the needs of the village, which wasn’t necessarily where the head of the village wanted it. ACF also formed water management committees. This is an example of how, when we intervene, we don’t simply put in a well or spring water collection system or gravity-feed network; we also think about ownership by the people, and meeting their needs. Of course, in an emergency situation we also supply the water that’s required. Should we be considering sustainability, even in emergency situations? Yes, if we agree that sustainability meets some purpose or need.
As we go from the local to the national level, other challenges emerge. Are we looking to make our actions in humanitarian contexts sustainable, or not? There are some situations where we know full well there won’t be sustainability. That’s the case right now in Somalia; the people working in the country know that sustainability is not viable. Nevertheless, we’re trying to look ahead, as if sustainability will become viable. Generally speaking, we believe we have a “duty” or responsibility to try for sustainability, insofar as it meets support from the population. The Millennium Development Goals give rise to another question for us. Some multinational corporations have appropriated the goals; adopting the language of the environmental movement, they say, “Yes, people must have access to water, etc.” We told ourselves that we had to talk to these companies, to compare their vision with ours. In numerous meetings, we’ve had to debate the numbers used for the Millennium goals. Indeed, that’s what the Goals are – numbers: to reduce the number of people who don’t have access to safe drinking water and sanitation by half.
The numbers’ issue was raised during a conference on water and health organised by the Merrieux Foundation in March 2010. One of the speakers brought up the differences in numbers between World Bank engineers and WHO doctors; they weren’t at all the same. To get back to the Millennium Development Goals: soon they’ll be presenting figures showing that the «reduce by half” goal has been met, because in North Africa, China, and some other areas, the people will have got access to water. We, on the other hand, believe that our first responsibility is to ensure access to water for the most vulnerable, those who don’t always have access to the programs that have been launched by the UN or supported by corporations. In other words, doesn’t the announcement about the drop in the number of people without access to water ignore the disparities suffered by the most vulnerable? Will it be enough, in a few years, to say, «Look, we improved the overall access to water numbers on the planet?” We believe it’s important to focus on vulnerability and quality – not merely numbers. This is the sort of debate we’ve been having at round tables with businesses – they show that they can contribute, in their way, to the Millennium Development Goals and respond to the challenge, if governments and donors give them the means to do it. Our duty as an NGO is to say, “Listen, okay, but which countries and which people?” “What does access to water mean in the first place?” Is access a tap in the home, an accessible pump, or what? When you say access to water, what do you mean? Can just anyone take up the challenge, or is there a legal basis each time? What’s the responsibility of the country involved? And at the international level, what about the right to water, sanitation and hygiene? And I haven’t even started on the debate over WHO definitions and standards. A leading specialist in water standards, Philippe Hartmann explains that ultimately there’s no such thing as pure water, from a biological point of view – it’s a set of standards defined by a state. Every time we’re invited to these debates, different players, seeing government willingness and an international opening, seize on these questions too with challenges almost the same as ours: “Yes, we’re going to give access to water too, that’s what we’re going to do; how can we do it?»
In the 1990s – I’m going to overstate a bit – ACF watsan teams were more focused on technical development. With the Thais we designed a drill, PAT, and made some progress. What’s more, Jean-Michel Vouillamoz, who ran the watsan department, did his thesis on using nuclear magnetic resonance to try to sound the water before launching drilling that could turn out to be futile. In the 1990s, we made a lot of advances in terms of technology and expertise. And in the 2000s, ACF tackled these issues of positioning. Seeing the growing importance of the World Water Forum, I went to Mexico in 2006. Some ACF people were saying, “You’re going to travel to Mexico, what’s the point of going?” But I wanted to see what the Water Forum was all about. We felt that we NGOs also had a responsibility to make our experience and voices heard by talking about our intervention contexts. It was a kind of trade fair; it was the same in Istanbul, there were lots of people selling water and technologies. In the end, should NGOs attend, or not? To send which messages? There are questions every time.
