
MSF and Ebola in Nord Kivu. Positioning, Politics and Pertinence
Natalie Roberts
This article was published on December 22nd, 2021 in the Journal of Humanitarian Affairs (Issue 3, Volume 3).
This article explores the actions of Médecins Sans Frontières during the 2018–20 Ebola outbreak in Nord Kivu, in the Democratic Republic of Congo. Based on the experiences of practitioners involved in the response, including the author, and on the public positioning of MSF during the first year of the epidemic, it argues that although the actions of response actors were usually well intentioned, they could rarely be described as lifesaving, may have exacerbated disease transmission as much as limited it and had the perverse effect of fuelling corruption and violence. The article documents and analyses contradictions in MSF’s moral and technical positioning, and the complicated relationship between the organisation and the international and Congolese institutions leading the response. It argues that the medical and social failure of the response was the result of an initial belief in a strategy designed at a time when the only realistically attainable outcome was to relieve suffering, and of the later inability of the organisation to convince the authorities in charge of the response to adjust their approach. It suggests that for future success new protocols must be elaborated and agreed based on a better social and political comprehension and a better understanding of the tools now available.
Introduction
The Ebola epidemic that occurred in eastern Democratic Republic of Congo, primarily Nord Kivu, between 2018 and 2020 was the first major outbreak of the disease since West Africa 2013–16. Dramatic biomedical progress was made before and during the Kivu outbreak, including the rapid development of effective tests, treatments, vaccines and care interventions. Response efforts were marked by an extraordinarily large budget dispersed among a plethora of scientific, public health, UN and humanitarian organisations, as well as the Congolese government and state institutions. Building on its long-standing presence in the region as well its prominent role in the response to the West African epidemic, Médecins Sans Frontières (MSF) positioned itself as a key response actor from the first day of the outbreak. Yet despite incorporating all the elements considered requisite for success, the Kivu response was eventually labelled ‘a systematic and catastrophic failure that left thousands dead’Médecins Sans Frontières (2020), ‘How the Ebola Response Failed the People of DRC’, opinion, 24 March, www.msf.org/how-ebola-response-failed-people-drc (accessed 5 October 2021)..
After working in Nord Kivu for the French section of MSF between February and September 2019, I was asked by the Director of Operations to research the epidemic and MSF’s activities in response to it, to inform future choices. Why and how did the response ‘fail’, and what was MSF’s contribution toward that? Could we avoid repeating these errors in future, and how? As well as reflecting on my own experience and reviewing MSF internal documents related to the outbreak, I interviewed MSF and non-MSF practitioners involved in the response, asking them to describe their intentions, their actions, the obstacles they faced and their evaluation of the results. Working on the basis that MSF’s freedom of action ‘depends largely on the organisation’s ambitions, the diplomatic and political support it can rely on, and the interest taken in its action by those in power’Magone, C., Neuman, M. and Weissman, F. (eds) (2011), Humanitarian Negotiations Revealed: The MSF Experience (London: Hurst & Co)., this article explores the contradictions in MSF’s moral and technical positioning before and during the Kivu epidemic, and analyses what impact the complicated relationship between the organisation and the international and Congolese institutions leading the response had on MSF’s actions, and on our perceptions of them. The article is organised chronologically, first providing background, then examining the significance of selected key events during the first year of the epidemic on the positioning of the actors executing the response. It focuses on MSF, for whom two pivotal events occurred during that period: attacks on two MSF-run Ebola treatment facilities in February 2019, and changes in the leadership of the response in July 2019.
Context
MSF and Ebola in West Africa
The largest epidemic of Ebola ever recorded started in West Africa in late 2013 and ended in 2016. MSF received praise for the rapidity and scale of its response, and for highlighting the inadequacy of the World Health Organization (WHO) Birrell, I. (2014), ‘The Ebola Outbreak Has Produced Some Real Heroes – but Western Governments Are Not among Them’, Independent, 19 October, www.independent.co.uk/voices/comment/ebola-outbreak-has-produced-some-real-heroes-western-governments-are-not-among-them-9804894.html (accessed 5 October 2021).. MSF was ‘considered a reference point as a medical and humanitarian organisation, with major legitimacy in the Ebola response’ and was the driving force behind the implementation at massive scale of an operational strategy originally developed to react to the usual, much smaller epidemics of the disease Médecins Sans Frontières (2016), MSF OCB Ebola Response – Medico-operational. Report. MSF Stockholm Evaluation Unit, http://cdn.evaluation.msf.org/sites/evaluation/files/attachments/ocb_ebola_review_medop_final_2.pdf (accessed 5 October 2021)..
When in 2014 recommendations were made at the European Parliament that ‘the lead [for the response] should be given to an NGO [non-governmental organisation] – in this case, Médecins Sans Frontières’, MSF directors insisted that it had ‘neither the legitimacy nor the skills nor the desire to take on the political leadership of the Ebola crisis in West Africa’ Nierle, T. and Jochum, B. (2014), ‘Ebola: MSF n’a pas à remplacer les Etats pour gérer la crise’, Le Temps, 30 October, www.letemps.ch/opinions/ebola-msf-na-remplacer-etats-gerer-crise (accessed 5 October 2021).. Based on his past ethnographic research of the organisation, RedfieldRedfield, P. (2015), ‘Medical Vulnerability, or Where There is No Kit’, Limn, Issue 5: Ebola’s Ecologies, https://limn.it/articles/medical-vulnerability-or-where-there-is-no-kit/ (accessed 5 October 2021)agreed that MSF was constitutionally ill suited to lead the response as the organisation ‘operates as independently as possible … and issues moral exhortations, not commands’, making its role reliant on the existence of a political as well as technical health infrastructure. However, in a situation where the unfamiliarity of national health authorities with the disease was exacerbated by the failure of the WHO to provide effective leadership, MSF’s apparent technical superiority, capacity for rapid action and vocal public positioning meant the organisation was still regarded by many as the de facto leader of the responseCheck Hayden, E. (2015), ‘Ebola Outbreak Thrusts MSF into New Roles’, Nature, 522, 18–19, doi:10.1038/522018a.. After criticising the leadership of the WHO as ‘slow, derisory and irresponsible’Médecins Sans Frontières (2014), ‘The Failures of the International Outbreak Response’, opinion, 29 August, www.msf.org/ebola-failures-international-outbreak-response (accessed 5 October 2021)., MSF convened international discussions and trained other organisations, including the WHO, on its Ebola protocols. During the height of the epidemic, between March 2014 and March 2015, MSF spent €77 million on the Ebola response and employed 5,300 response workers in West Africa, among whom 28 were infected with the virus and 14 diedMédecins Sans Frontières (2016), An Unprecedented Year: Médecins Sans Frontières’ Response to the Largest Ever Ebola Outbreak. Report, www.msf.org/report-ebola-2014-2015-facts-figures (accessed 5 October 2021)..