There was a change in the 1990s, with debates over governance and neoliberal policies. Researchers had also evolved in their definitions and on water-related economic and social issues. Then there’s the question of free water. Is water free? Yes, water is free, the question is, who pays for making water accessible, whether from the jerrican or the tap? Water is free like the sun; it’s there, it exists...it can rain. But tomorrow, someone could start charging for the sun; if you’re stuck and that person says, “If you want sun, go onto the terrace, but you have to pay.” Suddenly, you have to pay for access to the sun, even if the sun itself is free. Danielle Mitterrand says that water should be free, but water is free anyway; the question is, who pays the cost of getting the water? That’s where the vulnerable population issue comes into it.
Access to water in urban settings is one area where ACF has made progress in the 2000s. We know that the number of vulnerable people living in cities is growing, and will continue to do so. We see that access to the water supply integrates people; sociologists have established this. People feel they exist because they get a bill (the amount of the bill, and who takes care of it, or not, is another discussion). We’ve seen this in some big cities, in the megacities in Africa, and it’s been the highlight of many articles. We observe that water is also a social issue that goes beyond health, beyond the aspects we usually address.
I mentioned the players who are proactive in these debates, the donors who believe it’s part of their strategy, and the companies that latch onto it and ask for funds for their access to water projects in developing countries. Not necessarily a bad thing, but in which contexts are these strategies going to be implemented? How are the fund allocations decided? And should field NGOs be involved in advocacy around these issues? Should we stay out of it, because it’s not our area, we’re humanitarians, we do our work and that’s it? Or should we take part in these discussions, because they involve human rights and the principle of responsibility, because it’s also being concerned for people’s dignity, and making sure their rights are heard.
So, what is the right to water? There are connections with the declaration of human rights in various forms and on July 28, 2010, at Bolivia’s request, “the right to safe and clean drinking water” became, for the United Nations, “a human right that is essential for the full enjoyment of life and all human rights.” It’s also an aspect of humanitarian law, which considers drinking water reserves and irrigation works as goods essential to survival, and as such, protected. There are, of course, many other questions and challenges beyond the legal ones. In particular, the issue of access: free water, but financially inaccessible – that’s the question. The right to water should not trample other rights, and that’s no simple matter.
We also have to consider the issue of local governance, which Thierry Ruf has brought up. There are a lot of areas where the government is neither in a position nor able to intervene, where public-private partnerships are necessary, but there still needs to be public responsibility with regard to the issues of dependency or non-dependency. Sometimes there is access to water for a limited period, because a donor contributes; then two or three years later, people connected to the system are overwhelmed with bills and simply can’t pay them. In a lot of cities we also see trafficking, a black-market in water. The local social and economic impact must be taken into account; as a humanitarian NGO involved in such contexts, it is our duty. My presentation has been an opportunity to show you that the right to water debate continues at ACF. Before I was elected president in June 2010, we had a board meeting that wasn’t really supportive of involvement in the debate. The board’s argument went broadly like this: “It’s not your job. Field operations – that’s what you should focus on.” So does wanting to do more operationally mean that we shouldn’t take part in the debate, and contribute knowledge from the field, for the benefit of people and, more particularly, vulnerable people? Obviously, it would be risky for ACF to change fields and work only on the right to water. But to what extent? As we become more and more effective operationally, with high-performance technologies and water system governance methods developed over the years, shouldn’t we also concern ourselves with these much broader issues of water that are being appropriated by other actors? This is still an open question within ACF, and will be dealt with in our board meetings. This was a chance to talk about it with you.
DISCUSSION ON THE PRESENTATIONS BY THIERRY RUF AND BENOÎT MIRIBEL
Jean Lapègue
– A few comments about the right to water. First, I find it refreshing to hear the problems of rights and governance discussed in the humanitarian sphere. Not only is it refreshing – it’s necessary. Indeed, looking just at the Millennium Development Goals, in terms of water coverage, we know that 886 million people don’t have access to water, and that 2.6 billion people don’t have access to sanitation. So as humanitarians, we can already ask ourselves the question: we’re not going to put an end to the problem with our traditional programs like the ones we’ve developed at ACF over the past twenty-five years, are we?
ACF, for example, brings water to 1 million people a year; that’s our “annual sales figure”. Obviously, an absolutely microscopic drop in the bucket compared with the problem. That’s my first comment.
My second comment concerns the ACF Board. I think the board took a position on an issue of advocacy. It’s true that when we start getting involved in the right to water, we enter the international arena. We ourselves were there, at the European Parliament, to defend the right to water, obviously – as Benoît Miribel was saying – to protect access to the resource for the most vulnerable. As soon as we start getting involved in these issues, we abandon a bit our sacrosanct neutrality to stick our neck out with big corporations and politicians. And that concerns the very essence of humanitarianism. We’re in a paradigm: are we being interventionist, are we putting a sticking plaster on a wooden leg, or are we going to the heart of the problem – state governance, in particular? We decided, after Mexico, to work on governance and to try to move the states forward in the debate. As it happens, the decisions made by the UN in July 2010 and corroborated by the Human Rights Council in September show that the question is now settled. The right to water is a reality, and at ACF we can no longer ask ourselves the question: should we, or should we not, fight for it? It doesn’t need to be fought for, it exists. Now, what are we going to do to implement it, given that it mainly applies to urban and vulnerable populations? Another point that I think it’s important to raise.
I have had two practical experiences in the field with regard to the right to water. During the Israeli bombing in the latest war in Palestine, ACF brought water to 50,000 people in the Gaza Strip. At the same time, we were meeting with the UN and institutional donors in Amman, Jordan, to work on the international right to water in times of war. As Benoît Miribel reminded us, the right to water isn’t a development issue; it’s also a humanitarian one. International humanitarian law deals with several aspects of the right to water. As humanitarians, we shouldn’t protect ourselves by saying that these are development issues; it’s not true. It also involves the purely humanitarian sphere. That’s the first important point.
The second experience concerns our recent work in the slums of Côte d’Ivoire – in San Pedro, in particular. There we’re dealing with the problem of the price of water and urban vulnerability. When you work in urban and peri-urban settings, water has a price and the bill is, or isn’t, paid by the people. There are regulatory mechanisms – adjustments to the price of water. Working in urban settings also means working with institutions, and thus with the government and water companies, on the notion of urban vulnerability. At what point does a family need support to get access to water?
In fact, dealing with the right to water in urban settings today means working on the price of the resource, support mechanisms and ways of facilitating access to these basic services for the most vulnerable.
Rony Brauman
– I have one comment, but just for the sake of discussion because I think that if we go too far in this direction we’re going to get away from the focus of the symposium.
My comment is that water is, first and foremost, a need; a physiological need, a vital need, and it seems to me that the confusion between right and need is more muddling than enlightening. I think – contrary to what’s been said – that NGOs are enthusiastic about adopting and appropriating “the rights” vocabulary. For the past twenty years, we’ve witnessed an endless accumulation of rights: the right to water, to development, to the environment, the right to culture, and so on. I don’t think this approach is at all productive. So the question isn’t whether a humanitarian NGO should or shouldn’t get involved in the area of rights; I don’t think the question clarifies anything. The question is rather how far are these rights going to pile up, and to what extent that clarifies things. I see it more as a source of confusion.
The fact that the Human Rights Council adopted the resolution is anyway pretty laughable. The Human Rights Council is a union of dictatorships – that its members adopted one more right is nothing but rhetoric; it has absolutely no political significance. My comment is made for what I call “the sake of discussion,” but it isn’t necessarily directly related to the topic.
Thierry Ruf
– I’d like to comment on the issue of water being free. I’d like to discuss this, because I have several examples of tough discussions with people who have said to me that it isn’t normal that Egyptian farmers don’t pay for water, that they get water for free. In fact, Egyptian farmers have paid three times over for the infrastructure they’re using now. In the 19th century, it was their hard work that dug the irrigation canals. It was a colonial economy, and the canals were constructed to produce cotton for Europe. Then Egypt had a public debt it couldn’t pay. So, in 1870, we intervened as colonialists. There were European ministers, there was a conquest. For forty-five years, until 1914, they paid with monetised cotton; they repaid both the accumulated debt and the infrastructure modernization for the dams that were built during the colonial period. Then, under Nasser, they paid for the Aswan Dam, since they produced cotton for the Soviet Union. Ultimately, farmers, and they know full well, paid for the whole infrastructure we see today.