Yet once the epidemic was over, after more than 28,600 cases and 11,300 deaths, there was little critical reflection on the quantifiable or qualifiable outcomes of the MSF intervention, notably on whether it had resulted in any tangible reduction in mortality, disease transmission, or the duration of the outbreak; or whether the results achieved warranted the massive resources deployed and the heavy physical and psychological consequences suffered by responders. Prior to 2013 MSF had accepted the failure of its Ebola responses to save lives or limit transmission, partly due to the absence of effective vaccines or treatments, but had justified continuing to intervene primarily to alleviate suffering Redfield, P. (2015), ‘Medical Vulnerability, or Where There is No Kit’, Limn, Issue 5: Ebola’s Ecologies, https://limn.it/articles/medical-vulnerability-or-where-there-is-no-kit/ (accessed 5 October 2021).. During the West African outbreak, disagreement arose about the prospect of MSF’s actions meeting even those ambitions. Some doctorsMcNeil, D. G Jr. (2015), ‘Ebola Doctors Are Divided on IV Therapy in Africa’, New York Times, 1 January, www.nytimes.com/2015/01/02/health/ebola-doctors-are-divided-on-iv-therapy-in-africa.html. ;
Médecins Sans Frontières (2016), MSF OCB Ebola Response - Medico-operational. Report. MSF Stockholm Evaluation Unit, http://cdn.evaluation.msf.org/sites/evaluation/files/attachments/ocb_ebola-review_medop_final_2.pdf (accessed 5 October 2021).felt that MSF care protocols prohibiting the use of intravenous fluids both missed an opportunity to attempt to increase survival and did not go far enough to relieve suffering. Rony Brauman, a former president of MSF, observed that the organisation would have to decide whether it prioritised ‘treating the epidemic, or the patients of the epidemic’ Losson, C. (2015), ‘Interview. Rony Brauman : contre Ebola, « le traitement symptomatique a parfois été négligé, voire oublié »’, Liberation, 3 February, www.liberation.fr/terre/2015/02/03/parfois-le-traitement-symptomatique-a-ete-neglige-voire-oublie_1194960/ (accessed 5 October 2021).. Yet despite calls by another former MSF president, Jean-Hervé Bradol, to open a debate around some of MSF’s operational choices in West Africa Bradol, J-H. (2016), ‘The Response to the Ebola Epidemic: Negligence, Improvisation and Authoritarianism’, Alternatives Humanitaires, inaugural issue, https://alternatives-humanitaires.org/en/2016/01/15/the-response-to-the-ebola-epidemic-negligence-improvization-and-authoritarianism/ (accessed 5 October 2021)., few efforts were made to continue the discussion. The MSF International President, Joanne Liu, who had privately expressed support for doctors dissatisfied with the quality of care that the organisation had to offer, publicly commented: ‘We’re going to get a lot of people who haven’t treated a patient who are now the world experts, and who are going to give us lessons’ Check Hayden, E. (2015), ‘Ebola Outbreak Thrusts MSF into New Roles’, Nature, 522, 18–19, doi:10.1038/522018a.. The general belief inside and outside the organisation was that MSF’s intervention in West Africa had been an overwhelming success.
The Equateur Outbreak
By 2018, the landscape of Ebola response had changed. The weakness of the WHO in West Africa had directly contributed to the establishment of the WHO Emergencies Programme, intended to ensure rapid deployment capacity and the establishment of clear leadership at international, regional and country level in response to public health emergencies WHO (2017), Emergency Response Framework – Second Edition (Geneva: WHO).. Since its launch in 2016 the Programme had intervened in other crises, but an outbreak of Ebola declared in Equateur region of the DRC in May 2018 was considered its first real test.
The DRC had already experienced eight previous Ebola epidemics, mainly small and self-limiting, but in Equateur the WHO, working jointly with the Congolese Ministry of Health, deployed at unprecedented scale when case numbers were still low, aiming to ‘go big and go fast’ to avoid the mistakes it had been accused of in West AfricaCrawford, A. et al. (2021), The Democratic Republic of Congo’s 10th Ebola Response: Lessons on International Leadership and Coordination (London: ODI).. An initial budget of $57 million was requested from donors, and most was spent within the first month WHO (2018), ‘Bulletin humanitaire, R.D. Congo, Numéro 8’, 8 May, https://reliefweb.int/sites/reliefweb.int/files/resources/bulletin_mensuel_mai_2018.pdf (accessed 5 October 2021).. In apparent agreement with this approach, three MSF operational centres also intervened, mobilising 60 international and 106 national staff along with 60 tonnes of material Médecins Sans Frontières (2018), ‘Update: Ebola Outbreak in Equateur Province, DRC’, press release, 29 May, https://reliefweb.int/report/democratic-republic-congo/update-ebola-outbreak-equateur-province-drc-may-29-2018 (accessed 5 October 2021).to the remote rural province within the first three weeks of the response. Their ambition was no longer limited only to the relief of suffering, as MSF public communications now claimed that ‘with the correct intervention and careful monitoring of the situation, it is possible to limit the spread of the outbreak’ Médecins Sans Frontières (2018), ‘Update: Ebola Outbreak in Equateur Province, DRC’, press release, 29 May, https://reliefweb.int/report/democratic-republic-congo/update-ebola-outbreak-equateur-province-drc-may-29-2018 (accessed 5 October 2021).via the tracing and early isolation of people suspected to be suffering from the disease. These claims would not be proven in Equateur, however. Most of the fifty-four Ebola cases were identified in the ten days after the declaration of the epidemic WHO (2018), ‘Ebola Virus Disease: Democratic Republic of Congo. External Situation Report 17’, 25 July, http://apps.who.int/iris/bitstream/handle/10665/273348/SITREP_EVD_DRC_20180725-eng.pdf?utm_source=Newsweaver&utm_medium=email&utm_term=click+here+to+download+the+complete+situation+report&utm_content=Tag%3AAFRO%2FWHE%2FHIM+Outbreaks+Weekly&utm_campaign=WHO+AFRO+-+Situation+Report+-+Ebola+Virus+Disease+Outbreak+in+DRC+-+Declaration+of+End+of+Outbreak (accessed 5 October 2021)., before any real response activity had begun. Sixty per cent of them died, a fatality rate equivalent to previous epidemics in the DRC. Ebola vaccines were introduced only toward the end of the outbreak, once transmission had essentially already stopped. Still, when the epidemic was declared over, almost two months after the last new case had been identified, response actors claimed to have rapidly ‘controlled the outbreak’ under the leadership of the WHO and the Congolese Minister of Health, Dr Oly Ilunga Dowell, S. (2018), ‘The Democratic Republic of Congo Just Stopped a Killer Disease in Its Tracks. What’s Next?’, 31 July, www.gatesfoundation.org/ideas/articles/drc-stops-ebola-outbreak-lessons-learned-polio (accessed 5 October 2021).. Before any critical reflection could be initiated, attention moved to Nord Kivu.
First Phase of the Kivu Epidemic
Chasing after Cases
MSF had long been familiar with Nord Kivu, first intervening in the province in the early 1990s. During one reflection exercise held at MSF’s Paris headquarters, the consequences of operating in the region had been discussed, including the inevitable destabilisation of local health systems linked to the parallel payment of salaries and the provision of free care Brauman, R. (2017), ‘Should I Stay or Should I Go? Médecins Sans Frontières et les stratégies de sortie’, 2 May, http://msf-crash.org/fr/publications/acteurs-et-pratiques-humanitaires/should-i-stay-or-should-i-go-medecins-sans (accessed 5 October 2021).. The context of insecurity in Nord Kivu was also well understood by MSF. Four members of the association were abducted by an armed group near Beni in 2013; three of them have never been found Médecins Sans Frontières (2019), ‘Six Years on, Still No News of Our Colleagues Held Hostage by Armed Group ADF’, statement, 11 July, www.msf.org/six-years-still-no-news-our-colleagues-held-hostage-armed-group-adf-drc (accessed 5 October 2021).. Consequently, in early 2018 MSF France had decided not to intervene in Beni despite evidence of poor access to paediatric and surgical care in the town. Still, MSF was operational in six projects throughout the province when an Ebola outbreak was confirmed in Nord Kivu on 1 August 2018.
In late July, after hearing rumours that unexplained deaths had been occurring for months in Mangina, in the far north of Nord Kivu, members of the MSF Lubero project team accompanied local Ministry of Health and WHO staff to investigate. The rapid laboratory confirmation of Ebola virus in blood samples taken from four patients at the local health centre led to the declaration of the outbreak by the Ministry of Health. The MSF team, mainly comprised of local staff with little experience of Ebola, began installing an ad hoc setup within the health centre to provide care for those patients and any other sick people suspected to be suffering from the disease. A Congolese MSF logistician described it as a short and intense period of ‘constructive collaboration’, where MSF and local health staff worked long hours in difficult conditions to reorganise the existing facility. This locally focused approach would soon however change under the weight of a fast-growing national and international response.
The news of a new epidemic in the east of the country triggered the mass movement of Ministry of Health and WHO personnel from Equateur, Kinshasa and Geneva to Nord Kivu. Two days after the confirmation of the first cases, an Emergency Operations Centre (EOC) was installed in Beni, 30 km away from Mangina, under the coordination of a director from the national Ministry of Health and an incident manager from the WHO. Local health authorities from Nord Kivu province had little involvement in this coordination group. The EOC adopted technical and organisational protocols elaborated in West Africa and Equateur to develop the first Strategic Response Plan (SRP1), described by an MSF coordinator as a ‘copy-paste’ of the strategy used in Equateur.The primary response structure detailed in SRP1 consisted of eight ‘pillars’: surveillance (including contact tracing, points of entry and vaccination), laboratories, case management, communication and community engagement, psychosocial support, infection prevention and control (including safe and dignified burials), logistics and security. The initial aim was the rapid installation of the fundamentals of an ‘effective’ response following the template used in previous outbreaks (WHO (2019), WHO’s Response to the 2018–2019 Ebola Outbreak in North Kivu and Ituri, the Democratic Republic of the Congo. Report to donors for the period August 2018 – June 2019 (Geneva: WHO), www.who.int/docs/default-source/documents/emergencies/drc-ebola-response-srp-1-3-october2019.pdf?sfvrsn=41319fa1_2 (accessed 5 October 2021). An initial budget of $44 million was requested to cover three months of response activitiesCrawford, A. et al. (2021), The Democratic Republic of Congo’s 10th Ebola Response: Lessons on International Leadership and Coordination (London: ODI)..
As in Equateur, MSF also adopted the approach to ‘go big and go fast’. The day the Kivu epidemic was declared, after only four known cases, three MSF operational centres mobilised emergency teams to respond to the outbreak. Considered a ‘privileged partner’ due to MSF’s Ebola expertise as well as the fact that a team was already operational in Mangina, an MSF representative was invited to be part of the EOC taskforce coordinating the intervention from BeniMédecins Sans Frontières (2018), ‘New Ebola Outbreak Declared in North Kivu’, project update, 5 September, www.msf.org/new-ebola-outbreak-declared-north-kivu (accessed 5 October 2021).. This role was assumed by the Belgian section of MSF, which had the most experience in responding to Ebola outbreaks, thus putting them effectively in the lead of defining MSF’s actions. However, all sections initially agreed on the strategy elaborated in SRP1. When the Ministry of Health called for ‘partners’ to position themselves, MSF proposed to take the lead in case management, or the care of Ebola patients. The intention of this choice was not explicitly documented at the time, but in later interviews MSF staff described their ambitions as being ‘to relieve suffering’, ‘to save lives’ and ‘to control the epidemic’. Many considered that, as demonstrated in West Africa, only MSF had the necessary expertise and experience to achieve those aims. Some also noted MSF’s intention to be involved in the study of new treatments for Ebola, which would necessitate access to a cohort of Ebola patients and structures in which to implement the studies. Others recalled that during the initial planning meetings MSF coordinators had also requested to be involved in community ‘health promotion’ and vaccination activities, but this had been refused by the direction of the taskforce. According to one MSF staff member, ‘the WHO said they didn’t want partners to spread themselves too thinly, but really they didn’t want us to be seen as taking the lead’.
MSF quickly decided that the Mangina health centre was unsuitable for Ebola care, so began constructing a tented Ebola treatment facility nearby. Within two weeks MSF had equipped the structure, recruited and trained personnel and started receiving patients. However, when agreeing to offer ‘case management’ services, MSF coordinators had accepted that personnel would only be selected from lists provided by the Ministry of Health, who also determined the barème or salary scale that MSF would pay. MSF had also accepted to have no control over which patients would be admitted to the facility, agreeing to isolate and observe all ‘suspect’ cases brought to the centre by Ministry of Health and WHO surveillance teams, only allowing them to leave when two laboratory tests performed two days apart ruled out infection with the virus. MSF staff present at these early discussions recalled that there was little room to negotiate these points, noting that other NGOs had to abide by the same rules. However, it is unclear whether these ‘compromises’ were discussed more widely within the organisation, or whether the potential consequences were considered at the time.