Although the Irrigation Minister is a member of the World Water Council, which has promoted a somewhat new approach to paying for water, etc., he has never applied it in his own country, because the historical and social conditions don’t allow it. What I mean by this is that Egypt has found a solution – that is, no charge is made for water, and farmers control local water with pumping. They provide water for food production and also for the government. The government thus pays itself indirectly, and pays for maintenance indirectly. It’s a water economy that isn’t organized through individuals paying a bill. Having a person pay a water bill exists in other societies; it’s socially accepted, it can be expanded, but it isn’t everyone’s vision.
The 1992 Dublin conference, the start of the major water conferences in the world, pointed out that water is a commodity. Yet, drinking water is free in Dublin. In the 19th century, the City of Dublin chose a method for paying for the public works whereby the tax on buildings would pay for infrastructure and running costs; there wouldn’t be meters. So you have a society that lives with free water, but not completely. Of course there are charges, there are costs, and all that’s taken care of. You have to look at how each place operates, as there are different methods. The system of volume management with a meter isn’t universal, in my opinion.
Alexandre Brailowsky
– I’d like to talk about the Millennium goals. If I understood correctly when I was in Stockholm, the progress in some countries will make it possible to announce fairly decent numbers, but at the same time, if we look by continent or by country, it’s much more negative than that. One number is really alarming: the population in urban areas that doesn’t have access to water has gone up 20% over the past eight years. That means there’s a way of presenting the numbers that’s really unbalanced.
I think there’s a connection between saying the problem is extremely complex and hard to explain, and the lack of results. I think we need to draw a parallel between the two. Why do I say that? According to one of your geographer colleagues, Sylvy Jaglin, it’s not so much water management that’s complex. What is complex, because we don’t do it, is taking the territorial and the local specificities into account. Otherwise, the water problem, looked at universally, is quite simple: there’s an organizational responsibility that falls to the public authorities, and management by an operator. In fact, it’s relatively simple. There’s a third player, the user, who needs to be involved as far upstream as possible. So it’s not very complicated. What bothers me is that normally, when you understand something, it can be explained simply. We have trouble making a connection between the fact that, on the one hand, the international community and all the people working on water access are incapable of expressing an issue in a simple way, and on the other, the lack of results. For years they’ve been announcing objectives, but never achieving them. In the early 1980s it was the International Decade for Clean Drinking Water, now it’s the Millennium Development Goals. Where simplicity would be possible, there’s often confusion. For example, on the right to water issue – they put cross-border water issues and agricultural versus domestic use all in one bag, when logically it would be simpler to talk about the right to water, which is the right to a resource, on the one hand, and the right to a service, on the other. Wouldn’t it already be simpler to formulate it that way?
François Mansotte
– I have a comment and a question. In France, the right to water isn’t quite so simple. We have a growing population that doesn’t have access to water, even though we have social welfare that helps pay water and electricity bills as long as people have water and electricity meters. But when you live in a squat, when you’re totally outside the system, you don’t have a meter, so there is no social welfare.
We have an overseas department like Guyana, where 15% of the population can’t get any help with their drinking water, because these 15% live in slums or have no roof over their heads and don’t pay a water bill, because they don’t have meters. There is social welfare that would help pay the bills, if these people had a meter. That’s a fact.
Next, I’m going to say something very sexist. Water problems, both internationally and in France, are for women – not to paraphrase Victor Hugo’s Les Misérables and the Thénardier family, where it’s always a little girl who carries the water. In every country in the world, it’s the women who carry water, and it’s the women who take care of sick children, but it’s not the women who make the decisions. You haven’t really dealt with this subject, and I’d like to hear what you have to say about it in relation to the contexts in developing countries where there is no access to clean water. In certain cases, men always make the decisions, and the decision about clean water doesn’t always take precedence.