The consequences soon became apparent, however. Opening with thirty beds, at a cost estimated by the MSF project coordinator at a million dollars, the Mangina Ebola centre was rapidly overwhelmed. Within days the capacity had to be increased to seventy beds to cope with the number of admissions. After an initial cluster of positive cases in the first month, most people brought to the centre tested negative for Ebola. Some were mildly unwell or not sick at all, others suffered from critical illnesses that the facility was not equipped to manage. Supportive care interventions in West Africa had been rudimentary due to the fear of occupational contamination of staff, and due to disagreements within MSF about the benefits of administering intravenous fluids for the disease. Intentions to develop new Ebola care protocols in Kivu were impeded by the wide range of pathologies and severity of illness of the patients, although from September all patients who did test positive for Ebola were offered an intravenous experimental curative treatment that the Congolese authorities had agreed could be administered in designated treatment centres via a ‘compassionate use’ protocol. Although not noted in MSF documents written at the time, in later interviews medical staff reported frustration at not being able to provide individualised supportive care such as blood transfusions, and a perception that in indiscriminately admitting everyone for testing they were acting more as ‘attendants in a laboratory waiting room’ than skilled doctors and nurses. They also compared the quality of care offered by MSF unfavourably to that provided by the NGO Alima, who had opened an Ebola treatment centre in Beni’s General Hospital and were contributing to the documentation of a new ‘paradigm’ of improved supportive care, which included the administration of intravenous fluids, blood transfusions and oxygen therapy as necessary to any patient with signs of critical illness, whether they eventually tested positive for Ebola or notFischer, W. A., Crozier, I., Bausch, D. G., Muyembe, J-J., Mulangu, S., Diaz, J. V., Kojan, R., Wohl, D. A. and Jacob, S. T. (2019), ‘Shifting the Paradigm – Applying Universal Standards of Care to Ebola Virus Disease’, New England Journal of Medicine, 380: 15, 1389– 91..
Although cases had remained circumscribed to a small area before the outbreak was detected, infected people soon began to leave Mangina and new ‘imported’ cases emerged in different locations across Grand Nord Kivu and neighbouring Ituri province. MSF, with its private funds and rapid access to resources, was quick to volunteer its services in each location where an infected person was found (Figure 1). In several areas an MSF team set up an Ebola unit, recruited and trained staff and began observing and testing patients, only to never receive another positive case. In some instances, MSF chose to close units again when there was no evidence of local disease transmission, so that equipment could be deployed elsewhere; in other locations Ministry of Health coordinators insisted the structure must remain open, ‘suspect’ cases continue to be admitted and staff continue to be paid. To free up operational capacity, MSF tried to hand some facilities over to other response actors, but as these actors first needed to confirm the availability of funds from the response budget, the handovers were often delayed. By November Ebola facilities were full of people suffering from malaria or complications of pregnancy, but over a third of the 400 Ebola cases had died ‘in the community’, mainly in local health structures, having never made it to a treatment facility at all (Aruna et al., 2019). According to an MSF nurse, it seemed like the organisation was trying to be everywhere but was still ‘never in the right place at the right time’.
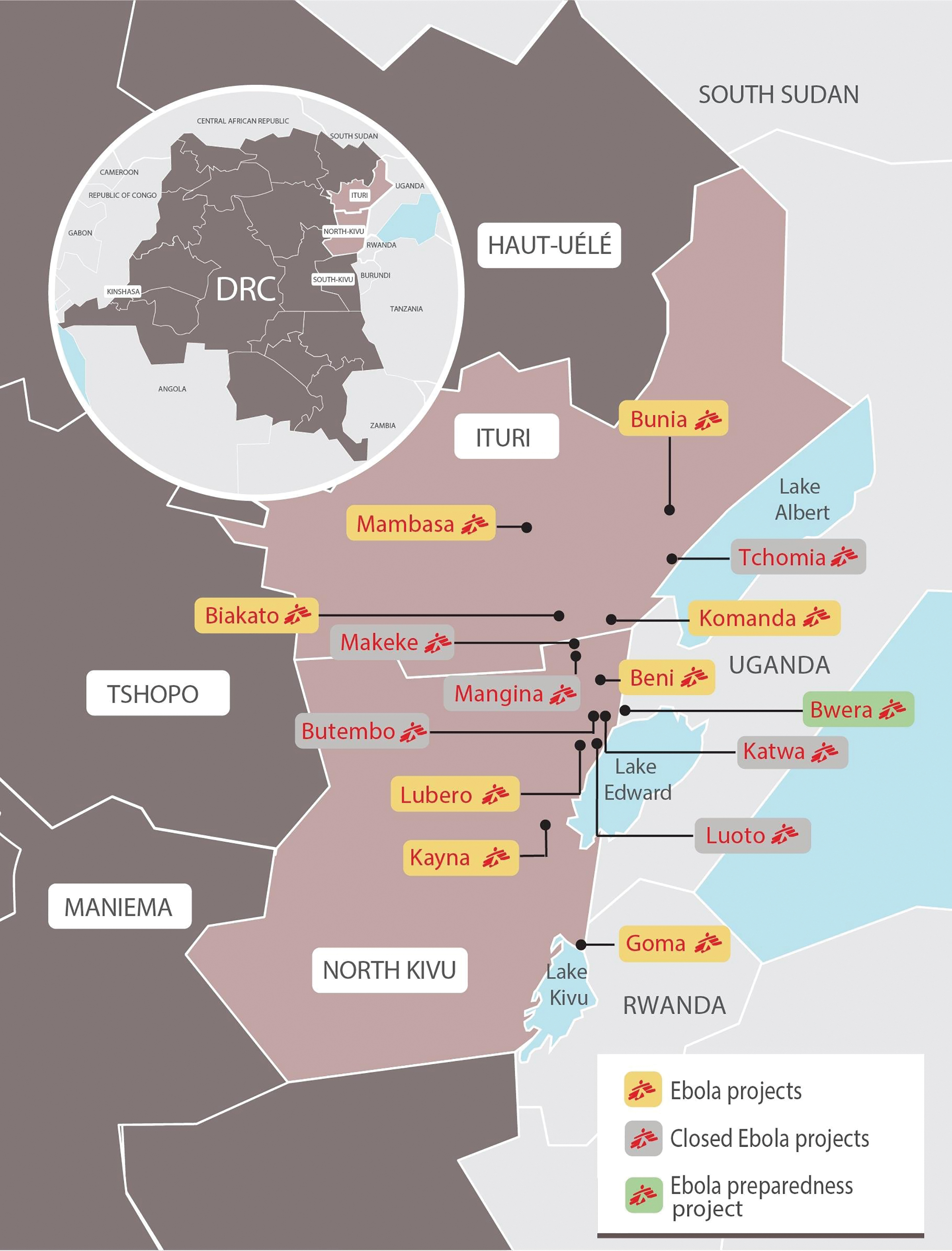
Figure 1: Map of MSF Ebola activities in Nord Kivu and Ituri provinces, August 2019.
Source: MSF, www.doctorswithoutborders.org/what-we-do/news-stories/story/ebola-outbreak-democratic-republic-congo-november-crisis-update.
Social and Political Tensions and Profits
Climbing infection and mortality figures were not the only indications of problems with the response. By the time I visited Nord Kivu in early 2019, Congolese MSF staff were openly alluding to endemic corruption in the ‘riposte’ – the name commonly given to the WHO and Ministry of Health-led Ebola response – particularly in recruitment practices, in car rentals and in vaccination activities. They complained about flagrant injustice and nepotism, remarking that an Ebola response worker’s salary, set by the national health authorities, was higher than that typically paid by international NGOs, and far higher than in the public health system. They also complained about corruption causing difficulties in accessing vaccination.