Benoît Miribel
– I’m not sure it’s as categorical as that. The women in Africa play a key role, including in governance.
That reminds me of an anecdote on the role of women, cited by the ICRC at the “Water and Health” colloquium in March. The ICRC had a program in an Asian country, where they were trying to make the lives of the women easier as they spent hours fetching water. A year later, an impact assessment study showed that a lot of the women had become a bit alcoholic and smoked, because they were alone again. When they used to go to the water works, there was a social life, they talked. After the program was completed, they felt somewhat disconnected. That’s just a critical anecdote about our intervention strategies.
On another note, I also agree with Rony Brauman’s observation on the UN Human Rights Council. ACF in Sri Lanka saw the total inefficacy and impotence of the Human Rights Commission. It’s a farce; when you’re in Geneva, they make such a big deal. But does that mean we should give up the fight there?
Marc Le Pape
– Everyone here agrees on the Human Rights Council, so I don’t think it’s worth much more discussion. It would be useful to get the reactions of some of the logistics people, from MSF or not, to the two presentations. For example, there’s what Gilles Isard said this morning, when he was talking about a potential conflict around sharing water between farmers and humanitarians. He mentioned an issue that came up again. Could you respond a bit? All of these complexities that have been mentioned – can you take them into account, can you manage them, should you manage them? Especially the “complex social compromises” that Thierry Ruf mentioned?
Gilles Isard
– I’m going to quickly describe the situation I was faced with in Thailand. We worked for a few years in a refugee camp, where we found ourselves involved in a conflict over the sharing of access to water. It was a small drainage basin with originally less than a thousand inhabitants, many of them farmers. The refugee camp was set up on the drainage basin. There were 8,000 refugees, and all of a sudden, MSF took the water from the small river. We used it, as a priority, to supply the refugees. We quickly found ourselves in conflict with the local farmers; while there was lots of water in the river during the rainy season, there was hardly any during the dry season. And this, of course, was exactly when the farmers needed the water to irrigate their crops, because it was the dry season and it was very hot. Naturally, we had to negotiate and find an agreement on sharing the water effectively; otherwise, they repeatedly sabotaged our system. It was an eight-kilometre-long gravity-fed system, so there was lots of room for sabotaging the pipes. We had no choice, and it was just as well. Our mistake was in not having understood the situation properly from the beginning. If we had done things differently and more appropriately, we would have known from the start that we’d have to deal with this type of situation, and find some way to work together to figure out how to share the resource.
In connection with the issues of productivity, water becomes a tradable commodity – it’s a question of finding how to make the most money from a cubic meter of water. As a result, water – because it brings in money – will be first distributed to a factory or used for irrigating high value-added crops. And last, at the end of the line, are the poor, those who can’t pay – they get what’s left over.
This can be a problem in developing countries, where there isn’t a lot of control and regulation, because water is becoming an increasingly scarce resource or, at any rate, increasingly poorly distributed. Improvements are made first where there’s money to be had, and the mouths of the poor are not where water makes the most money.
Jean-Hervé Bradol
– People are deprived of an economic resource – I can’t comment much on this point as it’s not my field. What has struck me in the area of water governance is the frequent use of the medical argument – we’re getting involved in this domain in order to indirectly promote health. But that doesn’t necessary follow. When individual household meters are installed, you see a drop in consumption. Usually, after a while, the individual household payment system puts economic pressure on the family, which will very often reduce its water consumption. The same with electricity. In some cities where there weren’t really any individual electric meters, we’ve seen prepaid card systems set up. When the credit on the card is used up, the electricity is cut off. In the end, the family itself restricts its consumption. In addition, medically, we’ve seen that it’s ingested water that’s decisive. We’ve seen, over the course of the day, all the conditions that are needed to ensure that the water produced and distributed by central systems truly contributes to good health: you need an almost perfect system that never runs out and, most of all, running water, which is rarely the case.