A Congolese MSF staff memberFirst discussion in Nord Kivu, March 2019; interviewed by telephone April 2020.described how he had heard of admission to MSF Ebola facilities being used as a form of punishment – for example, for people unable to pay fees at local health facilities. Just the threat of referral to an Ebola centre was an effective extortion tactic, as no-one wanted to be detained for three days in solitary isolation in a tent, where food was considered inadequate and where people died alone from diseases other than Ebola. He had also heard that local health workers, upset that Ebola centres provided free care and medicine to patients suffering from minor illnesses, were spreading rumours about foreign aid workers stealing organs; and that even people clearly suffering from Ebola could pay to avoid referral to a centre.
Political tensions around the epidemic were also rising, impacting the response efforts. On 26 December 2018 the Congolese President Joseph Kabila announced the suspension of presidential elections in Beni and Butembo, citing the risk of Ebola transmission occurring in polling stations. Opposition political leaders, suspecting this to be a political manoeuvre to deny people in areas known to be unfavourable to Kabila the right to vote, called for the local population to mobilise in protest. The protests, occurring the next day, quickly turned violent. An MSF centre built to triage ‘suspect’ Ebola patients in Beni was attacked by protesters Mohamed, H. (2018), ‘Protesters in DRC’s Beni Target Ebola Centre over Election Delay’, Al Jazeera, 27 December, www.aljazeera.com/news/2018/12/27/protesters-in-drcs-beni-target-ebola-centre-over-election-delay (accessed 5 October 2021)., and the patients and staff fled. MSF staff also recalled crowds trying to force entry into the hotel where they were staying before being dispersed by members of the Congolese armed forces, who fired live ammunition.
MSF Relations with the ‘Riposte’
MSF field reports and public communications from the first months of the outbreak reveal few signs of concern about the response strategy, although they note that the epidemic might not have been ‘under control’, possibly because patients ‘do not understand the importance of early hospitalisation and treatment’Médecins Sans Frontières (2018), ‘New Ebola Outbreak Declared in North Kivu’, project update, 5 September, www.msf.org/new-ebola-outbreak-declared-north-kivu (accessed 5 October 2021).. Rohan and McKayRohan, H. and McKay, G. (2020), ‘The Ebola Outbreak in the Democratic Republic of the Congo: Why There Is No “Silver Bullet”’, Nature Immunology, 21, 591–4, doi:10.1038/s41590-020-0675-8.attribute this failure to adjust the strategy to a phenomenon of ‘evidentiary inertia’, arguing that the size and complexity of the Kivu response prevented actors from adapting quickly to new evidence, due to ‘reasonable concerns about the logistical challenges of changing response-wide protocols as well as the belief that redesigning standard operating procedures and retraining staff would simply be too great a challenge’. Yet this assumes that practitioners recognised problems with the approach but decided that it was just too difficult to make changes. This is not apparent when reviewing MSF’s actions. The decision of the WHO not to declare the epidemic a Public Health Emergency of International Concern (PHEIC) passed without comment Butler, D. (2018), ‘WHO Says Africa’s Latest Ebola Outbreak Is Not an International Emergency’, Nature, 17 October, www.nature.com/articles/d41586-018-07116-3, https://doi.org/10.7227/JHA.017.. In October 2018 and January 2019 MSF coordinators were present during the elaboration of further governmental strategic response plans (SRP2 and SRP3), essentially unchanged from SRP1 but calling for budget increases of $61 million and $147 million respectively Crawford, A. et al. (2021), The Democratic Republic of Congo’s 10th Ebola Response: Lessons on International Leadership and Coordination (London: ODI).. Only the institutional donors to the response efforts remarked that the epidemic seemed to be accelerating despite the resources being deployed to contain it, and that they ‘did not perceive the SRP3 to be a viable basis for issuing funding’ Independent Oversight and Advisory Committee [IOAC] for the WHO Health Emergencies Programme (2019), IOAC Mission Report. Democratic Republic of the Congo 24 April–2 May 2019 (Geneva: WHO), www.who.int/about/who_reform/emergency-capacities/Mission-Report(English).pdf?ua=1 (accessed 5 October 2021).. However, the funds were still allocated, and as described by a non-MSF practitioner involved in the response, ‘the solution endorsed by everyone seemed to be to just throw more money at the problem’.
When disagreements occurred between MSF and the Congolese authorities at the Beni EOC meetings during this period, they were not over the strategy. In November 2018, MSF, looking to be involved in implementing studies of experimental treatments under the direction of the Congolese national research institute, requested to open a second Ebola treatment centre in Beni, then the epicentre of the epidemic. The EOC response coordinator refused, noting the existence of another facility managed by Alima. He authorised only a ‘transit’ centre where patients could be tested and receive supportive care but must be referred to the Alima facility for any Ebola treatment. MSF agreed to open the ‘transit’ centre, but an MSF coordinator, frustrated at having failed to negotiate access to Ebola patients, complained that MSF had been ‘blocked’ by the Congolese authorities and did not have enough ‘space’ in the response.
The next disagreement with the Congolese authorities was more dramatic. Early in February 2019 armed members of the police arrived at the Butembo MSF Ebola centre with a patient for admission. Displaying no signs or symptoms of Ebola, this person had apparently been beaten, but the MSF team still admitted him for testing. Once it was confirmed he was negative for the disease, MSF coordinators addressed a letter to the Minister of Health complaining about the use of excessive force. A member of MSF France staff described the subsequent taskforce meeting in Beni, where the Congolese EOC response coordinator, furious at the letter, accused MSF of undermining Congolese efforts to control the epidemic, while also reminding all partners that the Ministry of Health held no responsibility for the behaviour of the Congolese armed forces or police.
In Europe differences of opinion did arise between MSF Operational Centres about the choice of activities and the practical details of their implementation, leading to a decision in January 2019 that MSF Belgium would no longer be the lead for the organisation in Beni, and that each responding MSF section would determine and negotiate their own strategy Médecins Sans Frontières (2019), ‘Intersectional meeting/review on the Ebola epidemic strategy and operational response of MSF in DRC’. Internal document.. However, this decision resulted in little immediate change in MSF’s activity or in its relationships with the ‘riposte’. By late February 2019 an average of thirty new cases were being identified each week throughout the Grand Nord, with hotspots in Beni and Butembo. MSF continued running Ebola-related interventions across the region, paying incentives to hundreds of staff and attending the Ministry’s daily taskforce meetings, with apparently few premonitions of what was about to happen.