I have, above all, observed a policy of rationing created by fairly authoritarian, centralized production systems, with little done to make systems that improve water quality at the household level more accessible. These are the filters we talked about this afternoon; they may offer the possibility of making a difference in terms of disease and death among the “vulnerable” everyone’s talking about but, as we’ve seen, this primarily means infants. We talked about the “under-five” threshold, because that’s what’s used most often, but if we look more closely, it’s the youngest children amongst the under-fives who are at greatest risk of dying. While their deaths are often used for political mobilization around water issues, there isn’t much in the solutions put forward that’s going to affect them, or that we can expect to make an impact on them.
When I attend these discussions, I wonder about the health impact of the measures taken. They don’t target the “right vulnerables,” if you know what I mean. In any case, if you consider the family as a whole, it’s more rationing policies that are implemented via distribution and payment systems. That’s what truly baffles me.
Benoît Miribel
– Indeed, that’s just what I was saying. The questions you’re asking – we’re asking them too. The Millennium Development Goals say “reduce the lack of access to water,” they don’t say “reduce mortality.” They don’t mention mortality, and in particular, that of the infants you identify as most vulnerable.
Marc Laimé
– Looking at the intense upsurge in interest around the right to water over the past few years, I wonder whether things aren’t taking a completely Orwellian turn. At the same time as we see – and this is absolutely irrefutable – that the Millennium goals will not be met, that the situation is continuing to get worse everywhere, and that the international community is not fulfilling its commitments, the public arena is being taken over by the idea of the right to water.
I’d just like to point out a few facts. In Europe, according to the OECD, not all former Eastern bloc countries (100 million people) currently have proper rights to water access. Contrary to the figures cited a moment ago, Gérard Payen, one of the most distinguished representatives of the French business community, recently quoted the number of people who don’t have proper access to water and sanitation as four billion.
To finish, in December 2006, France passed its third major water law, the first article of which contains a categorical reference to the “right to water.” To date, this right to water is completely ineffective. There’s a heated debate going on within France itself on how to help the poorest. The outcome of an extremely complex political and legislative process will be that users who can afford to pay will pay for those who cannot. All this should tend to make us very humble and cautious, especially with the World Water Forum coming up in 2012 in Marseille, where France is going to lecture the whole world on the right to water. The topic has become an instrument, a veritable talisman enabling us to dispense with the political and social aspects of water, and the tensions and conflicting objectives that Thierry Ruf talked about.
Thierry Ruf
– I’d like to go back to the issue of the role of women in water management. True, at the 1992 Dublin conference, which was preparatory to the one in Rio, the role of women was the subject of the third of the four principles guiding worldwide public policy. But precisely, this principle of the inclusion of women masks all the other social exclusions. Incidentally, have you noticed that in the major international debates on water – at the forums and intermediate conferences – 95 to 99% of the people at the podium talking about this issue are men? Water leaders are almost all men. Why is the political, public, and business leadership still dominated by men?
Women’s access to resources like land and water in local societies sometimes poses enormous problems of adaptation. The Dutch, who pay particular attention to the subject, have tackled these issues regularly. In Andean countries, where mountain irrigation is widespread and constitutes a mode of social and political organization that has to reconcile the needs of indigenous communities with the need for government planning and market integration, action research by NGOs, academics, and local development organizations has changed the paradigms of water and social organization. There are now indigenous communities where the women are organization leaders in a global struggle against poverty and exclusion. So the situation is changing, often faster than governments and lobbies. Those who lecture others about women in the economic organization of water should apply what they’re saying to themselves.
There’s a second aspect that’s very important to me. In the suburbs of the big Moroccan cities, I’m seeing public fountains that used to give free water to the residents of slums, people who generally don’t have official documents or legal status, being converted; the service has been delegated to a private French company. The company has installed digital card devices at these street fountains that deliver water according to different schemes. This poses an ethical and economic problem. People who were undocumented now have to declare themselves to the administration – that is, register. Whether this is a good thing or not, I don’t know. The inhabitants are monitored by way of water. The electronic card delivers a forty-litre limit per person; this meets basic needs. Once the limit is reached, water has to be purchased. Will family finances permit it? Owning or losing a card is going to become an issue. Also, daily needs fluctuate considerably according to family situations (e.g. mobility, taking people in, social life).