Attacks and Fallout
On the night of the 24 February 2019, during a visit to Nord Kivu by Joanne Liu, then MSF International President, an MSF Ebola treatment centre in Katwa was attacked by armed men, and the structure set alight. The staff and patients fled. Three nights later, a second MSF centre a few kilometres away in Butembo was also attacked and burnt Médecins Sans Frontières (2019), ‘Medical Activities Suspended after Ebola Treatment Centre Attack’, statement, 28 February, www.msf.org/medical-activities-suspended-after-ebola-treatment-centre-attack (accessed 5 October 2021).. All MSF activities in Butembo and Katwa were immediately suspended, and international staff evacuated. Liu met with the Congolese Health Minister in Kinshasa to explain that the organisation would not return to Butembo or Katwa until the cause of the attacks could be verified. At the time Liu described the conversation as ‘cordial’, with the Minister thanking her for MSF’s ongoing support of response efforts.
A press conference was held in Geneva on 7 March, where Liu announced the withdrawal from Butembo and read a statement claiming that despite the availability of treatments and vaccines, the epidemic was out of control Médecins Sans Frontières (2019), ‘Ebola Response Failing to Gain the Upper Hand on the Epidemic’, press release, 7 March, www.msf.org/ebola-response-failing-gain-upper-hand-epidemic-democratic-republic-congo (accessed 5 October 2021).. Linking the attacks on MSF centres to ‘various political, social and economic grievances [that] are increasingly crystallising around the response’ she noted as contributing factors the massive deployment of financial resources in a ‘neglected’ region affected by conflict and violence and where the population suffered from long-standing health needs, the cancellation of the elections and the coercive practices of the armed forces and police. The statement positioned MSF as a ‘patient and community centred’ organisation, calling for patients to be ‘treated as patients, and not as some kind of biothreat’. Resulting press reports focused on the ‘militarisation’ of the response Miles, T. (2019), ‘Battle against Ebola Being Lost Amid Militarized Response, MSF Says’, Reuters, 7 March, www.reuters.com/article/us-health-ebola-congo-idUSKCN1QO1F1 (accessed 5 October 2021)., with several implying that MSF had withdrawn from all Ebola activities in the DRC in protest.
The Minister of Health, enraged over the press conference, immediately announced that MSF was no longer authorised to intervene in Butembo or Katwa until further discussions were held in Kinshasa. A spokesperson for the ministry noted to the press that MSF appeared ‘confused’ about the role of security forces, explaining that these forces operate under the control of the Interior Ministry and not the Ministry of Health, and had only been deployed to ‘protect health officials and facilities, and to guarantee the security of response workers’, just as MSF was demanding Miles, T. (2019), ‘Battle against Ebola Being Lost Amid Militarized Response, MSF Says’, Reuters, 7 March, www.reuters.com/article/us-health-ebola-congo-idUSKCN1QO1F1 (accessed 5 October 2021)..
Following the press conference, confusion reigned in eastern DRC, where Ebola-related MSF activities continued to the north and south of Butembo. Visiting the region at the time, I was inundated with questions from Congolese colleagues about whether all MSF Ebola activities would be stopped. Some noted a contradiction in MSF claiming to be primarily concerned for patients while simultaneously withdrawing from the epicentre of the outbreak and questioned whether MSF was abandoning the population of Butembo on a matter of moral principle. The Ebola treatment centre in Butembo was reopened by Ministry of Health staff, now operating under the direct supervision of the WHO, using funds mobilised from the overall response budget. MSF staff recalled that the ‘riposte’ returned quickly to ‘business as usual’, and that some representatives of the WHO, so heavily criticised by MSF in West Africa, pointed out with a note of triumphalism that the tables had turned. This time it was the WHO that was directly operational in all elements of the Ebola response, and MSF that was confined to the margins. Liu’s observation that the epidemic was ‘out of control’ was overlooked.
Second Phase: Life on the Periphery
A ‘New’ Response Coordination
The MSF withdrawal from Butembo coincided with a reorganisation of the response, if not the strategy. From March 2019 the Ministry of Health established a new Ebola response coordination committee in Goma, inviting representatives of institutional donors and key UN organisations. Although the Minister was still furious at MSF’s withdrawal from Butembo, and some WHO staff continued to remark on MSF’s lack of pertinent contribution to the Ebola response, MSF was also invited to join. The invitation was accepted. Despite the agreement for each to pursue their own operational strategy, the MSF operational centres involved in the Ebola response nominated a shared representative to the committee, tasked with following updates, reporting on MSF activities and negotiating with the ‘riposte’.
The information presented at the daily meetings of this committee revealed an increasingly catastrophic situation. By May the number of new infections climbed to reach a peak of 120 each week, mainly localised around the densely populated urban zones of Butembo and Katwa. Vaccination teams, moving with armed escorts, were regularly attacked, as were peripheral health facilities Congo Research Group (CRG) (2021), Rebels, Doctors and Merchants of Violence: How the Fight against Ebola Became Part of the Conflict in Eastern DRC’ (New York: Congo Research Group/Center on International Cooperation).. Several local workers were killed, and on 19 April armed men assassinated the WHO epidemiologist Dr Richard Mouzoko Kiboung in Butembo WHO (2019), ‘WHO Ebola Responder Killed in Attack on the Butembo Hospital’, statement, 19 April, www.who.int/news/item/19-04-2019-who-ebola-responder-killed-in-attack-on-the-butembo-hospital (accessed 5 October 2021).. Yet the level of catastrophe was not publicly acknowledged by the authorities in charge of the ‘riposte’. In April 2019, a group tasked with independent oversight of the WHO Emergencies Programme visited DRC and noted ‘the absence of an effective forum for identifying, reviewing, and resolving shortcomings in response effectiveness’ Independent Oversight and Advisory Committee [IOAC] for the WHO Health Emergencies Programme (2019), IOAC Mission Report. Democratic Republic of the Congo 24 April–2 May 2019 (Geneva: WHO), www.who.int/about/who_reform/emergency-capacities/Mission-Report(English).pdf?ua=1 (accessed 5 October 2021).; but in the same month a committee of experts convened by the WHO reviewed the epidemic situation and again decided that it did not justify the declaration of a PHEIC. According to the chairman of this committee, they remained optimistic that ‘this outbreak can be brought under control’ Green, A. (2019), ‘DR Congo Ebola Outbreak Not Given PHEIC Designation’, The Lancet, 393: 10181, 1586, doi: 10.1016/S0140-6736(19)30893-1.. This time, MSF representatives did criticise the decision in The Lancet Green, A. (2019), ‘DR Congo Ebola Outbreak Not Given PHEIC Designation’, The Lancet, 393: 10181, 1586, doi: 10.1016/S0140-6736(19)30893-1., arguing that although more resources were not required, a PHEIC declaration would raise important questions about the response strategy and force a re-evaluation and adjustment of the approach.
Attempts to Reorient MSF Operations
Meanwhile, MSF had little to report at coordination meetings. No longer present in the disease epicentre and with no Ebola treatment centre in which to offer care, the organisation was forced to reconsider its operations. MSF Belgium, whose main activity had been at the Katwa centre, temporarily withdrew from the Ebola response. MSF Switzerland, who had been running the Butembo centre, pulled back from Nord Kivu to focus on Ituri province. MSF France did not have so much choice. Days after the February attacks a patient died of Ebola in Lubero hospital, where an MSF France team was already supporting general medical activities. The Médecin Chef de Zone, the head of the local health authorities in the area, approached the MSF project coordinator to request support. Explaining that he had lost many staff to better paid Ebola response jobs, he suggested that MSF help reorganise and equip the existing health structure, rather than construct a separate Ebola centre. In return for intervening more widely in the hospital, he would grant the MSF team the authority to determine which patients would be tested for Ebola, as well to make decisions over recruitment, training and the salaries of hospital staff, in collaboration with the hospital management. The MSF project coordinator agreed.
Although the number of Ebola patients in Lubero remained low, members of the MSF France team used the experience to elaborate a new strategy Médecins Sans Frontières (2019), ‘Stratégie générale Urgence Grand Nord Kivu dans un contexte Ebola’. Internal document., working from a hypothesis that by integrating MSF staff into health structures routinely used by the local population, MSF could make earlier and more precise clinical diagnoses of Ebola, facilitating earlier targeted treatment and supportive care and thus reducing mortality. Still unauthorised to work in Butembo or Katwa, MSF teams approached the local health authorities in Beni to offer support to selected health facilities. An MSF coordinator recounted that most local interlocutors were rapidly convinced by the proposal, particularly when it was accompanied by an offer of material and financial support which until then had been distributed only via the ‘riposte’. Yet although these arguments persuaded local authorities, they foundered when they were put to the response hierarchy.
A False Independence
In the months following the attacks, putting new operational intentions into action proved difficult, as MSF struggled to convince the authorities in charge of the Ebola response. Encouraged by the enthusiasm of local health authorities for MSF support to existing facilities, some MSF France managers had begun claiming that they had found a way to operate ‘independently’ from the ‘riposte’. However, as the national Ministry of Health and WHO were the official leads of the Ebola response, authorisation for any new activity was still required from the response coordination in Goma. MSF staff described a game of ‘cat and mouse’, where they would agree activities with local health authorities, then draft a Memorandum of Understanding (MOU) to submit to the Congolese response coordinator. The standardised MOU format requested that the Congolese Ministry of Health respect the MSF charter and principles. The response coordinator, happy to have his claims that MSF was uncooperative justified by this use of authoritative legal documentation, routinely refused to sign. On some occasions, the MSF team launched the activity anyway, without waiting for a green light from the ‘riposte’. On others, the lack of official approval deterred MSF staff who were already reluctant to let go of familiar practices and protocols. In one location, the local authorities withdrew their support and asked MSF to leave the area.
From February 2019 MSF France also attempted to become involved in Ebola vaccination, including via public communications calling for a rapid increase in vaccination coverage of the at-risk population Médecins Sans Frontières (2019), ‘Not Contained, New Cases: Three Questions on Vaccines and the Ebola Outbreak in DRC’, interview, 31 July, www.msf.org/not-contained-new-cases-three-questions-vaccines-and-ebola-outbreak-drc-democratic-republic-congo (accessed 5 October 2021).. However, although at the beginning of the outbreak MSF had been allowed to vaccinate selected frontline workers, all offers to support Ebola vaccination in DRC were now refused by the WHO team leading the activity, who claimed that MSF would not respect the ‘study’ protocols for use of the vaccine. Looking for alternative options, MSF France and Epicentre, an MSF satellite organisation dedicated to epidemiology and research, agreed in April 2019 to support a clinical trial of a second Ebola vaccine, as part of a team led by the Congolese national research institute, the INRB (Institut National de Recherche Biomédicale). I was based in Goma from April until September 2019 to coordinate MSF France’s involvement in the study.
The attempts to introduce a second vaccine were however also impeded by a lack of official approval. Funding and scientific and ethical approval had been quickly obtained for the study, but although the proposal was instigated by a Congolese state institute, the INRB, it was not endorsed by the ‘riposte’. This seemed less related to the vaccine itself and more to animosity between the Minister of Health and Professor Muyembe, the Director of the INRB. In April 2019, Muyembe had produced a scathing analysis of the response, accusing the health ministry of ‘weak governance and a leadership deficit’ Kupferschmidt, K. (2019), ‘Ebola Veteran Promises an End to Congo’s Epidemic’, Science, 6 August, doi: 10.1126/science.aaz0268., and proposing a new strategy and leadership that would include the greater implication of local authorities and of state institutions beyond the Ministry of Health. As for the vaccine, although its introduction had been recommended by a WHO advisory panel, some in the WHO perceived a risk of interference with ongoing studies of the first vaccine BBC (2019), ‘Ebola Vaccine: Why Is a New Jab so Controversial?’, BBC News, 4 August, www.bbc.com/news/world-africa-49164066 (accessed 5 October 2021).. The Congolese Health Minister claimed that the use of a second vaccine would ‘confuse’ the local population Kupferschmidt, K. (2019), ‘Ebola Veteran Promises an End to Congo’s Epidemic’, Science, 6 August, doi: 10.1126/science.aaz0268.. Made nervous by controversy around the study in the media, and worried about becoming involved in a clash between Muyembe and the Health Minister, MSF coordinators in DRC were reluctant to engage in discussion with the ‘riposte’ about Ebola vaccination, preferring that a small group of MSF France and Epicentre staff handle all negotiations separately. The Minister of Health did give approval for the study in June 2019 Nakkazi, E. (2019), ‘Apply to Trial Ebola Vaccines in DR Congo, Says Ministry’, The Lancet, 6 July, doi: 10.1016/S0140-6736(19)31524-7.but retracted it shortly afterwards Branswell, H. (2019), ‘Debate over Whether to Test a Second Ebola Vaccine Turns Acrimonious’, STAT, 17 July, www.statnews.com/2019/07/17/debate-testing-second-ebola-vaccine/ (accessed 5 October 2021).. In July, the President of MSF France wrote to the Minister and the Director General of the WHO to express concern about the vaccination strategy, but did not receive a reply. In September, believing that the population’s access to protective vaccines was still insufficient a year after the epidemic had begun, MSF issued a press release accusing the WHO of a lack of transparency in the management of Ebola vaccination in the DRC Médecins Sans Frontières (2019), ‘Independent Ebola Vaccination Committee Is Needed to Overcome Lack of WHO Transparency’, press release, 23 September, www.msf.org/ebola-drc-independent-ebola-vaccination-committee-needed (accessed 5 October 2021)..