Obviously this is going to create discrimination, because one part of the population won’t be able to enter this system of contractualised water access. Since that part of the population will no longer have access to free water at the public fountains, where will it go? To water from bad wells drawing from the water table. Yet in the outskirts of these cities, polluted for decades, this is the worst possible water, from a sanitation and public health standpoint. So, while applying the Dublin principles in this context solves the problem of financial equilibrium for the water management company – which is putting out self-congratulatory press releases – nothing has been evaluated in terms of financial efficacy or social and medical impact. Yet the predictable shortcomings of the smart card system may generate direct and indirect public health costs not yet incorporated in the balance sheet. These costs will come ten or fifteen years down the road, when we become aware of all these problems. The next generation will have to deal with them. Today, we usually look no further than the price of water billed by the cubic meter delivered, as if it were some kind of marketable good. But water systems have a history, a water capital that may be ancient or modernized, inherited but poorly evaluated in financial terms. The dysfunctions, exclusions, and corruption also have to be corrected in the near and distant future, and its amenities are hard to quantify. In a way, by treating drinking water – and soon agricultural water – as a marketable commodity, we are passing on the conflicts we don’t want to resolve today to future generations. In society, water is often monopolized by the powerful. Policy serves to contain the appetite for domination and restore fairness and humanity in access to resources.
According to political commentator Leif Ohlsson, water management goes through three successive phases, or “turns of the screw”. First is the hydraulic era, where water is provided free to all by mobilizing energies and knowledge; canals are dug, water is collected and provided free of charge. The second “turning of the screw” occurs when certain segments of society are thought not to be using the water allocated to them properly. This is the water productivity phase, where water has to be reserved for those who produce the most physical goods with a drop of water. In agriculture, this means water is allocated to the most intensive farmers with the highest agricultural yields. In urban settings, it is undoubtedly the most dynamic cities with extraordinary development. Blind exclusion takes place, obviously affecting the most vulnerable populations with no means of production or “up to standard” housing. But this initial way of managing demand isn’t enough. There are still competing uses. In a third turning of the screw, the criterion becomes the economic efficiency of a drop of water. This neoliberal option relies on price-based regulation and comparative advantages. Better to give expensive water to those who produce the most value added. In agriculture, ancient rights are taken away from poor farmers and handed over to entrepreneurs freed from collective constraints by technological progress. Paid water serves individual interests. In towns and cities, neighbourhoods become discrimination zones where some areas have groups of well-off families demanding a high level of service, while the slums experiment with smart cards. At the interface between urban and rural, they’ll take resources away from a farming community to build a golf course (which may not even end up paying a high price for water), or to set up a mineral water installation when the source is appropriate – but without including the long-term users in such a radical and brutal transformation. If these three turns of the screw happen everywhere in the world, we’ll end up excluding three quarters of humanity from access to water – and not just for consumption, but for food too.
Obviously, in the context of humanitarian disaster relief you could think that the most important thing to do would be to supply the devastated populations with water treatment equipment. When we do this, we’re in the initial phase. But the two other turns of the screw are not far off, and there’s a substantial risk of hurting the most fragile – those we want to help the most. That’s why I think it’s very important to intervene at the social and organizational – as well as the technical – level, and to make sure, once the emergency is over, that the new network is managed as a common good, and not subject to the mechanisms of social exclusion.
Dominique Maison
– I’d just like to respond to that point, and then I’ll return to a previous comment. It does seem to me that there’s a grey area at the junction of emergency situations and what we’ve developed in terms of rights; more long-term actions or, in any case, actions that are part of a more long-term approach, in a given governance, structure or institution. This gets back to the situation in peri-urban neighbourhoods, often home to people from other places – people from the countryside or from other countries, IDPs, refugees, and so on. There, there is perhaps a big grey area, insofar as these are the very people we don’t necessarily want to deal with, because we don’t necessarily want to see them – in the slums here or anywhere else. And I think that everybody has images to put behind that.
The second thing is related to what was said a little earlier about the issue of filters. I understand that it was being discussed in terms of effectiveness in a particular situation. I think, and perhaps I’ve been overly conditioned by the French system – centralizing, positivist, 19th century, etc. – but the collective water approach is a bit of a creed. I can understand the usefulness of filters, etc.; what I’m afraid of (and this is getting back to the access to water issue), is that the public authorities will abandon any attempt to provide access, and in my opinion, providing that access is society’s duty.
When we talk about filters and individual solutions, we in fact risk that abandonment by the public authorities. Take, for example, peri-urban areas; if there’s an NGO or whoever who wants to supply filters, they say, go ahead, I don’t have to supply them, I don’t have to draw the line, I don’t have to provide access. If someone else does it, so much the better. And look, it works, it’s excellent! But there is punishment for success; to my mind, we create a lot more inequality, because it’s within the household, or within vulnerable populations (women, children, etc.). In any case, that wasn’t the purpose – at least in France – of the late-19th and early-20thcentury public health revolution in public facilities aimed, if you remember, at fighting the massive cholera epidemics that threatened both social stability and the political system. That’s how our societies raised themselves up a little, at least regarding public health, and with inequalities between social categories and between communities.
One other question: involving the social aspect, that’s an idea, but as engineers, we don’t always have the tools – that is, we don’t necessarily have a blueprint for the type of societies or social structure it’s possible to intervene in.
I’ll end with an example. When – after a tsunami or other disaster – we have societies that have lost their structure, that are unstable, where 10%, 20%, 30% of the population has been decimated, sometimes even the opinion makers and the religious leaders, everyone we’re supposed to go through to facilitate implementation, what do we do? Does social access need to be created, or recreated? Should we wait for the group we are assisting to stabilize? Or should we try to promote technical solutions anyway – even if they’re not necessarily very interactive? We do have to do something in these cases.
Francisco Diaz
– With regard to that intervention, on the contrary, I don’t think the emergency and medium-term approaches are incompatible. The whole point of our interventions is precisely to be able to change gear according to the situation, in urban settings too. I worked for ten years in a slum in Guatemala where we set up a water production and management system administered through a local cooperative. It worked; it can be done. It takes time. There are huge conflicts to resolve with a multitude of both public and external players.
Something that’s fundamental to the success of this type of approach, in my opinion, is the very notion of project. The people, whether rural or urban, has to want something for the future, have a desire for something different, for improvement, or at least change.
CONCLUSION
Marie-Pierre Allié, President, MSF-France
Good evening. First, I’d like to thank all of the speakers and participants who have contributed to today’s very rich exchange of ideas.
The discussions bear out the fact that the water issue remains fundamental to a humanitarian organization like MSF. We saw an illustration of this not only with the presentation on the hepatitis E epidemic in Mornay, but also with Professor Hunter’s presentation, which dealt with the impact of diarrheal illness on mortality in small children. The importance of this issue also relates to the need to distribute not only good quality water, but also in sufficient quantities. We were reminded of that, and should not forget it, even if there was a lot of discussion about quality.
That being said, however, the options for intervention, methods of action, and operational responses raise a multitude of challenges for humanitarian organizations. These issues are first of all technical; we saw that in today’s discussions. While there are some solutions, many remain yet to be found. The challenge is also, and especially, to look for operational strategies that are most appropriate in the long term and effective in terms of their impact on the people we are trying to help.
I think this symposium has produced a fair number of ideas on which we can still make progress. I believe this is a crucial area into which MSF needs to put more effort than we have in recent years, even if water distribution has been an important part of our activities in the past.
Once again, I thank you all.
Période
Newsletter
Subscribe to our newsletter to stay informed about our latest publications. Interested in a specific author or thematic? Subscribe to our email alerts.