Third Phase: The Donors Take Control
In June 2019, although MSF activities remained limited, the organisation was present once again for the drafting of a fourth Strategic Response Plan (SRP4), which was associated with a tripling of the budget; $540 million was now requested to fund six further months of response interventions Crawford, A. et al. (2021), The Democratic Republic of Congo’s 10th Ebola Response: Lessons on International Leadership and Coordination (London: ODI).. The request was finally refused by donors unwilling to commit to any further funding until there was a re-evaluation of the strategy and clearer accountability for the money that had already been allocated to the response Crawford, A. et al. (2021), The Democratic Republic of Congo’s 10th Ebola Response: Lessons on International Leadership and Coordination (London: ODI).. This decision provoked major repercussions. In a first public display of division between the WHO and the Congolese health ministry, a PHEIC was declared on 17 July 2019 Maxmen, A. (2019), ‘Ebola Outbreak Declared an International Public-Health Emergency’, Nature, 17 July, doi: 10.1038/d41586-019-02221-3.. The following day the Congolese president Félix Tshisekedi announced that he was placing the leadership of the Ebola response directly under his authority, nominating Professor Muyembe to head up the response efforts. In protest, Oly Ilunga resigned from his post as Minister of Health. He was later imprisoned for embezzlement of Ebola funds Cohen, J. (2019), ‘Congo Arrests Former Health Minister for Alleged Misuse of Ebola Funds’, Science, 16 September, doi: 1126/science.aaz5248, www.sciencemag.org/news/2019/09/congo-arrests-former-health-minister-alleged-misuse-ebola-funds, doi: 10.7227/JHA.017..
By August 2019, a new leadership was in place, a new strategic response plan had been drafted and donors, reassured by Muyembe’s forecast that the epidemic would be over within months Kupferschmidt, K. (2019), ‘Ebola Veteran Promises an End to Congo’s Epidemic’, Science, 6 August, doi: 10.1126/science.aaz0268., approved the requested budget. Partly due to mutual understandings developed during the planning of the vaccine study, and partly due to Muyembe’s inclusion of local authorities into the coordination of the response, MSF negotiations with the new leadership were more fruitful. Activities in support of local health facilities were finally officially approved, and the ‘integrated’ model was eventually considered a success Park, S-J., Morisho, N., Muhindo, K. W., Anoko, J., Gobat, N., Brown, H. and Borchert, M. (2020), ‘What Do Adaptations Tell Us about the Production of Trust? Shifting the “Burden of Change” from People to the Response’, Humanitarian Exchange, Number 77: Special Feature – Responding to Ebola in the Democratic Republic of Congo, https://odihpn.org/wp-content/uploads/2020/03/HE-77-web.pdf (accessed 5 October 2021).. MSF France was authorised to take over the running of the Beni Ebola treatment centre in September 2019 and so began again providing care to Ebola patients, this time adopting protocols put in place by Alima. The study of the second Ebola vaccine began in November 2019, with MSF support. However, the new response coordinator, Professor Ahuka of the INRB, also complained about MSF’s insistence on the signature of MOUs for each new activity, noting that he preferred to engage in collective discussion about the approach rather than be presented with lengthy documents that left little room for debate.
From September 2019 cases began to decline, dropping to under ten new Ebola infections a week by the end of the year, although the epidemic was not finally declared over until June 2020. Over nearly two years, 3,470 people were infected with Ebola and 2,280 of them died, a static mortality rate of 65 per cent, roughly the same as in previous Congolese Ebola epidemics. It is estimated that between $800 million and $1.2 billion was spent on the response Crawford, A. et al. (2021), The Democratic Republic of Congo’s 10th Ebola Response: Lessons on International Leadership and Coordination (London: ODI)..
Discussion
Perceptions of success and failure are inherently subjective. The response to the West African Ebola outbreak was considered a success for MSF; the response in Nord Kivu a failure for everyone involved. Yet even if the results in Nord Kivu would appear as good as in West Africa, if not better – fewer frontline staff infected, in fact, fewer cases overall and therefore fewer deaths – a comparison between the two epidemics is not helpful. Although actions of response actors in DRC were usually well intentioned, and the funds and resources provided were more than adequate, the Kivu response efforts could rarely be described as lifesaving, may have just as well exacerbated transmission of the disease as limited it, and had the perverse effect of fuelling corruption and violence.
This medical and social failure of the Kivu response can be attributed to an initial belief by the response leadership, including MSF, in a strategy that had never been proven to work, and which had been designed at a time when the only realistically attainable outcome was to relieve suffering. Despite early evidence of failure, it took three attacks on MSF-led structures for the organisation to mount a challenge to this strategy, which, as it was established on moral indignation and not on medical or operational reasoning, could be easily discounted as frustration at having been confined to the periphery of the response. In a context of apparently unlimited funding and with a multitude of actors willing to take its place, MSF’s withdrawal from Butembo, and therefore effectively from the response, had few repercussions.
When MSF did try to reorient its actions, the organisation’s proposals failed to convince the authorities in charge of the response. Although negotiations may have anyway been futile, given the entrenched corruption and the unwillingness of the authorities to acknowledge failure, MSF’s position vis-à-vis the response leadership was perpetually contradictory. While claiming to want independence from the ‘riposte’, MSF continued to participate in the coordination of the response strategy and to demand official approval for each new activity. Neither completely assuming a confrontational attitude with the national authorities and the WHO, nor a political role aiming to influence the direction of the response via relations with those in power, MSF chose to ally with local authorities who were excluded from the coordination of the response rather than join forces with the institutions that had the greatest influence, the donors, who were looking for a convincing alternative strategy and leadership to support. MSF did however probably contribute unintentionally to changes in the response leadership via support to a ‘controversial’ vaccine study.
So, what about the future? Returning to the debates that occurred prior to 2013, why should MSF continue to intervene in Ebola if the association’s actions are so unlikely to improve the situation and risk contributing to making it worse? Fundamentally, because there is now actually a chance of success. For the first time, new ‘gamechanger’ products are available, including vaccines to protect people that may encounter the disease and monoclonal antibody treatments that effectively neutralise the virus. The ambition to establish a new, effective, approach to Ebola is finally attainable; it should now be possible to develop strategies that make the best use of these products and incorporate both new knowledge about the disease and a better comprehension of the social and political circumstances in the places where Ebola epidemics occur. To not grasp this opportunity would be a failure. But to elaborate any new public health policy, the national and international authorities that will oversee future Ebola responses must also be convinced. It is not yet certain how Ebola activities in the DRC will be run, or how they will be funded, but it is definite that epidemics will continue to occur in the country. There have already been three since the Kivu epidemic ended in 2020. MSF must not wait until the next major outbreak and then attempt to impose a new strategy, or worse, attempt to recreate the old one. To avoid future failure, any new approach must be built via collective discussion with the Congolese and international institutions that will be involved in executing the response, and MSF must agree to share in the responsibility for the outcomes.
To cite this content :
Natalie Roberts, “MSF and Ebola in Nord Kivu. Positioning, Politics and Pertinence”, 4 novembre 2022, URL : https://msf-crash.org/en/medicine-and-public-health/msf-and-ebola-nord-kivu-positioning-politics-and-pertinence
If you want to criticize or develop this content, you can find us on twitter or directly on our site.
Contribute



